Take your anatomy class online
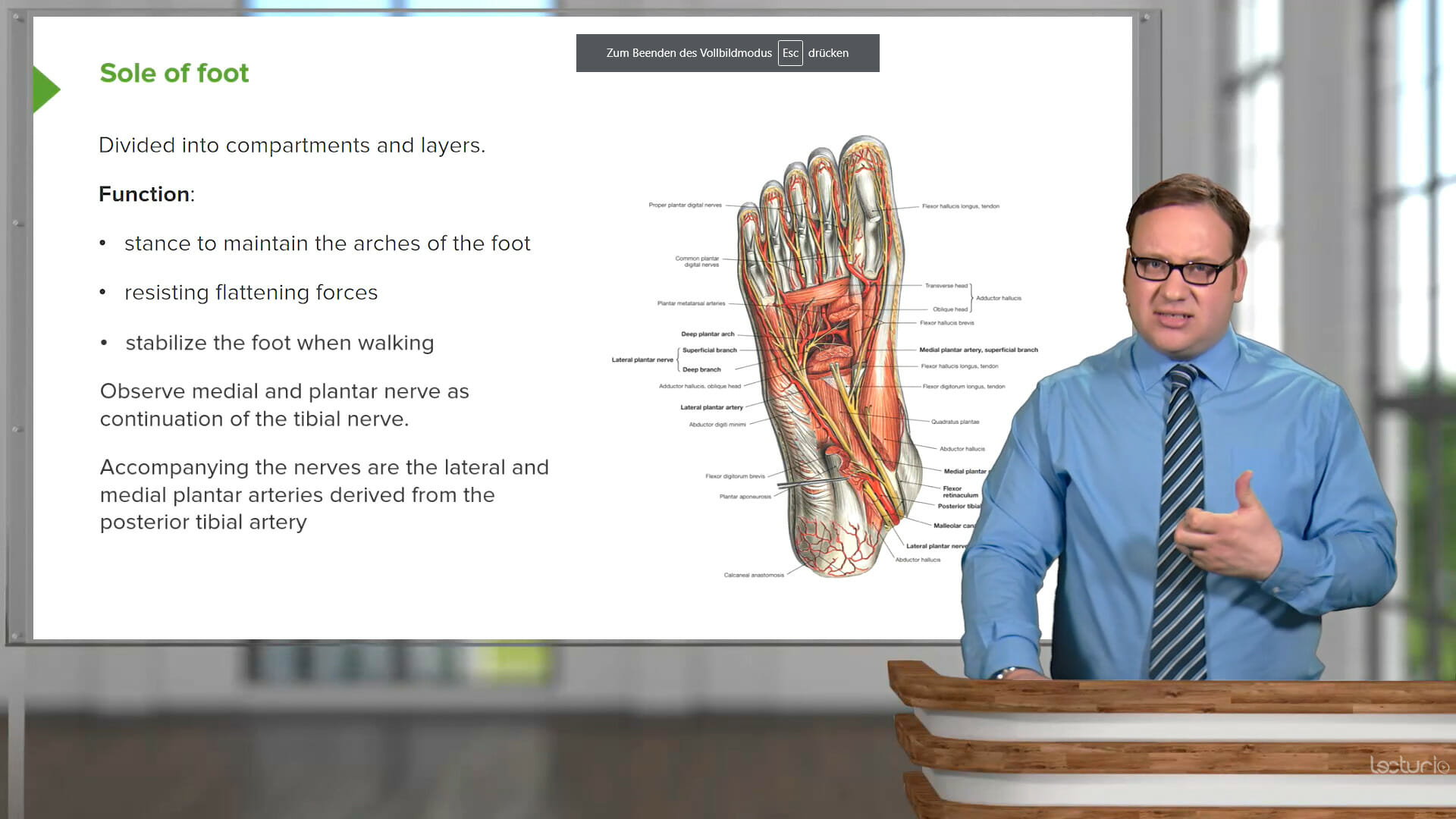
with James Pickering, PhD from UOL, Darren Salmi, MD, MS from Stanford University, and Craig Canby, PhD from DMU
“You must learn the normal before you can recognize the abnormal:” Knowing how the body is structured and composed is a key prerequisite for understanding its functions and all pathologies. The complexity, terminology, and vast amount of information is overwhelming for many students.
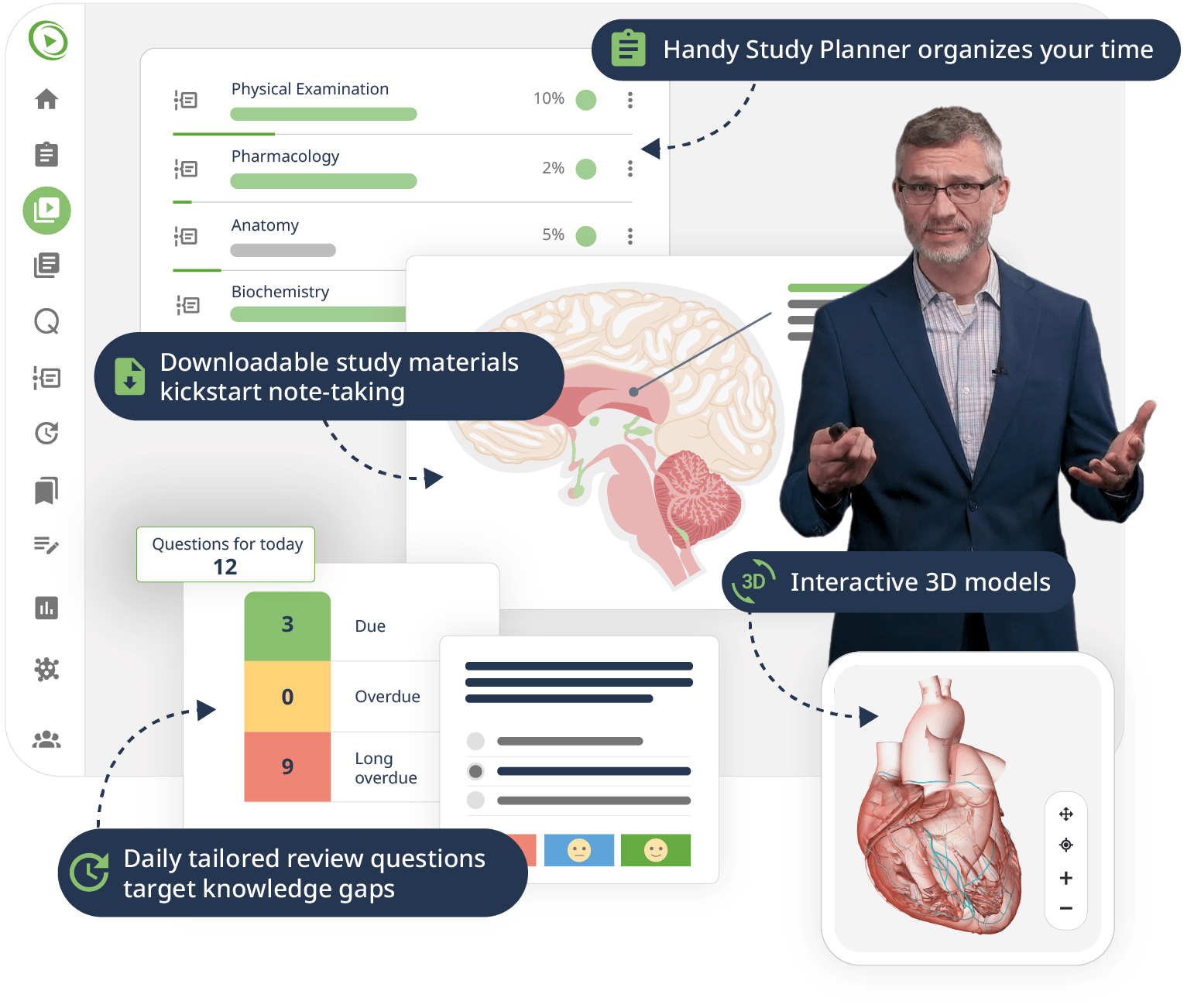
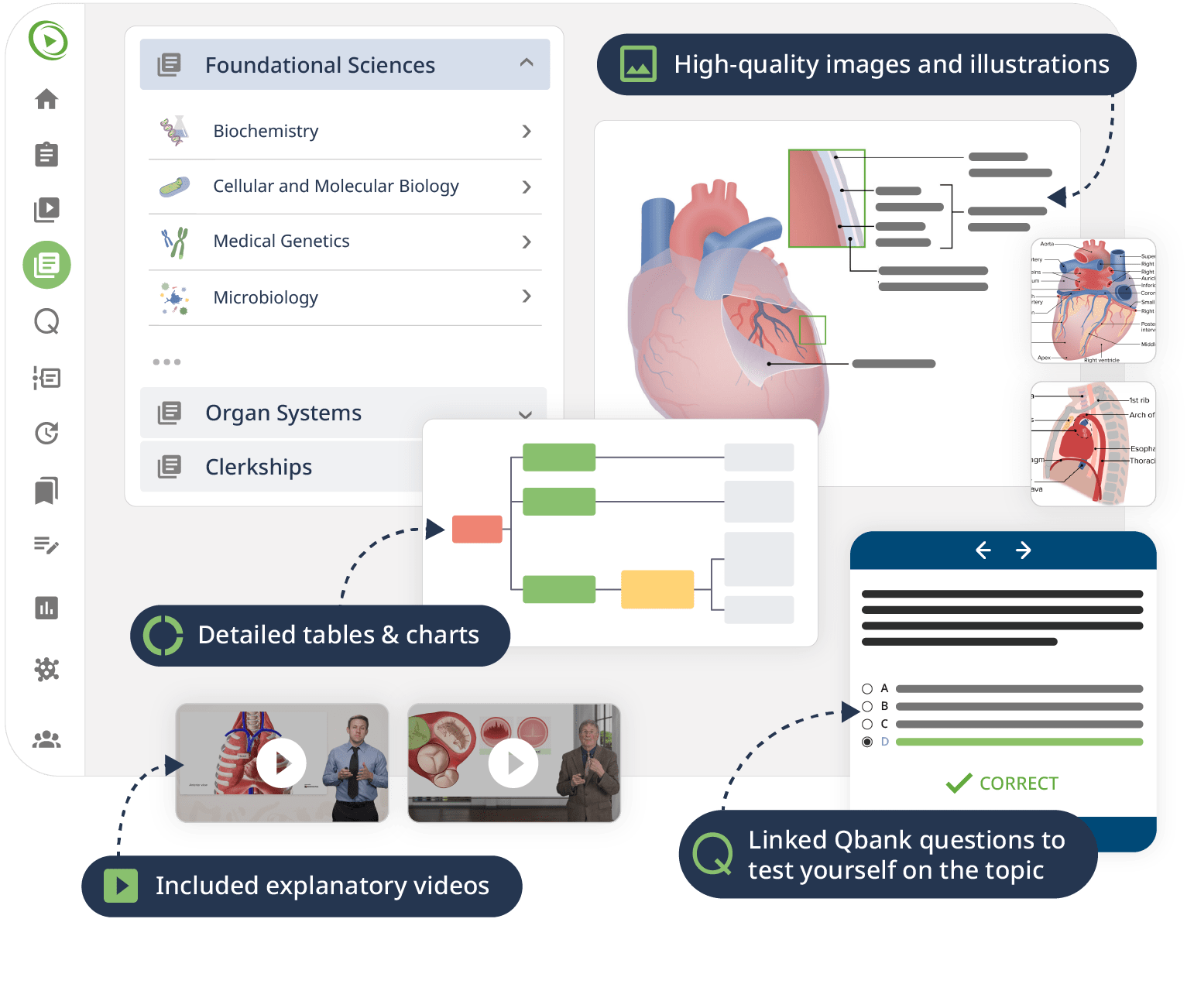
This course systematically teaches you everything you need to know on the subject of anatomy, beginning with the basics all the way through advanced topics. Moving from the brain, head, back, and upper limbs through the thorax and abdomen to the pelvis and lower limbs, a team of experienced educators walks you through the structures in a series of engaging Video Lessons, pointing out key concepts on high-quality illustrations. Interactive 3D models let you explore the organs and structures yourself.
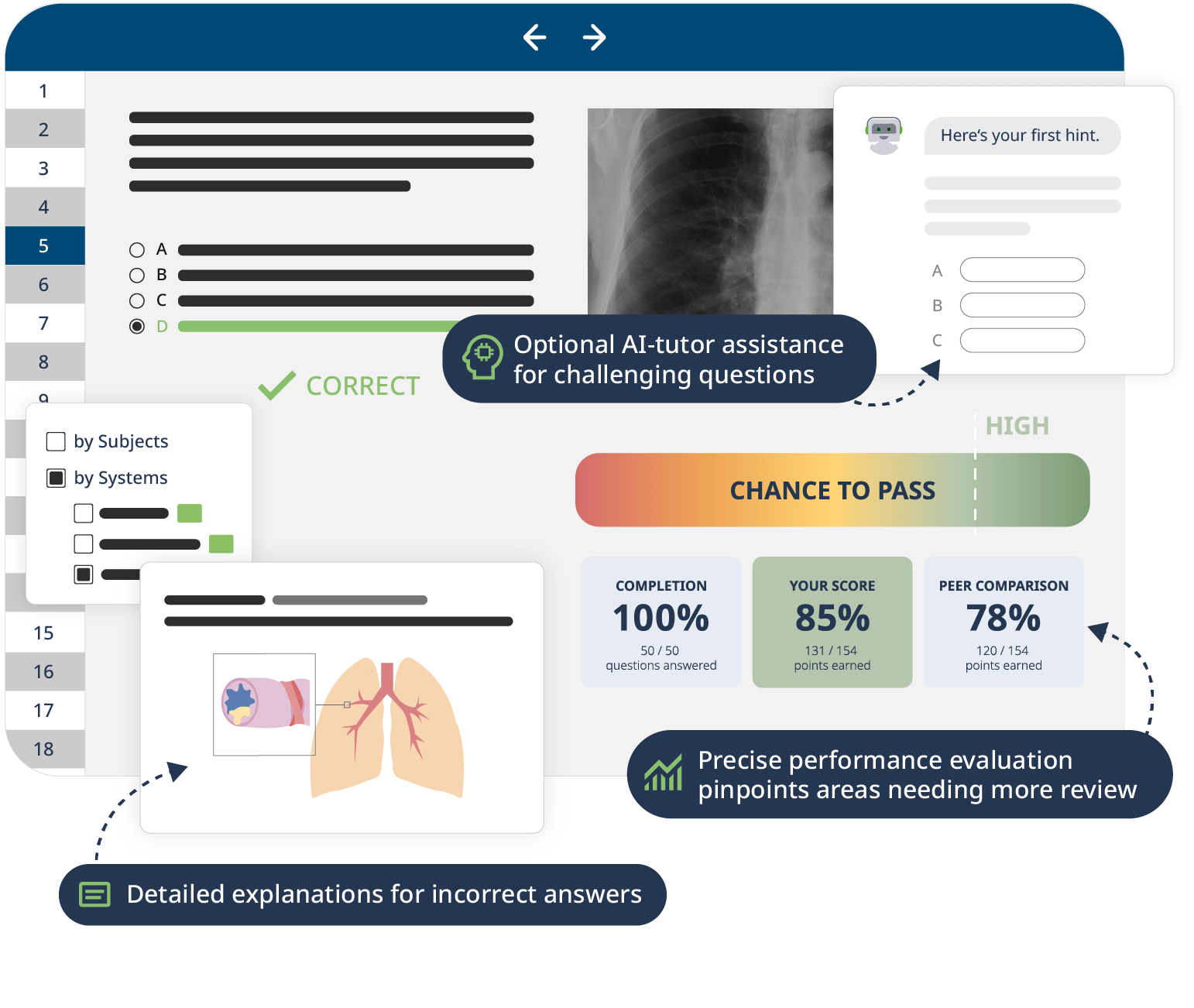
Downloadable study materials and a USMLE-style Qbank further support your learning, making it easy to understand and retain the topics. By the end of this course, you will have a comprehensive overview of the human body making you ready to ace your exams and dive into advanced clinical topics.