Pyruvate kinase Pyruvate kinase Atp:pyruvate 2-o-phosphotransferase. A phosphotransferase that catalyzes reversibly the phosphorylation of pyruvate to phosphoenolpyruvate in the presence of ATP. It has four isozymes (l, r, m1, and m2). Glycolysis (PK) deficiency is an autosomal recessive Autosomal recessive Autosomal inheritance, both dominant and recessive, refers to the transmission of genes from the 22 autosomal chromosomes. Autosomal recessive diseases are only expressed when 2 copies of the recessive allele are inherited. Autosomal Recessive and Autosomal Dominant Inheritance enzymatic disorder of erythrocytes Erythrocytes Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology that results in hemolytic anemia Hemolytic Anemia Hemolytic anemia (HA) is the term given to a large group of anemias that are caused by the premature destruction/hemolysis of circulating red blood cells (RBCs). Hemolysis can occur within (intravascular hemolysis) or outside the blood vessels (extravascular hemolysis). Hemolytic Anemia. PK deficiency is mainly a hereditary disorder, with a defect in the PKLR or PKM gene Gene A category of nucleic acid sequences that function as units of heredity and which code for the basic instructions for the development, reproduction, and maintenance of organisms. Basic Terms of Genetics, but it can be acquired secondary to underlying conditions, such as leukemia. The typical clinical features of PK deficiency are mild to moderate anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types, jaundice Jaundice Jaundice is the abnormal yellowing of the skin and/or sclera caused by the accumulation of bilirubin. Hyperbilirubinemia is caused by either an increase in bilirubin production or a decrease in the hepatic uptake, conjugation, or excretion of bilirubin. Jaundice, delay in growth, failure to thrive Failure to Thrive Failure to thrive (FTT), or faltering growth, describes suboptimal weight gain and growth in children. The majority of cases are due to inadequate caloric intake; however, genetic, infectious, and oncological etiologies are also common. Failure to Thrive, and frontal bossing Frontal Bossing Hydrocephalus in Children. However, more severe presentations are possible, especially in younger patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship. Diagnosis involves ruling out other, more common, causes of hemolytic anemia Hemolytic Anemia Hemolytic anemia (HA) is the term given to a large group of anemias that are caused by the premature destruction/hemolysis of circulating red blood cells (RBCs). Hemolysis can occur within (intravascular hemolysis) or outside the blood vessels (extravascular hemolysis). Hemolytic Anemia. Biochemical assays and/or genetic testing Genetic Testing Detection of a mutation; genotype; karyotype; or specific alleles associated with genetic traits, heritable diseases, or predisposition to a disease, or that may lead to the disease in descendants. It includes prenatal genetic testing. Myotonic Dystrophies can confirm the diagnosis. Management may include supportive treatment, mitapivat (a PK activator recently approved by the FDA), exchange transfusion, phototherapy Phototherapy Treatment of disease by exposure to light, especially by variously concentrated light rays or specific wavelengths. Hyperbilirubinemia of the Newborn, or splenectomy Splenectomy Surgical procedure involving either partial or entire removal of the spleen. Rupture of the Spleen. Prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is age-dependent, with older age at diagnosis associated with a better prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas.
Last updated: Apr 5, 2023
Pyruvate kinase Pyruvate kinase Atp:pyruvate 2-o-phosphotransferase. A phosphotransferase that catalyzes reversibly the phosphorylation of pyruvate to phosphoenolpyruvate in the presence of ATP. It has four isozymes (l, r, m1, and m2). Glycolysis (PK) deficiency is an autosomal recessive Autosomal recessive Autosomal inheritance, both dominant and recessive, refers to the transmission of genes from the 22 autosomal chromosomes. Autosomal recessive diseases are only expressed when 2 copies of the recessive allele are inherited. Autosomal Recessive and Autosomal Dominant Inheritance enzymatic disorder of erythrocytes Erythrocytes Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology that results in chronic hemolysis due to a defect in the PKLR or PKM gene Gene A category of nucleic acid sequences that function as units of heredity and which code for the basic instructions for the development, reproduction, and maintenance of organisms. Basic Terms of Genetics.
Pyruvate kinase Pyruvate kinase Atp:pyruvate 2-o-phosphotransferase. A phosphotransferase that catalyzes reversibly the phosphorylation of pyruvate to phosphoenolpyruvate in the presence of ATP. It has four isozymes (l, r, m1, and m2). Glycolysis is an enzyme required for the conversion of phosphoenolpyruvate Phosphoenolpyruvate A monocarboxylic acid anion derived from selective deprotonation of the carboxy group of phosphoenolpyruvic acid. It is a metabolic intermediate in glycolysis; gluconeogenesis; and other pathways. Glycolysis ( PEP PEP A monocarboxylic acid anion derived from selective deprotonation of the carboxy group of phosphoenolpyruvic acid. It is a metabolic intermediate in glycolysis; gluconeogenesis; and other pathways. Glycolysis) into pyruvate Pyruvate Derivatives of pyruvic acid, including its salts and esters. Glycolysis and ATP in the energy-producing glycolysis Glycolysis Glycolysis is a central metabolic pathway responsible for the breakdown of glucose and plays a vital role in generating free energy for the cell and metabolites for further oxidative degradation. Glucose primarily becomes available in the blood as a result of glycogen breakdown or from its synthesis from noncarbohydrate precursors (gluconeogenesis) and is imported into cells by specific transport proteins. Glycolysis pathway.
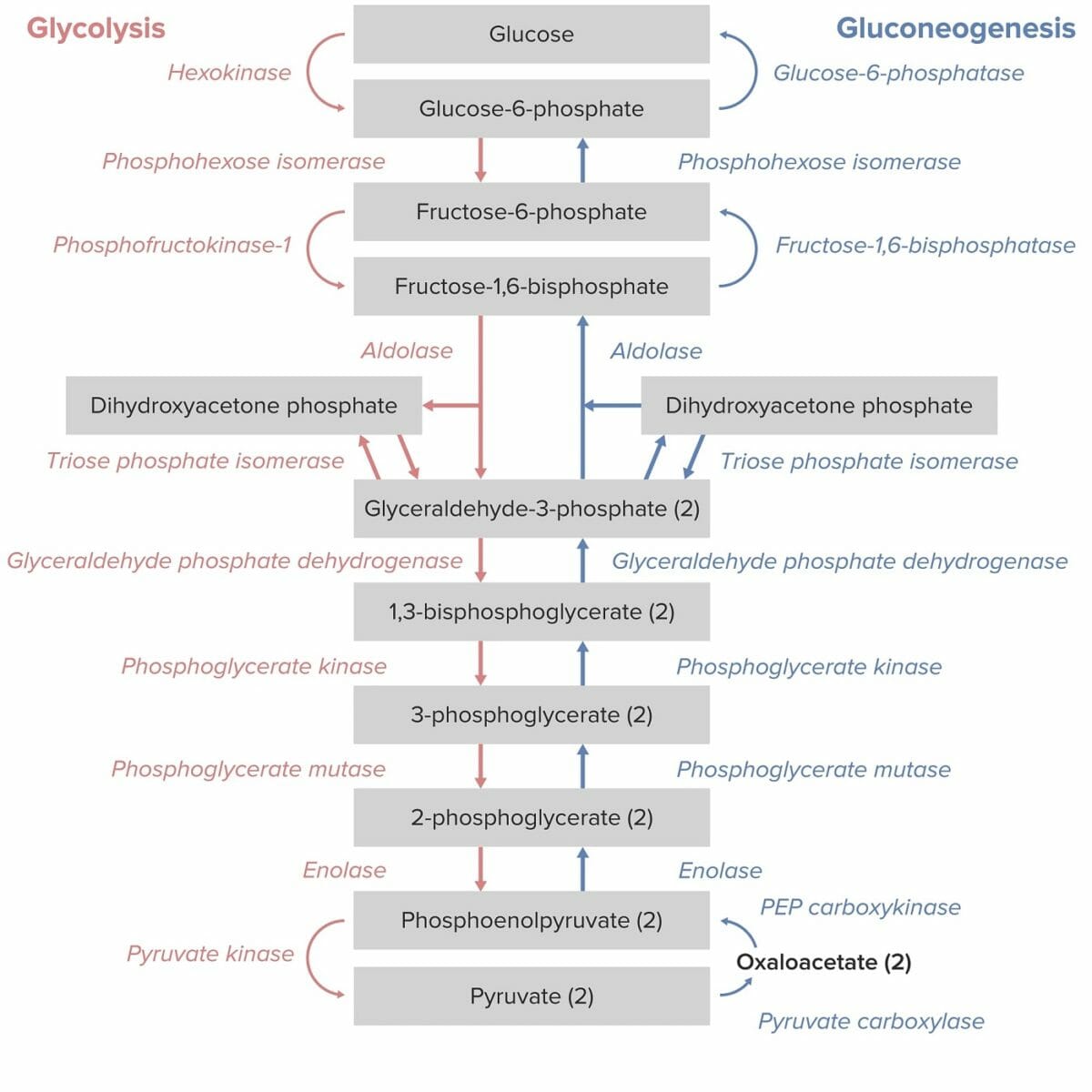
Glycolysis and gluconeogenesis pathways:
Note that the conversion of phosphoenolpyruvate to pyruvate by pyruvate kinase is the final step in the glycolysis pathway.
Effect of PK deficiency:
Consequences of PK deficiency:
The age and severity at presentation depend on the extent of hemolysis and anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types. Additionally, the age at presentation may vary.
Signs and symptoms in newborns:
Signs and symptoms in older children and adults:
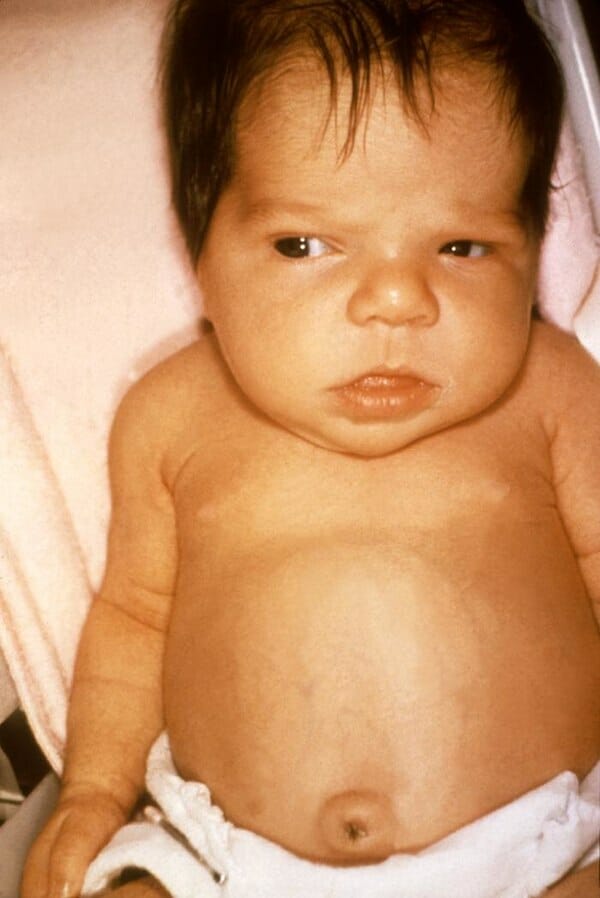
A 6-week-old girl with symptoms of jaundice due to hypothyroidism
Image: “Jaundice in newborn” by Dr. Hudson (CDC). License: Public DomainPyruvate kinase Pyruvate kinase Atp:pyruvate 2-o-phosphotransferase. A phosphotransferase that catalyzes reversibly the phosphorylation of pyruvate to phosphoenolpyruvate in the presence of ATP. It has four isozymes (l, r, m1, and m2). Glycolysis deficiency is rare; ruling out other causes of hemolytic anemia Hemolytic Anemia Hemolytic anemia (HA) is the term given to a large group of anemias that are caused by the premature destruction/hemolysis of circulating red blood cells (RBCs). Hemolysis can occur within (intravascular hemolysis) or outside the blood vessels (extravascular hemolysis). Hemolytic Anemia is important.
CBC with differential:
Chemistry:
Antiglobulin testing:
Peripheral blood smear Peripheral Blood Smear Anemia: Overview and Types, focusing on red cell morphology:
Diagnosis is confirmed if a patient with hemolytic anemia Hemolytic Anemia Hemolytic anemia (HA) is the term given to a large group of anemias that are caused by the premature destruction/hemolysis of circulating red blood cells (RBCs). Hemolysis can occur within (intravascular hemolysis) or outside the blood vessels (extravascular hemolysis). Hemolytic Anemia/compensated hemolysis has abnormalities on either biochemical or genetic testing Genetic Testing Detection of a mutation; genotype; karyotype; or specific alleles associated with genetic traits, heritable diseases, or predisposition to a disease, or that may lead to the disease in descendants. It includes prenatal genetic testing. Myotonic Dystrophies.
Biochemical testing:
Genetic testing Genetic Testing Detection of a mutation; genotype; karyotype; or specific alleles associated with genetic traits, heritable diseases, or predisposition to a disease, or that may lead to the disease in descendants. It includes prenatal genetic testing. Myotonic Dystrophies:
Indications for genetic testing Genetic Testing Detection of a mutation; genotype; karyotype; or specific alleles associated with genetic traits, heritable diseases, or predisposition to a disease, or that may lead to the disease in descendants. It includes prenatal genetic testing. Myotonic Dystrophies:
Management is dependent on the age at diagnosis and the severity.
Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship should be monitored for: