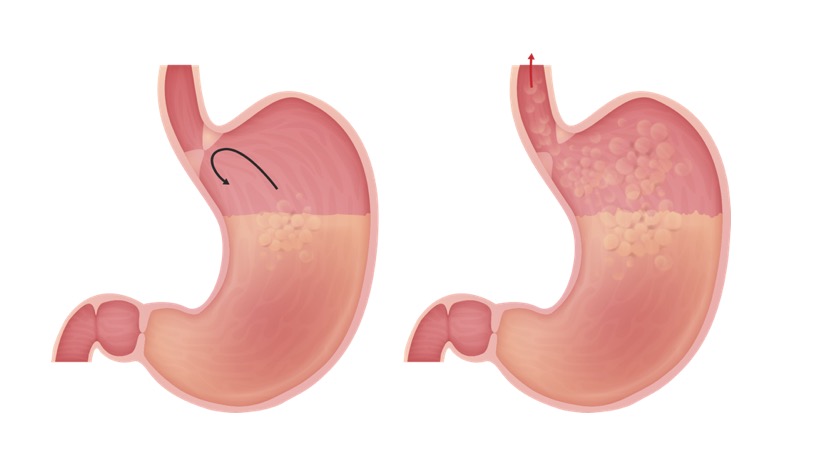
Gastroesophageal reflux disease (GERD) is due to pathologic reflux that causes symptoms and complications, including erosive esophagitis. Common symptoms are heartburn, early satiety, bloating, and belching. Diagnosis is made clinically and requires endoscopy in adults over 55 who are unresponsive to empiric therapy with acid blockade or those with alarm symptoms. Uncomplicated GERD can be managed with lifestyle changes and over-the-counter medications. Complications include erosive esophagitis, stricture, and Barrett esophagus, which can increase the risk of esophageal cancer. Management includes lifestyle and dietary modification, acid-reducing medications, and in some cases, surgery.
Last updated: Dec 15, 2025
Gastroesophageal reflux disease (GERD) is the passage of gastric contents into the esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy that leads to symptoms or complications.
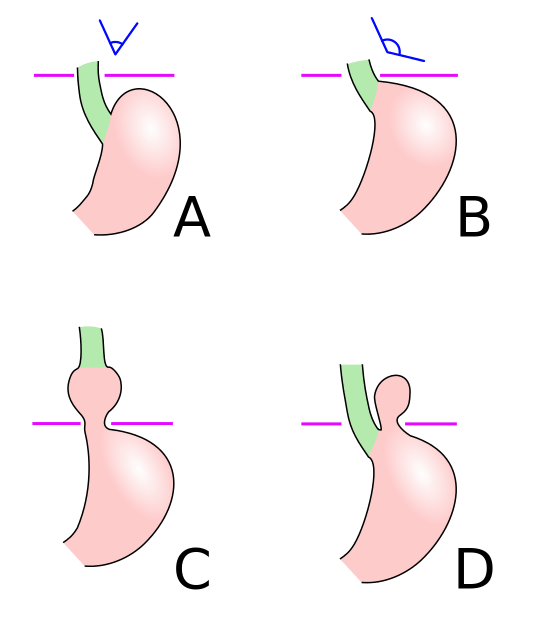
Schematic diagram of different types of hiatal hernia. A: Normal anatomy. B: Pre-stage (note the widening of the esophagogastric angle). C: Sliding hiatal hernia. D: Paraesophageal hiatal hernia
Image: “Hiatus hernia” by Mysid. License: CC0 1.0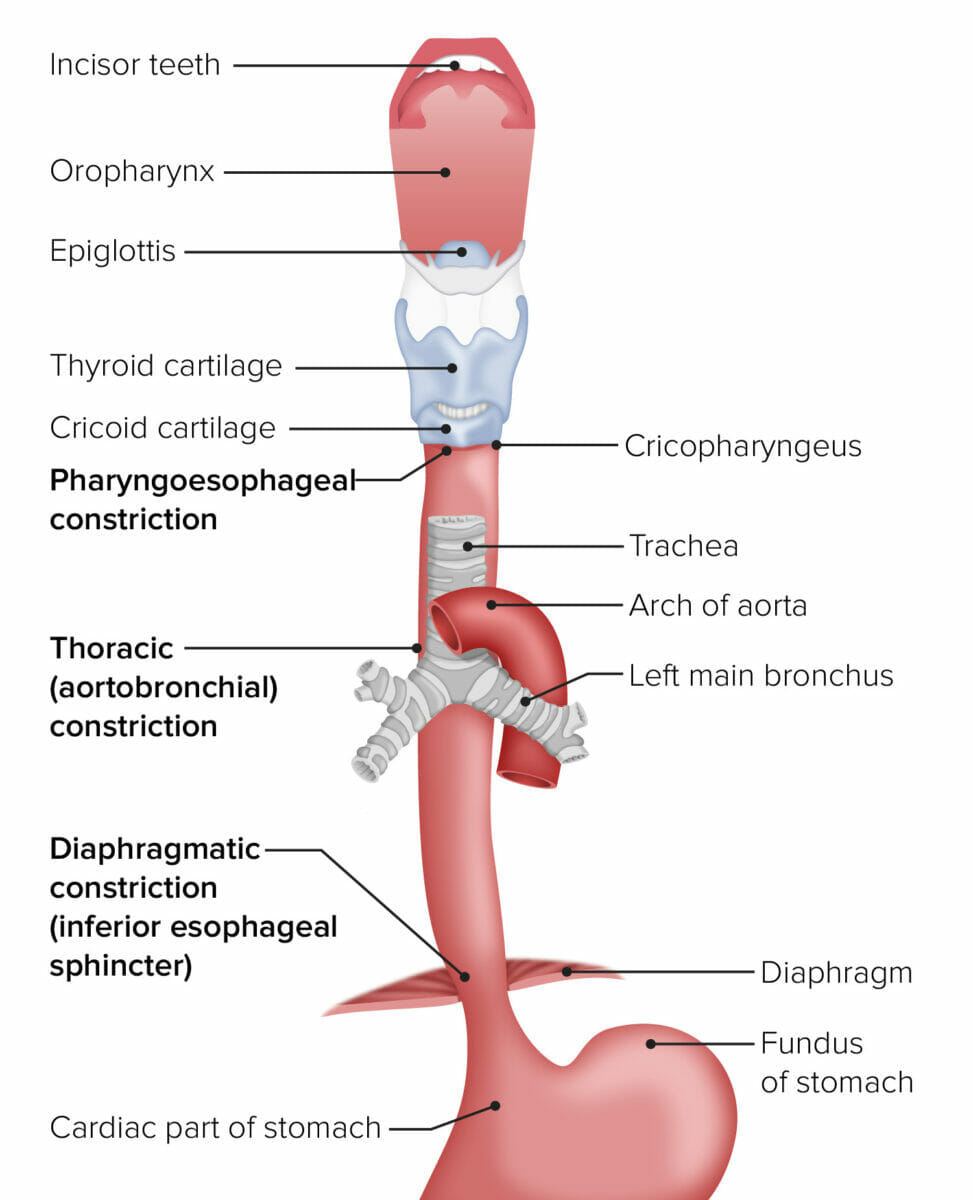
The esophagus in relation to other organs from the mouth to the stomach
Image by Lecturio.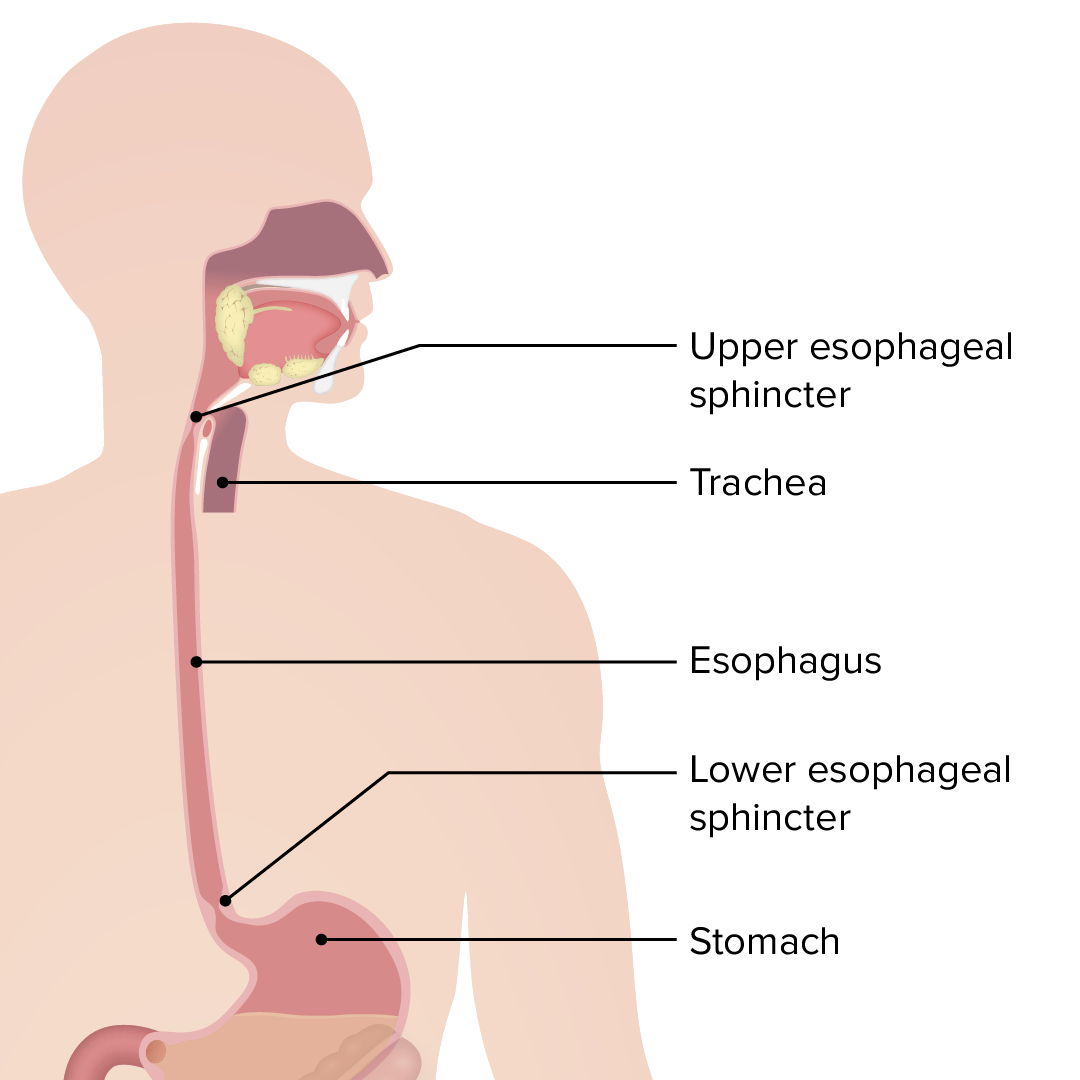
Esophagus: the upper esophageal sphincter controls the movement of food from the pharynx to the esophagus. The lower esophageal sphincter controls the movement of food from the esophagus to the stomach.
Image by Lecturio.Factors leading to increased exposure of esophageal mucosa Esophageal Mucosa Circular innermost layer of the esophagus wall that mediates esophageal peristalsis which pushes ingested food bolus toward the stomach. Esophagus: Anatomy to gastric acid/contents:
Pathophysiology of gastroesophageal reflux (GERD):
Left image (normal): The LES, a structure at the gastroesophageal junction, maintains a high-pressure zone between the esophagus and the stomach. This prevents the reflux of gastric contents. The LES relaxes transiently in response to meals.
Right image (GERD): An incompetent LES (lower baseline pressure) and increased frequency of TLESRs are among the factors causing GERD.
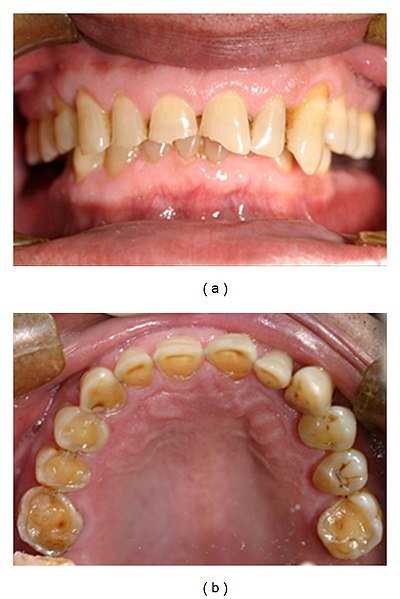
Frontal and maxillary occlusal views of severe tooth erosion caused by endogenous acid in a patient with GERD
Image: “Tooth erosion due to GERD” by Dr. A. Dickson. License: CC BY 2.5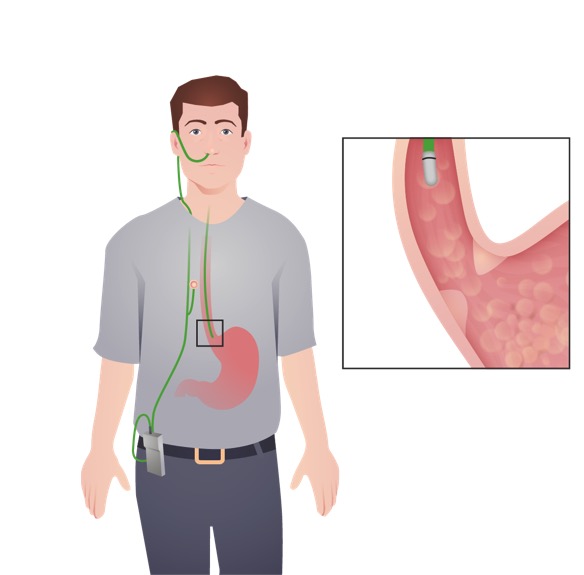
Ambulatory esophageal pH monitoring: This test aids in the diagnosis of GERD and evaluates the adequacy of treatment in those with persistent symptoms. In this image, the device with a pH sensor is placed transnasally, and is attached to a portable data recorder.
Image by Lecturio.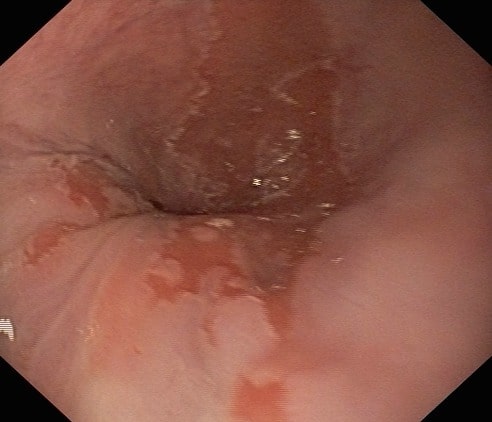
Esophagogastroduodenoscopy of a patient with persistent GERD: The image shows replacement of the squamous epithelium with columnar epithelium (Barrett esophagus).
Image: “Barretts esophagus” by US National Library of Medicine. License: CC BY 2.0
Nissen fundoplication: Gastric fundus is wrapped around the lower esophagus, causing narrowing of the gastroesophageal junction (GEJ).
Image by James P. Gray, PD.
Nissen fundoplication: Gastric fundus is wrapped around the lower esophagus, causing narrowing of the gastroesophageal junction (GEJ).
Image by James P. Gray, PD.
Upper gastrointestinal series: A severe stricture measuring 85 mm along the longitudinal axis was observed extending from the middle to lower thoracic esophagus caused by reflux esophagitis
Image: “Upper gastrointestinal series” by Department of Gastroenterological Surgery, Tokai University School of Medicine, 143 Shimokasuya, Isehara, Kanagawa, 259-1193, Japan. License: CC BY 4.0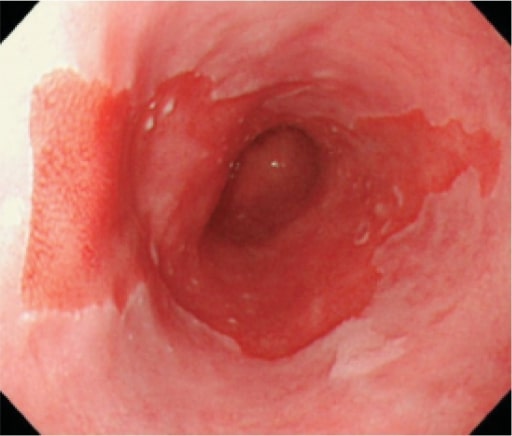
Long segment of Barrett esophagus
Image: “Long segment Barrett’s esophagus” by Japan Esophageal Society. License: CC BY 4.0The following conditions are differential diagnoses of GERD/reflux esophagitis Esophagitis Esophagitis is the inflammation or irritation of the esophagus. The major types of esophagitis are medication-induced, infectious, eosinophilic, corrosive, and acid reflux. Patients typically present with odynophagia, dysphagia, and retrosternal chest pain. Esophagitis: