Hydrocephalus Hydrocephalus Excessive accumulation of cerebrospinal fluid within the cranium which may be associated with dilation of cerebral ventricles, intracranial. Subarachnoid Hemorrhage is a potentially life-threatening condition caused by the excess accumulation of cerebrospinal fluid Cerebrospinal Fluid A watery fluid that is continuously produced in the choroid plexus and circulates around the surface of the brain; spinal cord; and in the cerebral ventricles. Ventricular System: Anatomy (CSF) within the ventricular system Ventricular System The ventricular system is an extension of the subarachnoid space into the brain consisting of a series of interconnecting spaces and channels. Four chambers are filled with cerebrospinal fluid (CSF): the paired lateral ventricles, the unpaired 3rd ventricle, and the unpaired 4th ventricle. Ventricular System: Anatomy. Hydrocephalus Hydrocephalus Excessive accumulation of cerebrospinal fluid within the cranium which may be associated with dilation of cerebral ventricles, intracranial. Subarachnoid Hemorrhage can be classified as communicating, which is caused by either impaired CSF absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption or excess CSF production; or non-communicating, which is caused by a structural blockage in CSF flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure. The causes of hydrocephalus Hydrocephalus Excessive accumulation of cerebrospinal fluid within the cranium which may be associated with dilation of cerebral ventricles, intracranial. Subarachnoid Hemorrhage can be congenital or acquired. The clinical presentation is often nonspecific with symptoms including headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess, behavioral changes, developmental delays, or nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics and vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia. If the hydrocephalus Hydrocephalus Excessive accumulation of cerebrospinal fluid within the cranium which may be associated with dilation of cerebral ventricles, intracranial. Subarachnoid Hemorrhage is congenital or acquired at a young age, infants often present with macrocephaly Macrocephaly Cowden Syndrome. Diagnosis is confirmed with neuroimaging Neuroimaging Non-invasive methods of visualizing the central nervous system, especially the brain, by various imaging modalities. Febrile Infant (ultrasound, computed tomography of the head, or magnetic resonance imaging) showing ventriculomegaly. Treatment is most commonly surgical with the placement of a CSF shunt.
Last updated: Feb 16, 2026
There are different ways to characterize hydrocephalus Hydrocephalus Excessive accumulation of cerebrospinal fluid within the cranium which may be associated with dilation of cerebral ventricles, intracranial. Subarachnoid Hemorrhage, each of which can help physicians Physicians Individuals licensed to practice medicine. Clinician–Patient Relationship better understand the underlying cause and determine the appropriate treatment.
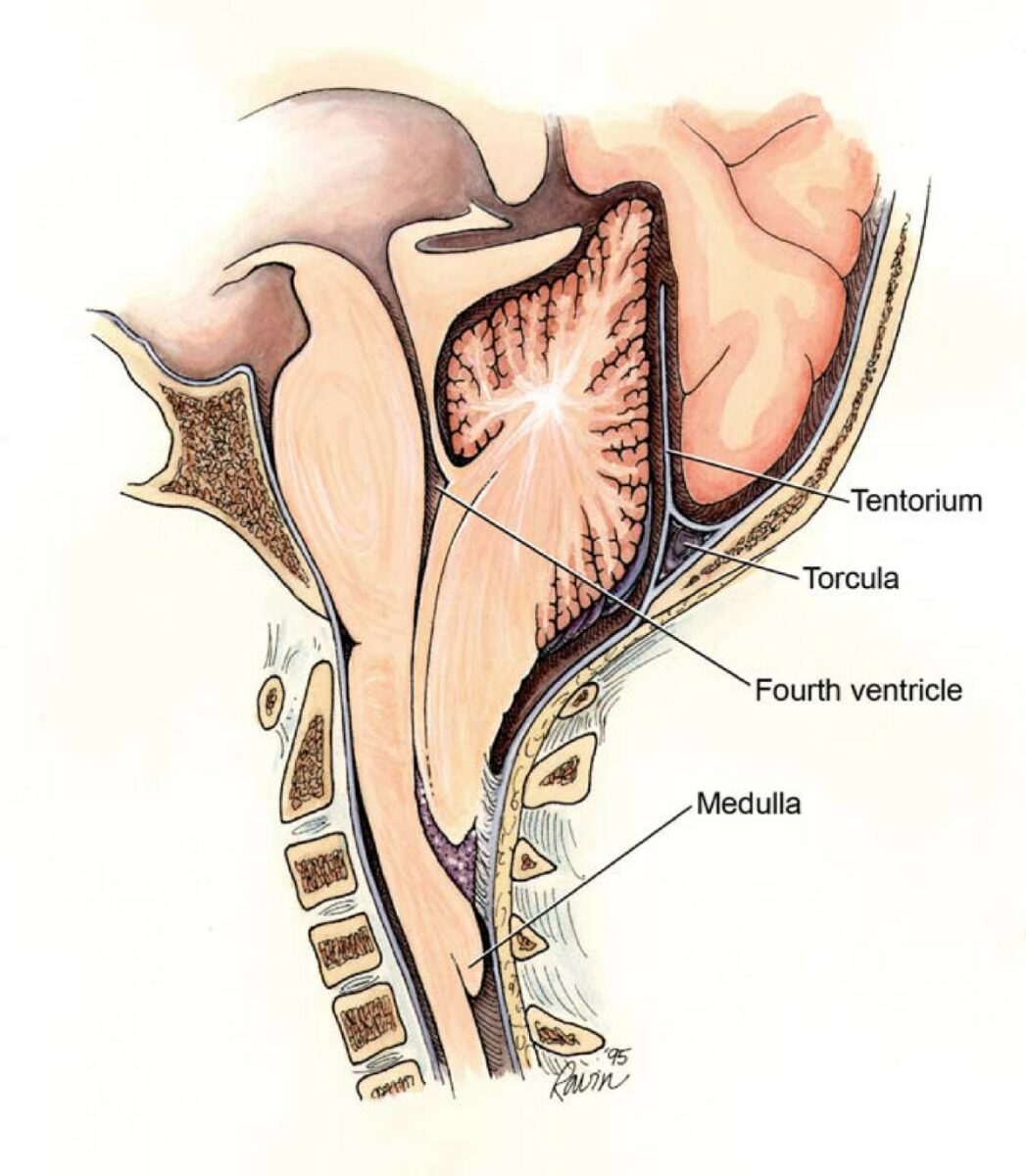
Chiari II malformation showing the points of potential obstruction that yield different subtypes of hydrocephalus
Image: “Chiari2” by Rekate HL. License: CC BY 2.0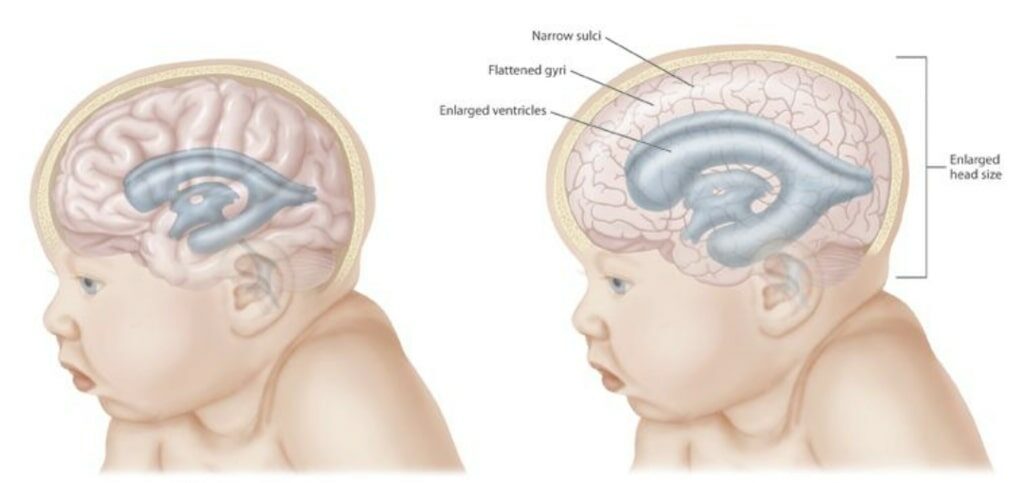
An infant with normal intracranial pressure (left), and a child with hydrocephalus (right)
Image: “Hydrocephalus CDC” by CDC. License: Public Domain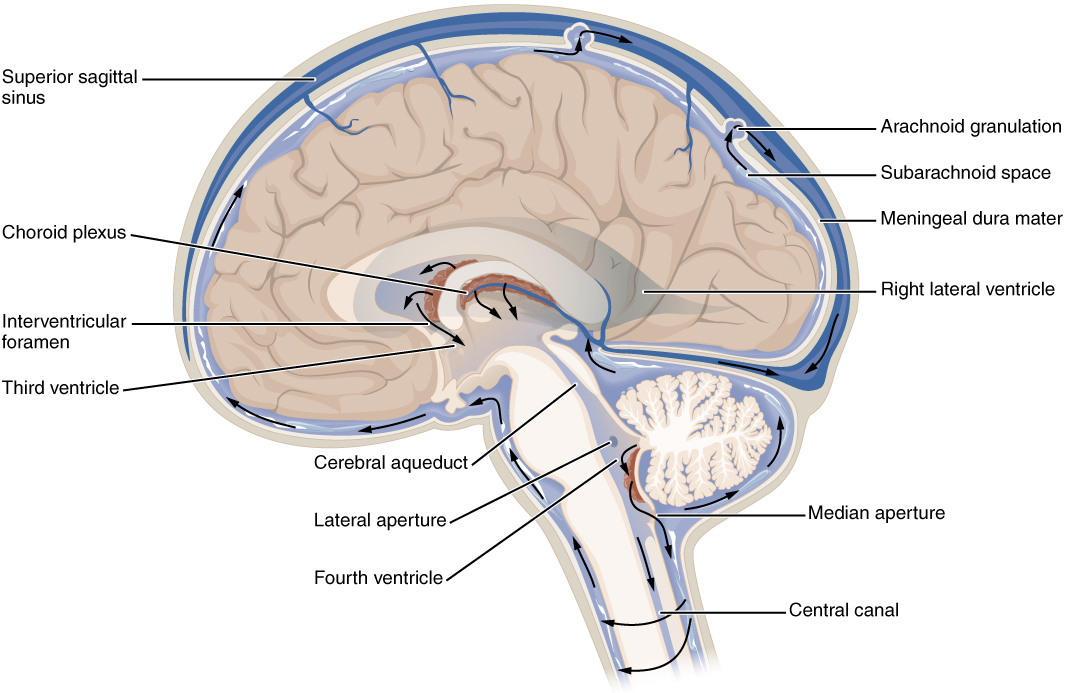
Normal CSF production: CSF is produced in the choroid plexus of the ventricles → circulates through the ventricular system → 4th ventricle → subarachnoid space → absorbed by arachnoid villi (located in the subarachnoid space) → venous sinuses + systemic circulation
Image: “CFS_Circulation” by OpenStax. License: CC BY 4.0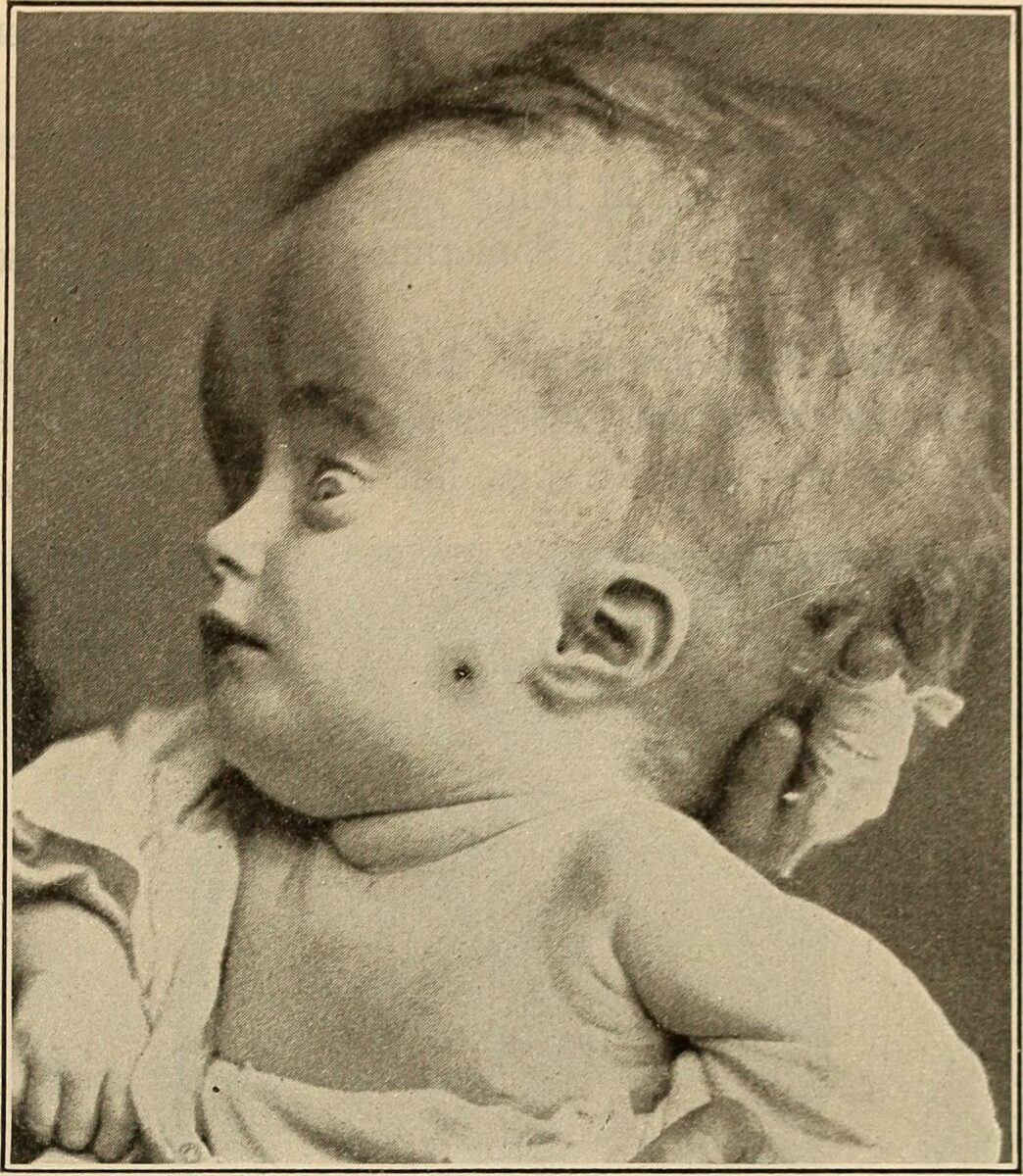
Photo of a child with hydrocephalus and a noticeable “setting sun” sign
Image: “Sunset sign” by Louis Fischer. License: Public Domain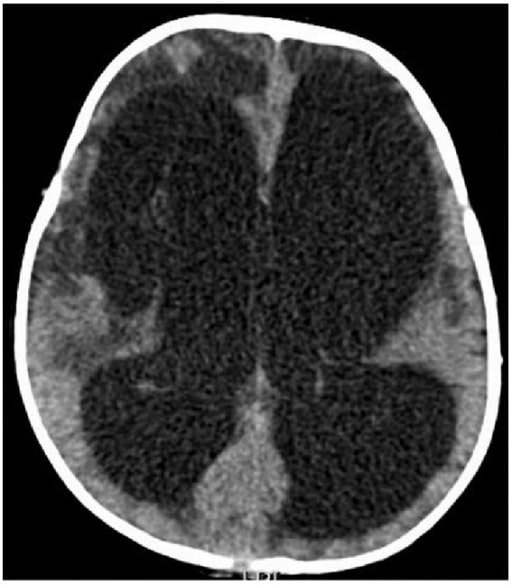
Non-enhanced brain computed tomography scan of a 7-month-old boy with a history of pneumococcal meningitis. Axial image shows significant non-obstructive hydrocephalus resulting in compression of cerebral parenchyma. There are hypodensities involving the periventricular regions and the frontal lobes bilaterally with associated cystic encephalomalacia, especially on the right.
Image: “Nonenhanced brain computed tomography scan” by Division of Neurology, Department of Pediatrics and Adolescent Medicine, American University of Beirut Medical Center, P.O. Box 11-0236, Riad El Solh, Beirut 1107 2020, Lebanon. License: CC BY 3.0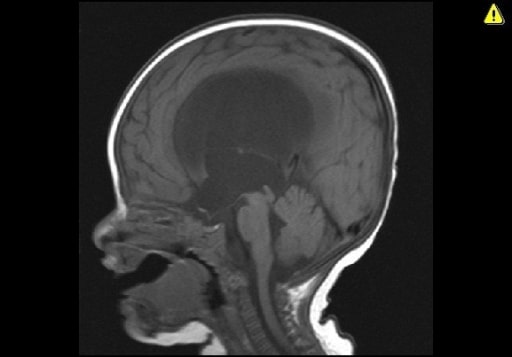
Sagittal T1-weighted MRI demonstrating obstructive hydrocephalus due to congenital aqueductal stenosis.
Image: “Obstructive hydrocephalus” by Division of Neurosurgery, Faculty of Medicine, King Abdulaziz University, PO Box 80215, Jeddah, 21589, Saudi Arabia. License: CC BY 2.0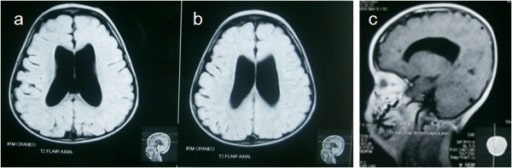
MRI of head showing supratentorial non-communicating hydrocephalus (a, b) and slightly hypoplastic corpus callosum (c).
Image: “Magnetic Resonance of head” by Laboratorio de Inmunología y Biología Molecular, Doctorado en Biotecnología, Facultad de Ciencias Químico Biológicas, Universidad Autónoma de Sinaloa, Culiacán, Sinaloa, México. License: CC BY 2.0Any patient with hydrocephalus Hydrocephalus Excessive accumulation of cerebrospinal fluid within the cranium which may be associated with dilation of cerebral ventricles, intracranial. Subarachnoid Hemorrhage and symptoms of ICP ICP Normal intracranial pressure (ICP) is defined as < 15 mm Hg, whereas pathologically increased ICP is any pressure ≥ 20 mm Hg. Increased ICP may result from several etiologies, including trauma, intracranial hemorrhage, mass lesions, cerebral edema, increased CSF production, and decreased CSF absorption. Increased Intracranial Pressure (ICP) requires intervention. The method used to relieve the pressure and the speed at which it is deployed is based on the severity of the patient’s ICP ICP Normal intracranial pressure (ICP) is defined as < 15 mm Hg, whereas pathologically increased ICP is any pressure ≥ 20 mm Hg. Increased ICP may result from several etiologies, including trauma, intracranial hemorrhage, mass lesions, cerebral edema, increased CSF production, and decreased CSF absorption. Increased Intracranial Pressure (ICP).
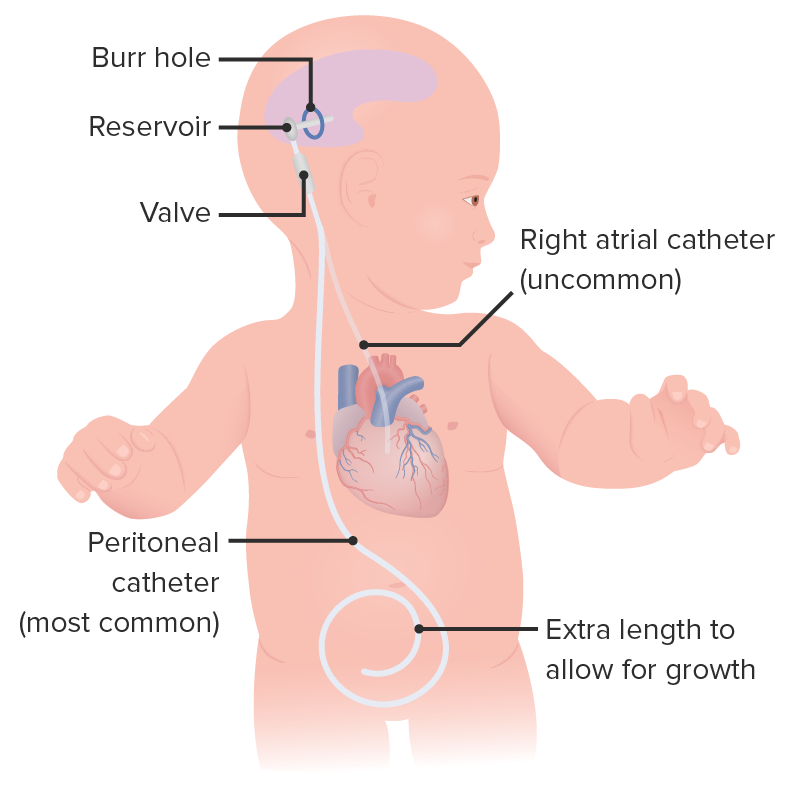
A diagram of a ventriculoperitoneal shunt in a baby
Image by Lecturio.Mnemonic
“Don’t pump Pump ACES and RUSH: Resuscitation Ultrasound Protocols the shunt unless you’re stuck.”: The shunt pump Pump ACES and RUSH: Resuscitation Ultrasound Protocols should be accessed as little as possible.
The differential diagnosis of hydrocephalus Hydrocephalus Excessive accumulation of cerebrospinal fluid within the cranium which may be associated with dilation of cerebral ventricles, intracranial. Subarachnoid Hemorrhage includes: