Anesthesiology is the field of medicine that focuses on interventions that bring a state of anesthesia upon an individual. General anesthesia is characterized by a reversible loss of consciousness along with analgesia, amnesia, and muscle relaxation. General anesthesia is induced via the administration of gaseous or injectable agents before surgical procedures or other medical interventions. On the other end of the spectrum is local anesthesia, which is achieved via the use of topical agents or the local administration of injectable anesthetics to the area of concern. The use of anesthetics has been well documented in history, but the practice of modern anesthesiology only began by the end of the 18th century.
Last updated: Dec 15, 2025
Anesthesiology is the field of medicine focusing on interventions that bring about a state of anesthesia, which is characterized by a reversible loss of consciousness, as well as analgesia, amnesia, and muscle relaxation.
| Years | Events |
|---|---|
| 4000 BCE–0 CE | The use of opium poppy; herbal remedies using Hyoscyamus niger, Mandragora, and aconitum; and acupuncture performed with bones, cannabis vapors, and carotid compression Compression Blunt Chest Trauma is documented in records from ancient China, Greece, and Egypt. |
| 1799–1850 CE |
|
| 1850–1900 CE |
|
| 1900–1925 CE |
|
| 1925–1950 CE |
|
| 1950–1975 CE |
|
| 1975–2000 CE |
|
| 2000 CE–present | The American Society of Anesthesiologists establishes a Simulation Education Network (SEN) to continue educating and certifying anesthesiologists. |
Focused evaluation and planning for anesthesia should be completed in advance for all surgeries, interventions, and procedures.
| Preexisting disease/condition | Diagnostic testing |
|---|---|
| Age > 65 years | Albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests, creatinine, hemoglobin |
| Alcohol use disorder Alcohol use disorder Alcohol is one of the most commonly used addictive substances in the world. Alcohol use disorder (AUD) is defined as pathologic consumption of alcohol leading to impaired daily functioning. Acute alcohol intoxication presents with impairment in speech and motor functions and can be managed in most cases with supportive care. Alcohol Use Disorder | ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG), electrolytes Electrolytes Electrolytes are mineral salts that dissolve in water and dissociate into charged particles called ions, which can be either be positively (cations) or negatively (anions) charged. Electrolytes are distributed in the extracellular and intracellular compartments in different concentrations. Electrolytes are essential for various basic life-sustaining functions. Electrolytes, hemoglobin, liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy function test, platelet count, PT/INR |
| Anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types | CBC, creatinine, ferritin Ferritin Iron-containing proteins that are widely distributed in animals, plants, and microorganisms. Their major function is to store iron in a nontoxic bioavailable form. Each ferritin molecule consists of ferric iron in a hollow protein shell (apoferritins) made of 24 subunits of various sequences depending on the species and tissue types. Hereditary Hemochromatosis, iron Iron A metallic element with atomic symbol fe, atomic number 26, and atomic weight 55. 85. It is an essential constituent of hemoglobins; cytochromes; and iron-binding proteins. It plays a role in cellular redox reactions and in the transport of oxygen. Trace Elements, transferrin Transferrin An iron-binding beta1-globulin that is synthesized in the liver and secreted into the blood. It plays a central role in the transport of iron throughout the circulation. Heme Metabolism saturation, TSH, T3 T3 A T3 thyroid hormone normally synthesized and secreted by the thyroid gland in much smaller quantities than thyroxine (T4). Most T3 is derived from peripheral monodeiodination of T4 at the 5′ position of the outer ring of the iodothyronine nucleus. The hormone finally delivered and used by the tissues is mainly t3. Thyroid Hormones, T4 T4 The major hormone derived from the thyroid gland. Thyroxine is synthesized via the iodination of tyrosines (monoiodotyrosine) and the coupling of iodotyrosines (diiodotyrosine) in the thyroglobulin. Thyroxine is released from thyroglobulin by proteolysis and secreted into the blood. Thyroxine is peripherally deiodinated to form triiodothyronine which exerts a broad spectrum of stimulatory effects on cell metabolism. Thyroid Hormones, vitamin B12 Vitamin B12 A cobalt-containing coordination compound produced by intestinal microorganisms and found also in soil and water. Higher plants do not concentrate vitamin B 12 from the soil and so are a poor source of the substance as compared with animal tissues. Intrinsic factor is important for the assimilation of vitamin B 12. Folate and Vitamin B12, blood typing, screening Screening Preoperative Care |
| Cardiac disease | BNP BNP A peptide that is secreted by the brain and the heart atria, stored mainly in cardiac ventricular myocardium. It can cause natriuresis; diuresis; vasodilation; and inhibits secretion of renin and aldosterone. It improves heart function. It contains 32 amino acids. Renal Sodium and Water Regulation, ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG), +/- stress testing |
| Diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus | Creatinine, HbA1c HbA1c Products of non-enzymatic reactions between glucose and hemoglobin a, occurring as a minor fraction of the hemoglobin components of human erythrocytes. Hemoglobin a1c is hemoglobin a with glucose covalently bound to the terminal valine of the beta chain. Glycated hemoglobin a is used as an index of the average blood sugar level over a lifetime of erythrocytes. Diabetes Mellitus, glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance |
| Liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease | Albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests, BUN, creatinine, electrolytes Electrolytes Electrolytes are mineral salts that dissolve in water and dissociate into charged particles called ions, which can be either be positively (cations) or negatively (anions) charged. Electrolytes are distributed in the extracellular and intracellular compartments in different concentrations. Electrolytes are essential for various basic life-sustaining functions. Electrolytes, hemoglobin, liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy function test, platelet count, PT/INR |
| Pulmonary disease Pulmonary disease Diseases involving the respiratory system. Blastomyces/Blastomycosis | Chest X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests |
| Thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy disease | T3 T3 A T3 thyroid hormone normally synthesized and secreted by the thyroid gland in much smaller quantities than thyroxine (T4). Most T3 is derived from peripheral monodeiodination of T4 at the 5′ position of the outer ring of the iodothyronine nucleus. The hormone finally delivered and used by the tissues is mainly t3. Thyroid Hormones, T4 T4 The major hormone derived from the thyroid gland. Thyroxine is synthesized via the iodination of tyrosines (monoiodotyrosine) and the coupling of iodotyrosines (diiodotyrosine) in the thyroglobulin. Thyroxine is released from thyroglobulin by proteolysis and secreted into the blood. Thyroxine is peripherally deiodinated to form triiodothyronine which exerts a broad spectrum of stimulatory effects on cell metabolism. Thyroid Hormones, TSH |
| American Society of Anesthesiologists physical status classification | Definition | Examples |
|---|---|---|
| I | A normal, healthy individual without known diseases | Healthy, nonsmoker, minimal alcohol use |
| II | An individual with mild systemic disease | Current smoker, mild hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, mild lung disease |
| III | An individual with severe systemic disease | Poorly controlled hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension or diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus, chronic obstructive pulmonary disease Pulmonary disease Diseases involving the respiratory system. Blastomyces/Blastomycosis |
| IV | An individual with severe systemic disease that is a constant threat to life | Recent MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction, severely reduced ejection fraction Ejection fraction Cardiac Cycle, sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock, ARDS |
| V | An individual who is not expected to survive without the intended operation | Brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification bleed, ruptured aneurysm Aneurysm An aneurysm is a bulging, weakened area of a blood vessel that causes an abnormal widening of its diameter > 1.5 times the size of the native vessel. Aneurysms occur more often in arteries than in veins and are at risk of dissection and rupture, which can be life-threatening. Thoracic Aortic Aneurysms, massive trauma |
| VI | An individual declared brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification dead or whose organs are being harvested |
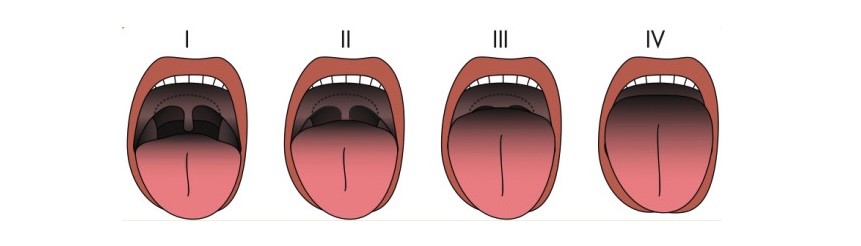
Mallampati classification to assess ease of airway access for intubation:
I: The soft palate, fauces, uvular, and pillars are visible.
II: The soft palate, fauces, and part of the uvula are visible.
III: The soft palate and base of the uvula are visible.
IV: Only the hard palate is visible.
The creation of a plan for anesthesia involves the consideration of:
Considerations include:
Several types of anesthesia are used for surgery or other medical procedures. Choosing the appropriate type depends on:
Types of anesthesia:
The 3 stages of general anesthesia are:
| Class | Commonly used drugs |
|---|---|
| IV sedative-hypnotics | Propofol Propofol An intravenous anesthetic agent which has the advantage of a very rapid onset after infusion or bolus injection plus a very short recovery period of a couple of minutes. Propofol has been used as anticonvulsants and antiemetics. Intravenous Anesthetics, etomidate Etomidate Imidazole derivative anesthetic and hypnotic with little effect on blood gases, ventilation, or the cardiovascular system. It has been proposed as an induction anesthetic. Intravenous Anesthetics, ketamine Ketamine A cyclohexanone derivative used for induction of anesthesia. Its mechanism of action is not well understood, but ketamine can block NMDA receptors (n-methyl-d-aspartate receptors) and may interact with sigma receptors. Intravenous Anesthetics |
| IV adjuvants | Opioids Opioids Opiates are drugs that are derived from the sap of the opium poppy. Opiates have been used since antiquity for the relief of acute severe pain. Opioids are synthetic opiates with properties that are substantially similar to those of opiates. Opioid Analgesics, lidocaine Lidocaine A local anesthetic and cardiac depressant used as an antiarrhythmic agent. Its actions are more intense and its effects more prolonged than those of procaine but its duration of action is shorter than that of bupivacaine or prilocaine. Local Anesthetics, midazolam Midazolam A short-acting hypnotic-sedative drug with anxiolytic and amnestic properties. It is used in dentistry, cardiac surgery, endoscopic procedures, as preanesthetic medication, and as an adjunct to local anesthesia. The short duration and cardiorespiratory stability makes it useful in poor-risk, elderly, and cardiac patients. It is water-soluble at ph less than 4 and lipid-soluble at physiological pH. Benzodiazepines |
| Inhalation agents | Nitrous oxide Nitrous oxide Nitrogen oxide (N2O). A colorless, odorless gas that is used as an anesthetic and analgesic. High concentrations cause a narcotic effect and may replace oxygen, causing death by asphyxia. Inhaled Anesthetics, halothane Halothane A nonflammable, halogenated, hydrocarbon anesthetic that provides relatively rapid induction with little or no excitement. Analgesia may not be adequate. Nitrous oxide is often given concomitantly. Because halothane may not produce sufficient muscle relaxation, supplemental neuromuscular blocking agents may be required. Inhaled Anesthetics, isoflurane Isoflurane A stable, non-explosive inhalation anesthetic, relatively free from significant side effects. Inhaled Anesthetics |
| Neuromuscular blockers Neuromuscular blockers Neuromuscular blockers are skeletal muscle relaxant medications that block muscle contraction through a couple of mechanisms. Depolarizing neuromuscular blockers bind to nicotinic cholinergic receptors (nAChRs), locking the ion channel open. This results in muscle relaxation and paralysis. Neuromuscular Blockers | Vecuronium Vecuronium Monoquaternary homolog of pancuronium. A non-depolarizing neuromuscular blocking agent with shorter duration of action than pancuronium. Its lack of significant cardiovascular effects and lack of dependence on good kidney function for elimination as well as its short duration of action and easy reversibility provide advantages over, or alternatives to, other established neuromuscular blocking agents. Neuromuscular Blockers, rocuronium Rocuronium An androstanol non-depolarizing neuromuscular blocking agent. It has a mono-quaternary structure and is a weaker nicotinic antagonist than pancuronium. Neuromuscular Blockers, succinylcholine Succinylcholine A quaternary skeletal muscle relaxant usually used in the form of its bromide, chloride, or iodide. It is a depolarizing relaxant, acting in about 30 seconds and with a duration of effect averaging three to five minutes. Succinylcholine is used in surgical, anesthetic, and other procedures in which a brief period of muscle relaxation is called for. Cholinomimetic Drugs |
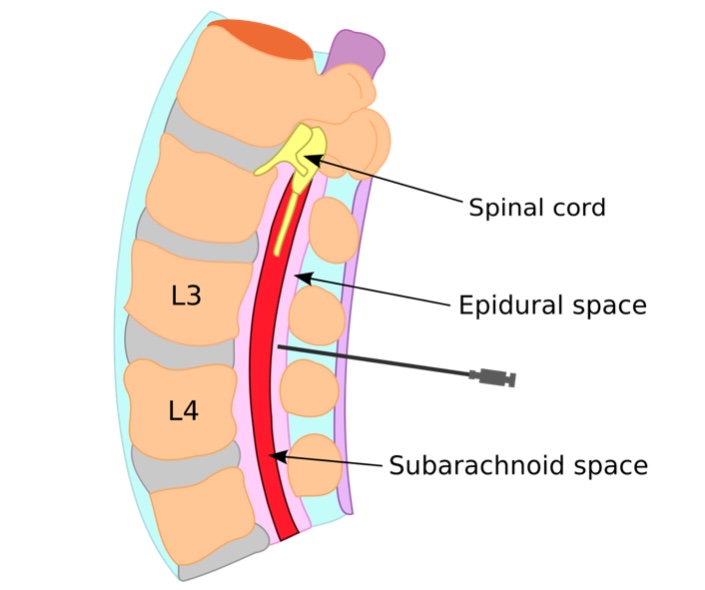
Epidural anesthesia is commonly used during childbirth:
Anesthesiologists place a catheter between the L3 and L4 vertebrae into the epidural space for the continuous delivery of local anesthetics. Common epidural agents include lidocaine, bupivacaine, and ropivacaine.
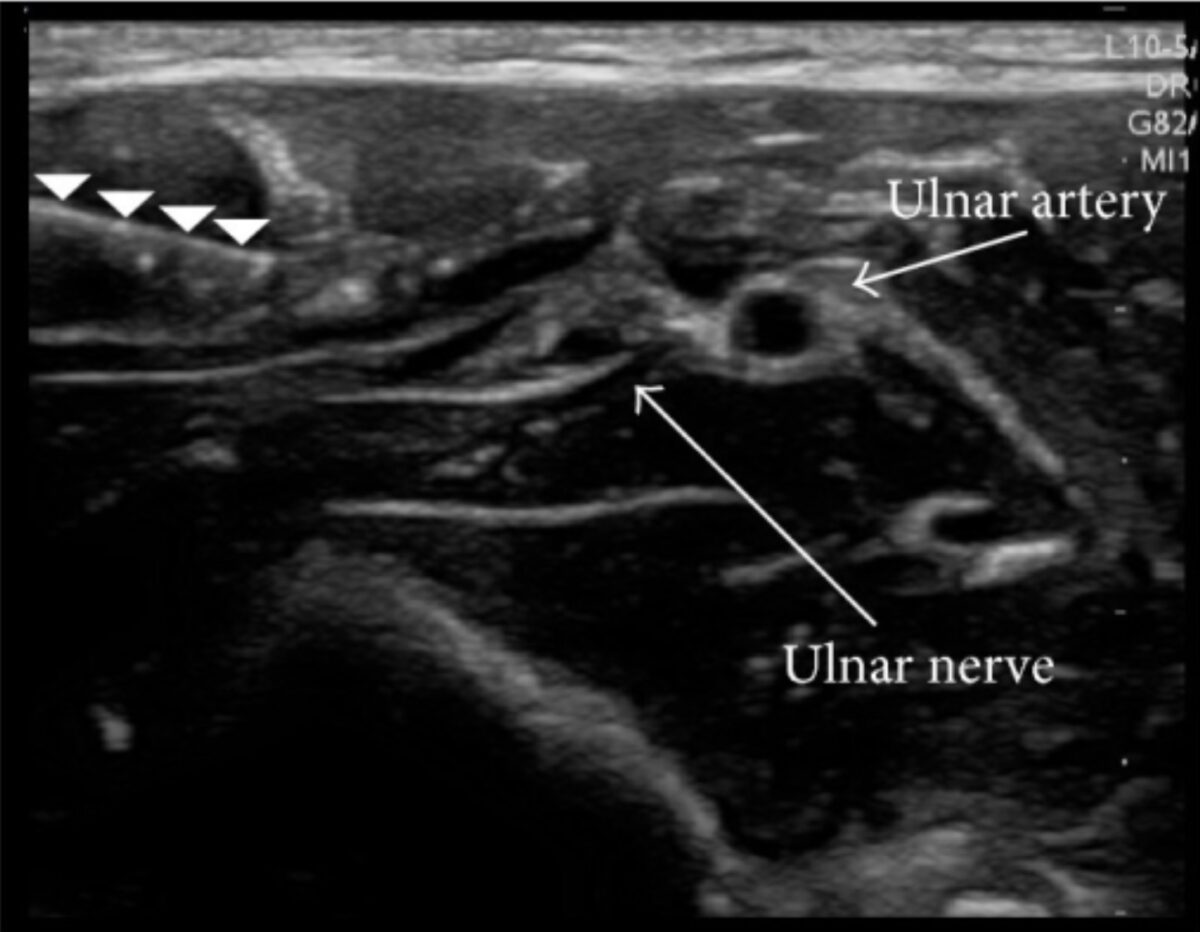
Ultrasound-guided nerve block:
Ultrasound demonstrating a needle (row of white arrowheads) and an anesthetic solution (dark area surrounding the ulnar nerve) injected around the ulnar nerve for successful peripheral nerve block. Anesthetic blockade of a nerve bundle blocks all nerves downstream, providing adequate analgesia for a procedure. Notice how the anesthesiologist identified the ulnar artery to avoid puncturing it.
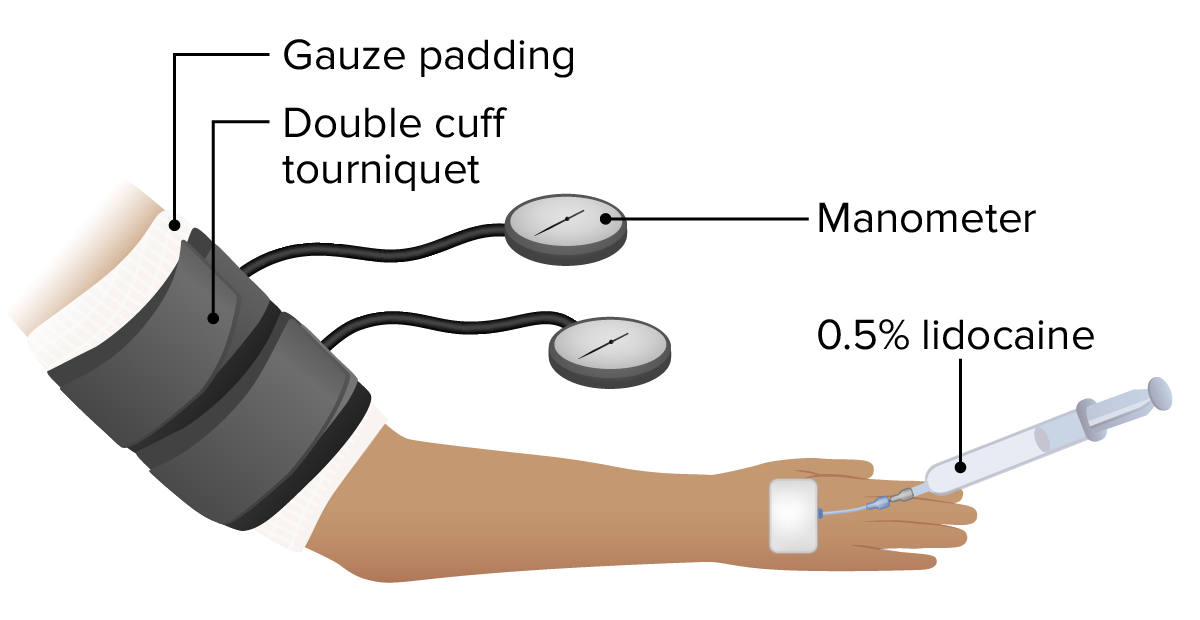
Basic setup for a Bier block
Image by Lecturio.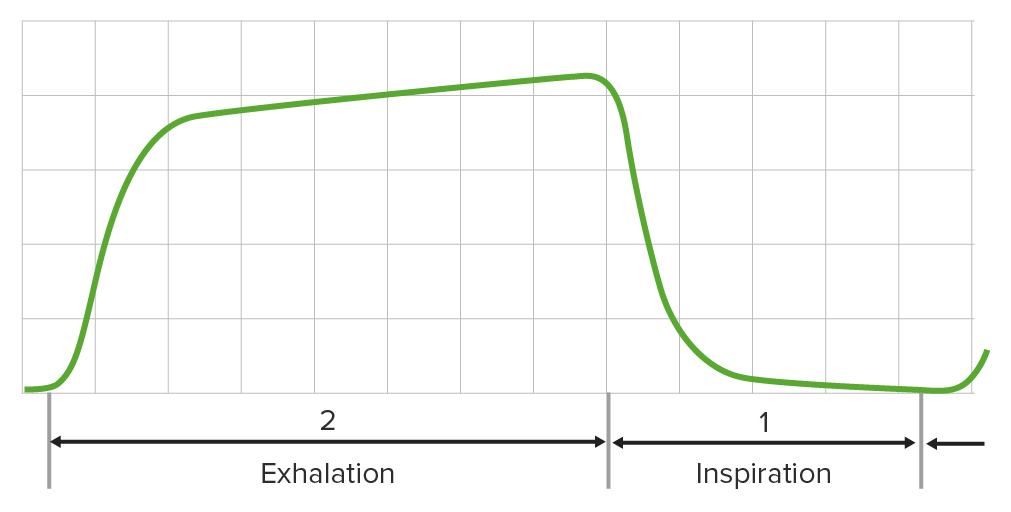
Normal capnogram reflecting appropriate CO2 levels in an individual receiving general anesthesia:
Capnography reflects adequate ventilation during surgery.
| Stage I | Conscious and rational with decreased pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways perception Perception The process by which the nature and meaning of sensory stimuli are recognized and interpreted. Psychiatric Assessment |
|---|---|
| Stage II | Unconscious Unconscious Those forces and content of the mind which are not ordinarily available to conscious awareness or to immediate recall. Psychotherapy and reflexive with an irregular breathing pattern |
| Stage III | Inability to protect the airway Airway ABCDE Assessment due to increased muscle relaxation |
| Stage IV | Cardiovascular and respiratory depression (medullary) |
All individuals are monitored postoperatively in a PACU, where standard procedures are followed: