Scarlet fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever is a clinical syndrome consisting of streptococcal pharyngitis Streptococcal Pharyngitis Rheumatic Fever accompanied by fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever and a characteristic rash Rash Rocky Mountain Spotted Fever caused by pyrogenic exotoxins Exotoxins Toxins produced, especially by bacterial or fungal cells, and released into the culture medium or environment. Bacteriology. Scarlet fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever is a non-suppurative complication of streptococcal infection that is more commonly seen in children. Incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency peaks during the winter Winter Pityriasis Rosea and spring in temperate climates. The rash Rash Rocky Mountain Spotted Fever begins in the 1st 24–48 hours of illness. Starting in the face or neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess, the exanthem Exanthem Diseases in which skin eruptions or rashes are a prominent manifestation. Classically, six such diseases were described with similar rashes; they were numbered in the order in which they were reported. Only the fourth (Duke's disease), fifth (erythema infectiosum), and sixth (exanthema subitum) numeric designations survive as occasional synonyms in current terminology. Varicella-Zoster Virus/Chickenpox spreads to the trunk and extremities but spares the palms and soles. With the infection, the face looks flushed, accompanied by circumoral pallor and a strawberry tongue Strawberry tongue Kawasaki Disease (enlarged papillae Papillae Lips and Tongue: Anatomy). The minute papules feel like sandpaper. Diagnosis is usually made clinically, confirmed with a rapid antigen detection Antigen detection Respiratory Syncytial Virus test (RADT) or throat Throat The pharynx is a component of the digestive system that lies posterior to the nasal cavity, oral cavity, and larynx. The pharynx can be divided into the oropharynx, nasopharynx, and laryngopharynx. Pharyngeal muscles play an integral role in vital processes such as breathing, swallowing, and speaking. Pharynx: Anatomy culture. Treatment is with penicillin Penicillin Rheumatic Fever or amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins.
Last updated: Feb 11, 2025
Scarlet fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever (also called “scarlatina”) is a diffuse erythematous eruption or rash Rash Rocky Mountain Spotted Fever that occurs in association with pharyngitis Pharyngitis Pharyngitis is an inflammation of the back of the throat (pharynx). Pharyngitis is usually caused by an upper respiratory tract infection, which is viral in most cases. It typically results in a sore throat and fever. Other symptoms may include a runny nose, cough, headache, and hoarseness. Pharyngitis.

Streptococcus pyogenes (GAS)
Image: “Photomicrograph of Streptococcus pyogenes bacteria” by the Centers for Disease Control and Prevention. License: Public domain.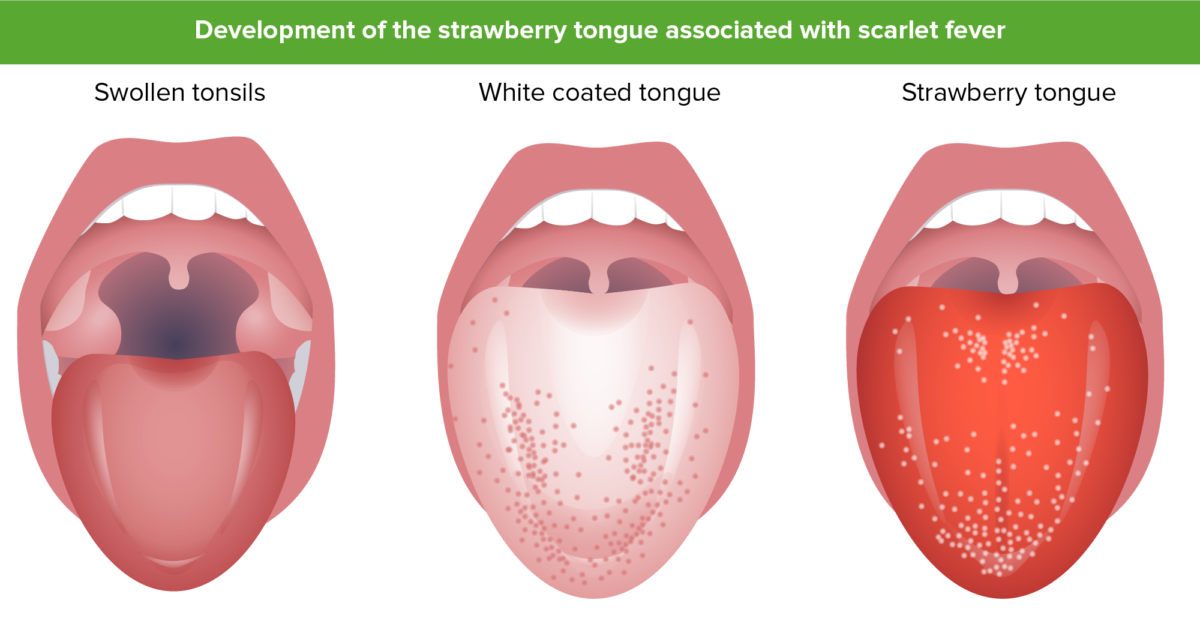
“Strawberry tongue”: early in the disease, the tongue could be covered by a white membrane or coating through which the papillae are seen. This layer sloughs off and reveals a bright red tongue with prominent papillae. A strawberry tongue results from a general inflammatory response early in the course of the disease.
Image by Lecturio.
Face looks flushed but has a “white mustache” or circumoral pallor, typical of scarlet fever.
Image: “Slapped cheeks and white mustache” by Estreya. License: CC BY-SA 4.0.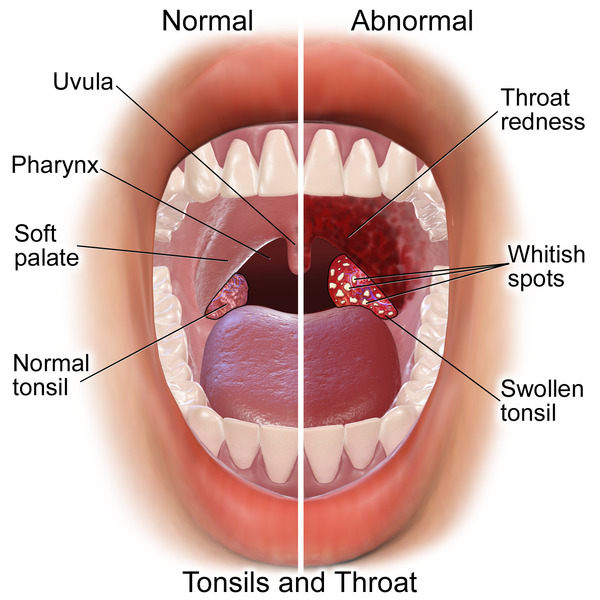
Common physical examination findings in acute exudative pharyngitis/tonsillitis (right half of the image), of which 1 of the most common causes is Streptococcus pyogenes
Image: “Tonsillitis” by BruceBlaus. License: Public domain.Management consists of treating the causative agent of pharyngitis Pharyngitis Pharyngitis is an inflammation of the back of the throat (pharynx). Pharyngitis is usually caused by an upper respiratory tract infection, which is viral in most cases. It typically results in a sore throat and fever. Other symptoms may include a runny nose, cough, headache, and hoarseness. Pharyngitis, Streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus pyogenes.
| Number | Other names for the disease | Etiology | Description |
|---|---|---|---|
| 1st disease 1st disease Measles (also known as rubeola) is caused by a single-stranded, linear, negative-sense RNA virus of the family Paramyxoviridae. It is highly contagious and spreads by respiratory droplets or direct-contact transmission from an infected person. Typically a disease of childhood, measles classically starts with cough, coryza, and conjunctivitis, followed by a maculopapular rash. Measles Virus |
|
Measles Measles Measles (also known as rubeola) is caused by a single-stranded, linear, negative-sense RNA virus of the family Paramyxoviridae. It is highly contagious and spreads by respiratory droplets or direct-contact transmission from an infected person. Typically a disease of childhood, measles classically starts with cough, coryza, and conjunctivitis, followed by a maculopapular rash. Measles Virus morbillivirus Morbillivirus A genus of the family paramyxoviridae (subfamily paramyxovirinae) where the virions of most members have hemagglutinin but not neuraminidase activity. All members produce both cytoplasmic and intranuclear inclusion bodies. Measles virus is the type species. Measles Virus |
|
| 2nd disease |
|
Streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus pyogenes |
|
| 3rd disease 3rd disease An acute infectious disease caused by the rubella virus. The virus enters the respiratory tract via airborne droplet and spreads to the lymphatic system. Rubella Virus |
|
Rubella Rubella An acute infectious disease caused by the rubella virus. The virus enters the respiratory tract via airborne droplet and spreads to the lymphatic system. Rubella Virus virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology |
|
| 4th disease |
|
Due to Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess strains that make epidermolytic (exfoliative) toxin |
|
| 5th disease | Erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion infectiosum | Erythrovirus or parvovirus B19 Parvovirus B19 Primate erythroparvovirus 1 (generally referred to as parvovirus B19, B19 virus, or sometimes erythrovirus B19) ranks among the smallest DNA viruses. Parvovirus B19 is of the family Parvoviridae and genus Erythrovirus. In immunocompetent humans, parvovirus B19 classically results in erythema infectiosum (5th disease) or “slapped cheek syndrome.” Parvovirus B19 (Primate erythroparvovirus Erythroparvovirus Parvovirus B19 1) |
|
| 6th disease |
|
Human herpesvirus 6B or human herpesvirus 7 |
|