Asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma is a chronic inflammatory condition causing intermittent airway Airway ABCDE Assessment obstruction, wheezing Wheezing Wheezing is an abnormal breath sound characterized by a whistling noise that can be relatively high-pitched and shrill (more common) or coarse. Wheezing is produced by the movement of air through narrowed or compressed small (intrathoracic) airways. Wheezing, cough, and dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea. Genetics Genetics Genetics is the study of genes and their functions and behaviors. Basic Terms of Genetics and environmental factors play a significant role in etiology. A diagnosis of asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma in children often involves careful history taking, physical examination, pulmonary function tests, and radiologic studies to rule out other conditions. The goal is to minimize symptoms, exacerbations, and functional as well as psychological morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status. Treatment also involves relief and chronic pharmacotherapy.
Last updated: Dec 15, 2025
Asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma is defined as the episodic obstruction of lung airways resulting from a chronic inflammatory condition.
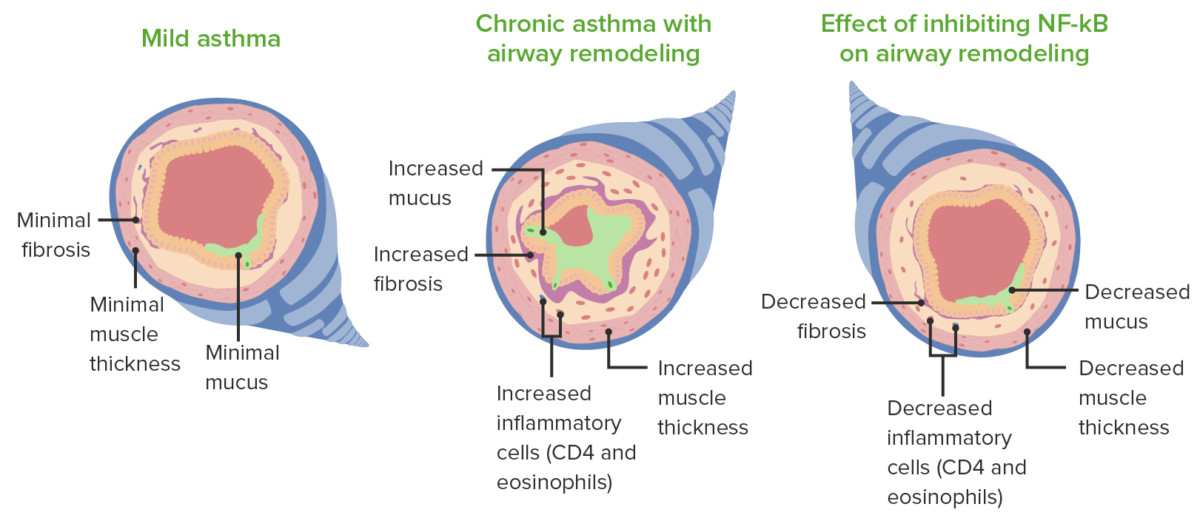
Remodeling and pathological changes noted in asthma.
Image by Lecturio.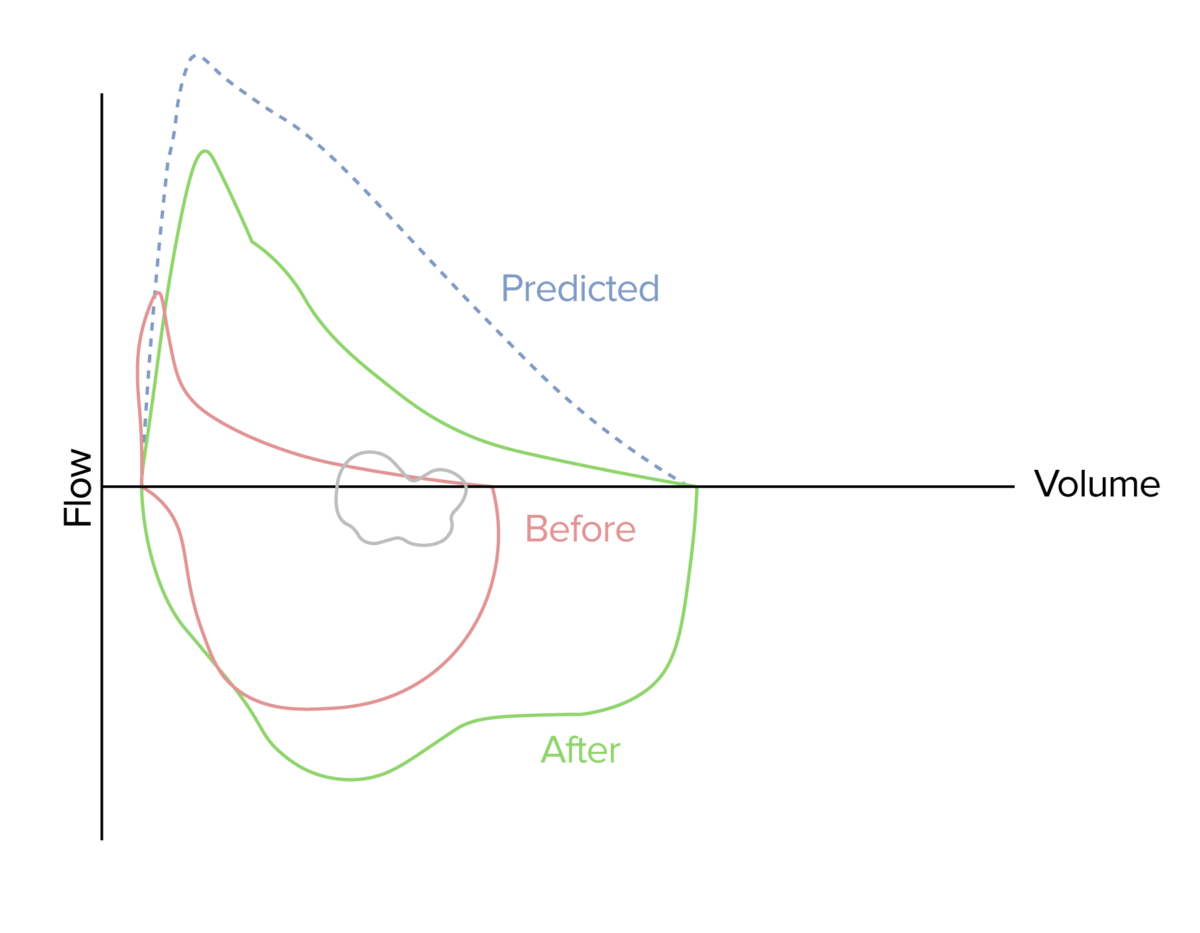
Flow-volume loop demonstrating improved airflow (green loop) following the administration of a short-acting bronchodilator in a patient with acute asthma attack (red loop)
Image by Lecturio.
A child using a peak flow meter in a clinic
Image: A child using a peak expiratory flow meter in a pediatric clinic. By: National Heart, Lung and Blood Institute. License: Public domainThe goal of asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma management is to prevent/minimize symptoms, exacerbations, and functional and psychological morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status to provide a healthy lifestyle appropriate for the age of the child.
The management of asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma has 4 components:
| Component of severity | Classification of asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma severity | |||
|---|---|---|---|---|
| Intermittent | Persistent | |||
| Mild | Moderate | Severe | ||
| Symptoms | ≤ 2 days/week | > 2 days/week | Daily | Throughout the day |
| SABA use | ≤ 2 days/week | > 2 days/week | Daily | Several times/day |
| Nighttime awakenings | ≤ 2/month | 3–4/month | ≥ 1/week | Nightly |
| Activity limitation | None | Minor | Some | Extreme |
| Lung function (only in children > 5 years) |
|
|
|
|
| Exacerbation requiring oral corticosteroid use | 0–1 times/year | ≥ 2 times/year | ||
| Recommended action for treatment | Step 1 | Step 2 | Step 3 + medium-dose inhalded corticosteroids Corticosteroids Chorioretinitis (ICS) | Step 3 + medium-dose ICS, or Step 4 or 5 |
| Consider a short course of oral corticosteroids Corticosteroids Chorioretinitis. | ||||
| In 2–6 weeks, evaluate for control and adjust dose accordingly. | ||||
| Component of control | Well controlled | Not well controlled | Very poorly controlled |
|---|---|---|---|
| Symptoms | ≤ 2 days/week | > 2 days/week or multiple times on ≤ 2 days/week | Throughout the day |
| SABA use | ≤ 2 days/week | > 2 days/week or multiple times on ≤ 2 days/week | Several times/day |
| Symptoms | ≤ 2 days/week | > 2 days/week | Throughout the day |
| Nighttime awakenings | ≤ 1/month | ≥ 2/month | ≥ 2/week |
| Activity limitation | None | Some | Extreme |
| Lung function | |||
| FEV1 | > 80% | 60%–80% | < 60% |
| FEV1/FVC | > 80% | 75%–80% | < 75% |
| Exacerbation requiring oral corticosteroid use | 0–1/year | ≥ 2/year | |
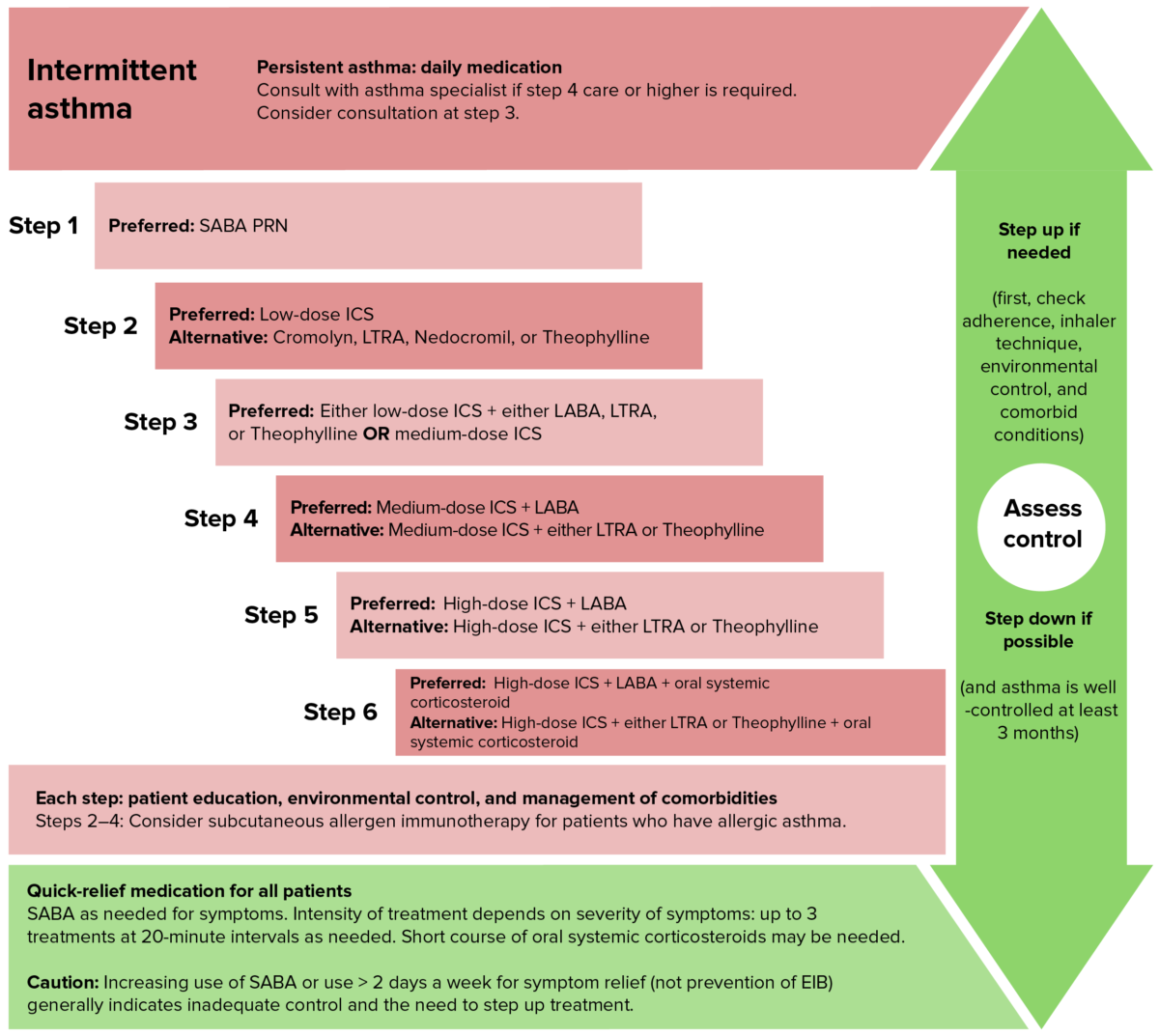
Step up ladder approach in management of asthma for children between 5-11. Note in children, long-acting bronchodilators are not used initially and the aim is to have lower doses of inhaled corticosteroids.
Image by Lecturio.Acute exacerbation of asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma is the acute or subacute progressive worsening of airway Airway ABCDE Assessment inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation and obstruction in an asthmatic patient.
| Mild | Moderate | Severe | Respiratory arrest imminent | |
|---|---|---|---|---|
| Alertness | Normal | Usually agitated | Agitated | Drowsy or confused |
| Respiratory rate Respiratory rate The number of times an organism breathes with the lungs (respiration) per unit time, usually per minute. Pulmonary Examination (breaths/minute) | Increased | Increased | > 30 | Paradoxical thoracoabdominal movement or normal-low respiratory rate Respiratory rate The number of times an organism breathes with the lungs (respiration) per unit time, usually per minute. Pulmonary Examination |
| Pulse (beats/minute) | < 100 | 100–120 | >120 | Bradycardia Bradycardia Bradyarrhythmia is a rhythm in which the heart rate is less than 60/min. Bradyarrhythmia can be physiologic, without symptoms or hemodynamic change. Pathologic bradyarrhythmia results in reduced cardiac output and hemodynamic instability causing syncope, dizziness, or dyspnea. Bradyarrhythmias |
| Wheeze | End expiratory only | Throughout expiration Expiration Ventilation: Mechanics of Breathing | Throughout inhalation and expiration Expiration Ventilation: Mechanics of Breathing | Absent |
| Inspiratory/expiratory ratio (normally 2:1) | Inspiratory/expiratory ratio of 1:1 | Inspiratory/expiratory ratio of 1:2 | < 1:2 | N/A |
| Accessory muscle use | None | Common | Present | Present, but decreasing |
| O2 saturation | > 95% | 90%–95% | < 90% ± cyanosis Cyanosis A bluish or purplish discoloration of the skin and mucous membranes due to an increase in the amount of deoxygenated hemoglobin in the blood or a structural defect in the hemoglobin molecule. Pulmonary Examination | < 90% ± cyanosis Cyanosis A bluish or purplish discoloration of the skin and mucous membranes due to an increase in the amount of deoxygenated hemoglobin in the blood or a structural defect in the hemoglobin molecule. Pulmonary Examination |
| PCO2 (mm Hg) | < 42 | < 42 | < 42 | < 42 |
| Peak expiratory flow Peak expiratory flow Measurement of the maximum rate of airflow attained during a forced vital capacity determination. Common abbreviations are pefr and pfr. Asthma | ≥ 70% | 40%–69% | 25%–39% | ≤ 25% |