Female sexual dysfunction Sexual dysfunction Physiological disturbances in normal sexual performance in either the male or the female. Sexual Physiology represents a variety of disorders in any part of the sexual response cycle, including desire disorders, arousal disorders, orgasmic disorders, and pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways disorders. The condition may result from stresses and interpersonal conflicts as well as physical illness or medication/substance use. These disorders cause significant distress to the patient and her partner. Treatment options include psychotherapy Psychotherapy Psychotherapy is interpersonal treatment based on the understanding of psychological principles and mechanisms of mental disease. The treatment approach is often individualized, depending on the psychiatric condition(s) or circumstance. Psychotherapy, physical therapy Physical Therapy Becker Muscular Dystrophy, and pharmacotherapy.
Last updated: Dec 15, 2025
Sexual dysfunction Sexual dysfunction Physiological disturbances in normal sexual performance in either the male or the female. Sexual Physiology (in males or females) arises from problems involving any stage of the sexual response cycle.
The female sexual response cycle is non-linear and more complex than the male sexual response, with additional factors such as emotional intimacy.
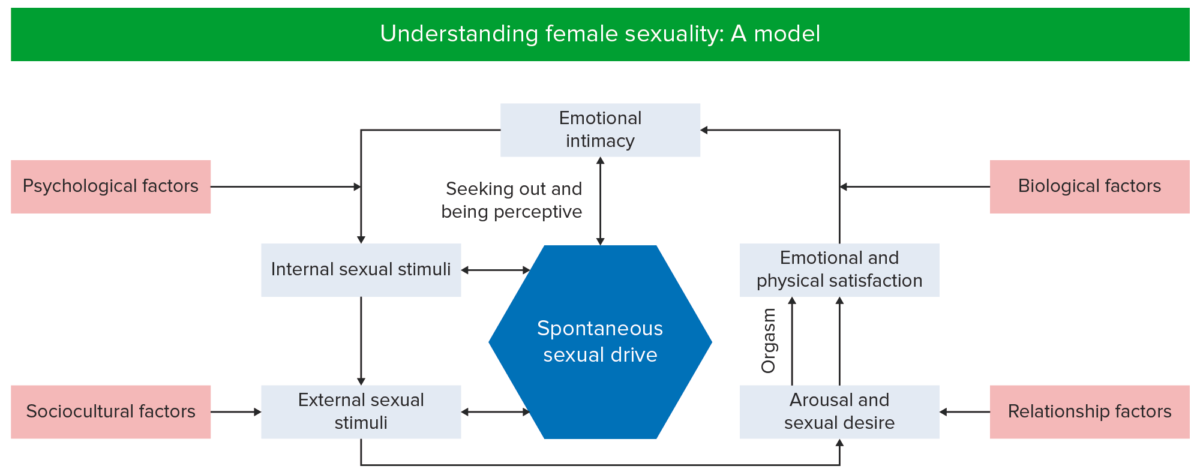
A model of female sexuality. A problem that consistently impairs sexual arousal or functioning at any point in this cycle may cause sexual dysfunction.
Image by Lecturio.| Stage of sexual response | Changes in females | Changes in males | Changes in both |
|---|---|---|---|
| Desire |
|
||
| Excitement/arousal |
|
|
|
| Orgasm | Vaginal and uterine contractions |
|
|
| Resolution | Women experience little or no refractory period. | Men have a refractory period lasting minutes to hours, during which they cannot re-experience orgasm. |
|
Before turning toward the diagnosis of a psychiatric condition, anatomic or physiologic causes should be ruled out via laboratory or radiologic imaging.
The diagnosis of female sexual dysfunction Sexual dysfunction Physiological disturbances in normal sexual performance in either the male or the female. Sexual Physiology and its types is made by clinical observation based on the type of symptoms presented, their severity, and duration.
| Female sexual interest/arousal disorder | Female orgasmic disorder | Genitopelvic pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways/ penetration Penetration X-rays disorder (formerly dyspareunia Dyspareunia Recurrent genital pain occurring during, before, or after sexual intercourse in either the male or the female. Primary Ovarian Insufficiency and vaginismus) |
|---|---|---|
|
|
|
The following conditions are differential diagnoses of female sexual dysfunction Sexual dysfunction Physiological disturbances in normal sexual performance in either the male or the female. Sexual Physiology: