Constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation is a common complaint in children that is relatively defined for individual age groups based on the frequency and difficulty of defecation Defecation The normal process of elimination of fecal material from the rectum. Gastrointestinal Motility and stool consistency Consistency Dermatologic Examination. The majority of constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation cases are functional or non-organic. Clinical presentation may vary, from insufficient evacuation noted by the parents, to complaints of abdominal pain Abdominal Pain Acute Abdomen, to secondary incontinence. Often, a combination of non-pharmacologic and pharmacologic management is needed for evacuating bowel content, eliminating pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways upon defecation Defecation The normal process of elimination of fecal material from the rectum. Gastrointestinal Motility, and improving bowel habits.
Last updated: Dec 15, 2025
| Infants and toddlers (≤4 years developmental age) | Children (>4 years developmental age) |
|---|---|
| At least 2 of the following findings for over 1 month: | At least 2 of the following findings for over 1 month, occurring at least once per week: |
|
|
Additional criteria for toilet-trained children:
|
| Nonorganic (functional or retentive) | No underlying pathologic causes |
|---|---|
| Anatomic |
|
| Abnormal musculature |
|
| Intestinal nerve or muscle abnormalities |
|
| Metabolic disorders |
|
| Intestinal disorders |
|
| Drugs |
|
| Psychiatric | Anorexia Anorexia The lack or loss of appetite accompanied by an aversion to food and the inability to eat. It is the defining characteristic of the disorder anorexia nervosa. Anorexia Nervosa nervosa |
Functional constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation is the most common cause of constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation:
History and exam are performed to rule out any organic causes and reassure the provider that the symptoms in question are due to functional constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation.
Toileting patterns:
Timing of onset of symptoms:
Psychosocial stressors:
Behavioral cues:
Cues pointing to organic etiologies:
General:
Abdominal exam:
Rectal exam:
Neurologic exam:
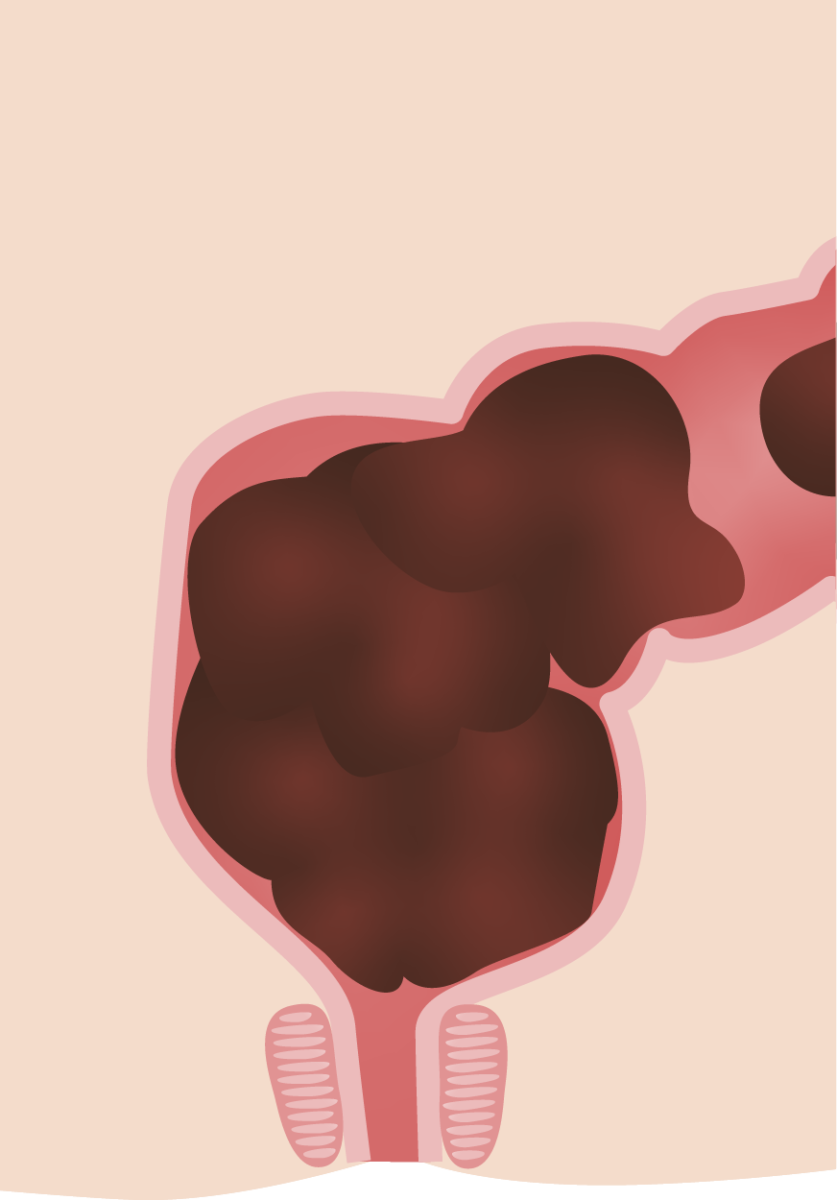
Cross-section depiction of the rectal vault in constipation with large fecal burden seen often in functional constipation in children
Image by Lecturio.In an otherwise healthy child, functional constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation is diagnosed clinically. Laboratory examination should be directed by cues suggesting other pathologic causes:
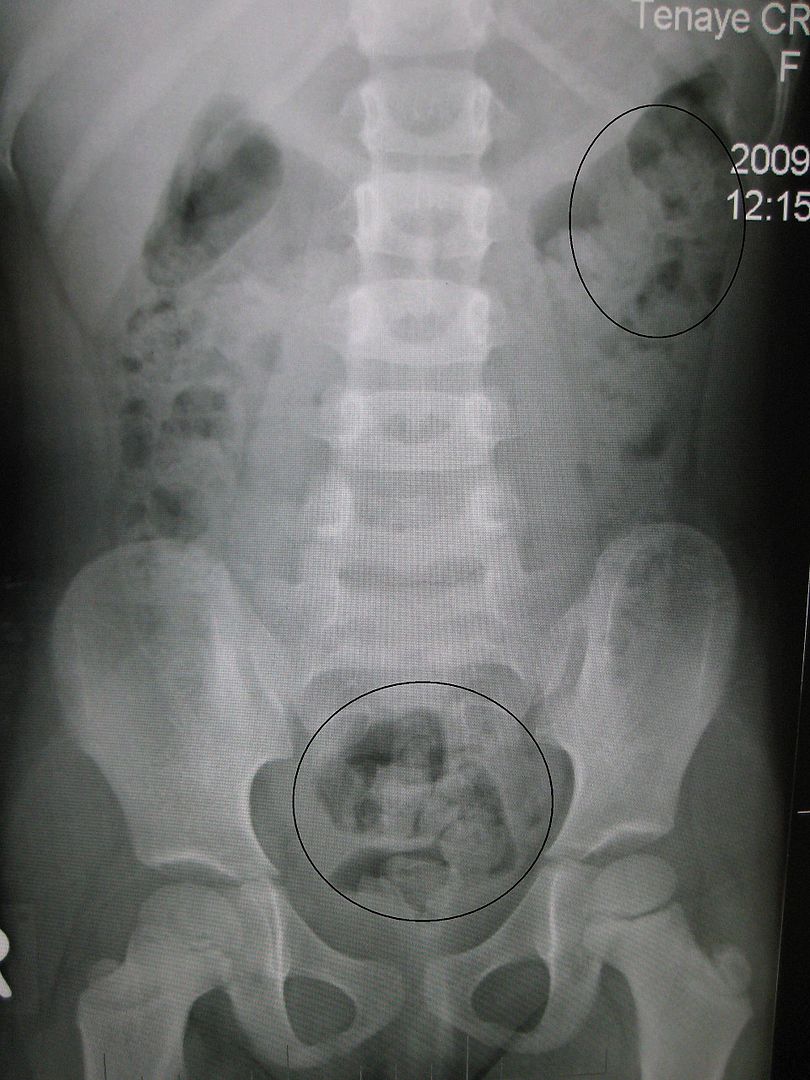
Anterior view X-ray of a young boy showing significant fecal burden in the rectum suggestive of constipation
Image: “Constipation in a young child as seen on X-ray” by James Heilman, MD. License: CC BY 3.0.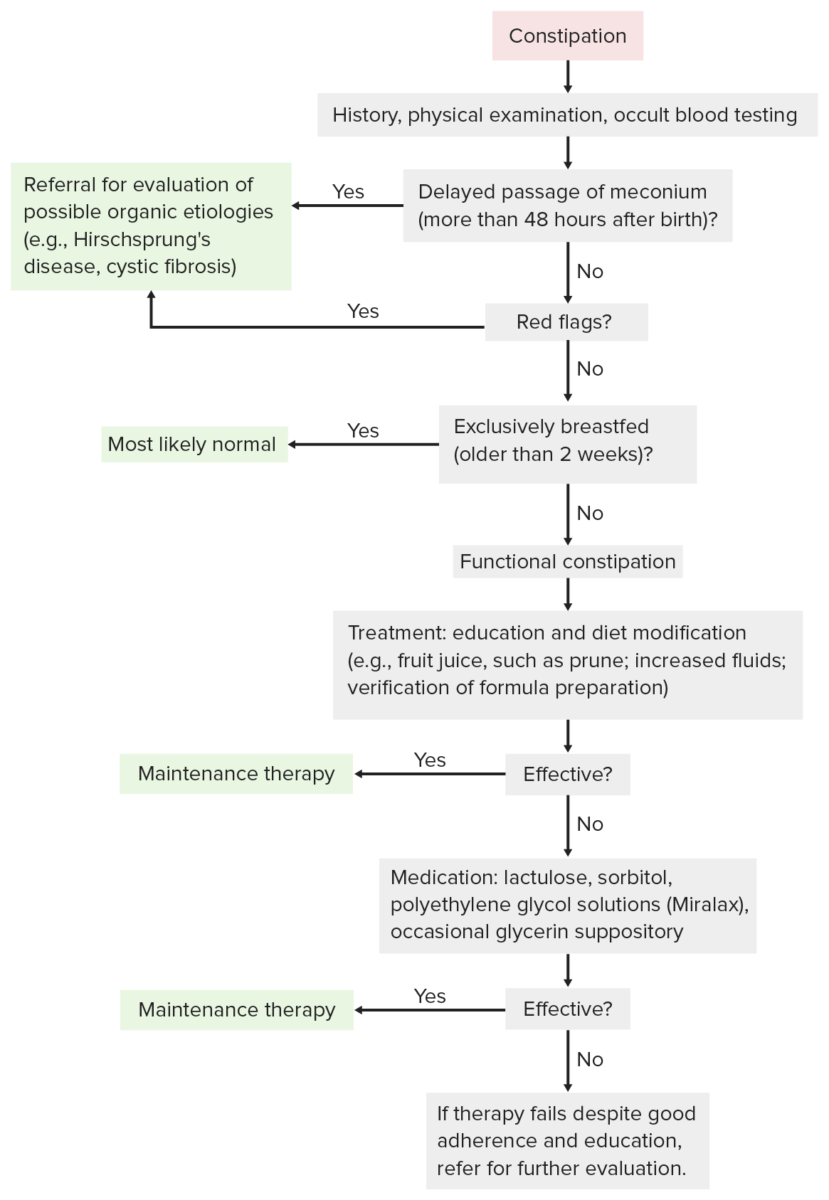
Diagnostic and management flow charts for constipation.
Image by Lecturio.