The peritoneum is a serous membrane lining the abdominopelvic cavity. This lining is formed by connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology and originates from the mesoderm Mesoderm The middle germ layer of an embryo derived from three paired mesenchymal aggregates along the neural tube. Gastrulation and Neurulation. The membrane lines both the abdominal walls (as parietal Parietal One of a pair of irregularly shaped quadrilateral bones situated between the frontal bone and occipital bone, which together form the sides of the cranium. Skull: Anatomy peritoneum) and all of the visceral organs (as visceral peritoneum). The peritoneum supports and suspends the organs within the abdominal cavity and provides an important conduit for the neurovasculature supplying these organs. There are several peritoneal folds, known as mesenteries, omenta, and ligaments. The greater and lesser omenta divide the peritoneal cavity into greater and lesser sacs, which are important anatomic spaces within the cavity. Organs located behind the posterior parietal Parietal One of a pair of irregularly shaped quadrilateral bones situated between the frontal bone and occipital bone, which together form the sides of the cranium. Skull: Anatomy peritoneum are known as retroperitoneal, while organs that protrude into the cavity and are fully covered by visceral peritoneum are known as intraperitoneal.
Last updated: Dec 15, 2025
The peritoneum is a serous membrane lining the abdominopelvic cavity and covering its organs.
The peritoneum develops from the mesoderm Mesoderm The middle germ layer of an embryo derived from three paired mesenchymal aggregates along the neural tube. Gastrulation and Neurulation of the trilaminar embryo Embryo The entity of a developing mammal, generally from the cleavage of a zygote to the end of embryonic differentiation of basic structures. For the human embryo, this represents the first two months of intrauterine development preceding the stages of the fetus. Fertilization and First Week:
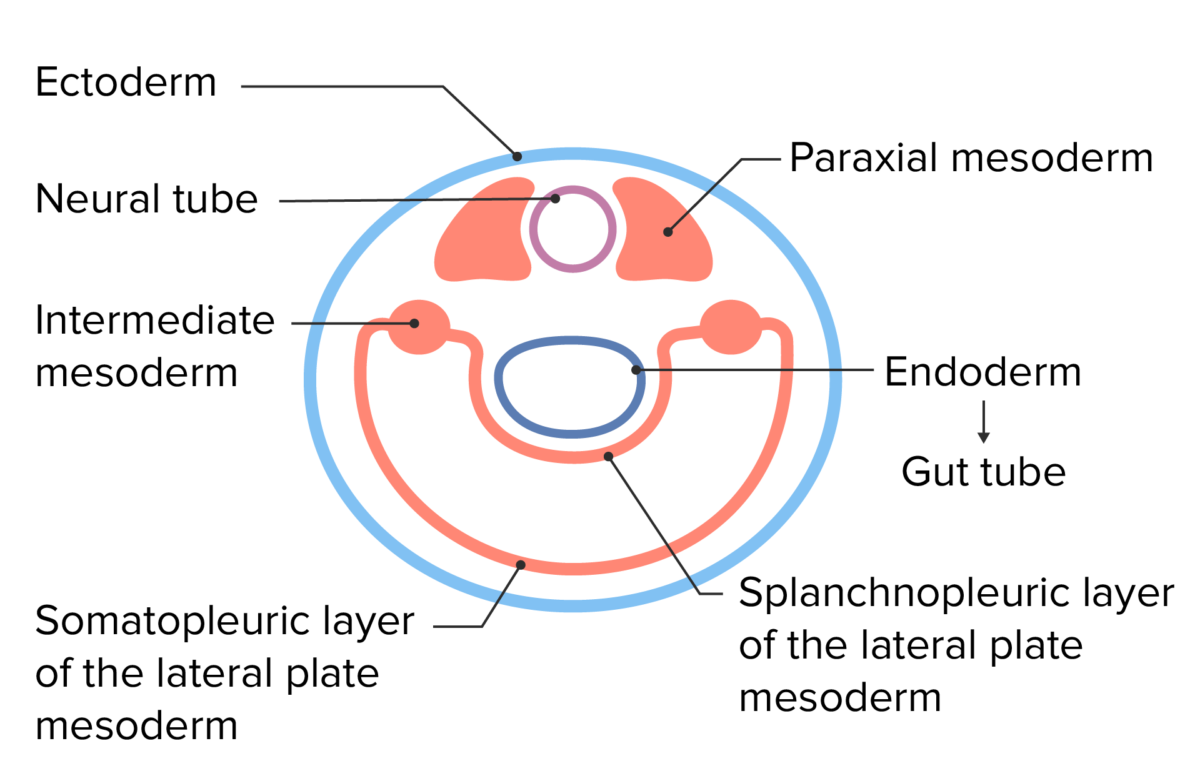
Embryonic cell layers following lateral folding of the trilaminar disc
Image by Lecturio.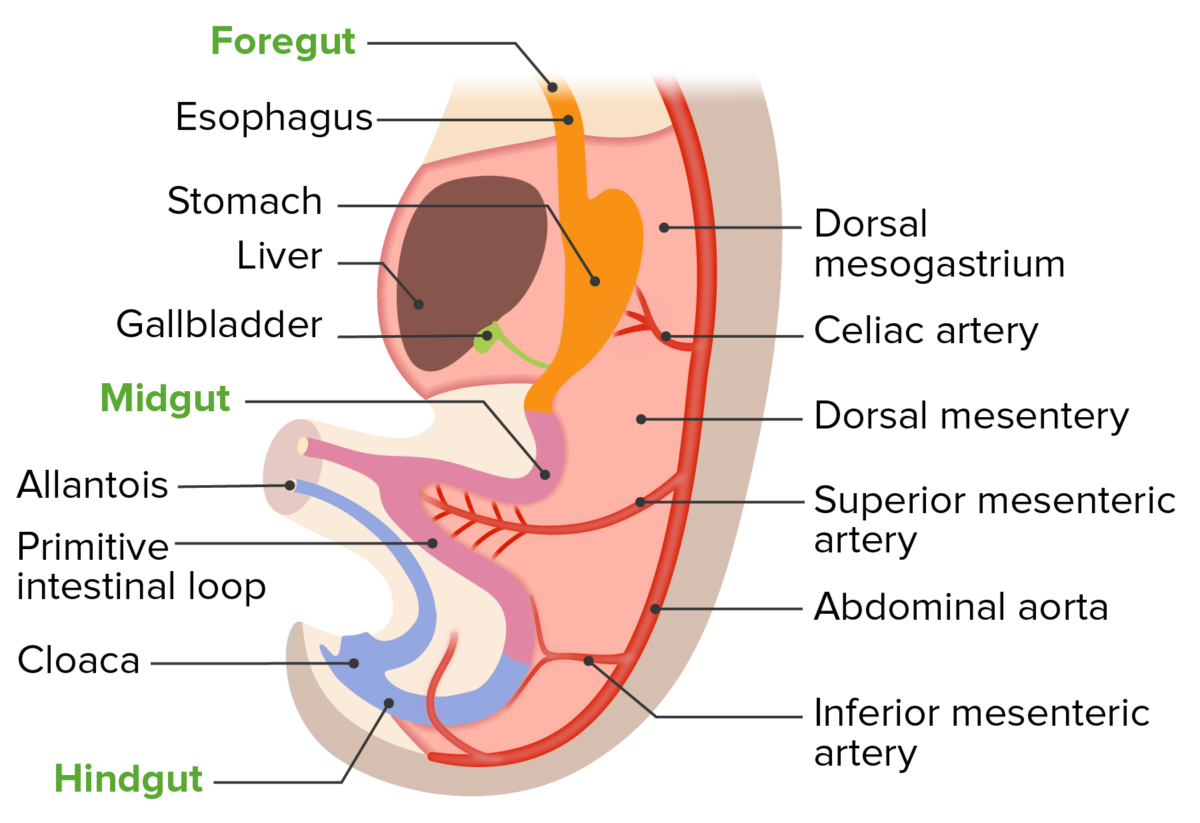
Development of the dorsal mesentery with the primitive gut tube
Image by Lecturio.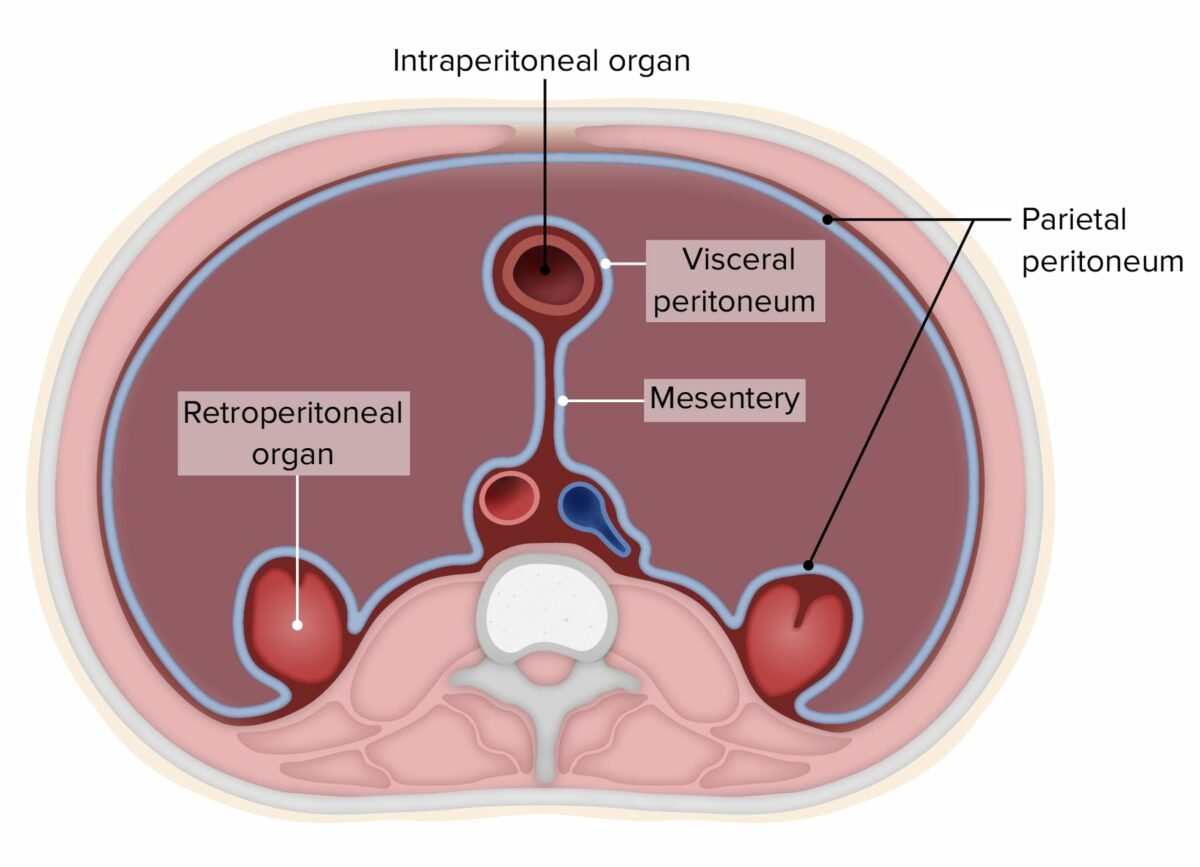
Diagram of the peritoneum (abdominal organs removed to more clearly demonstrate the concepts)
Image by Lecturio.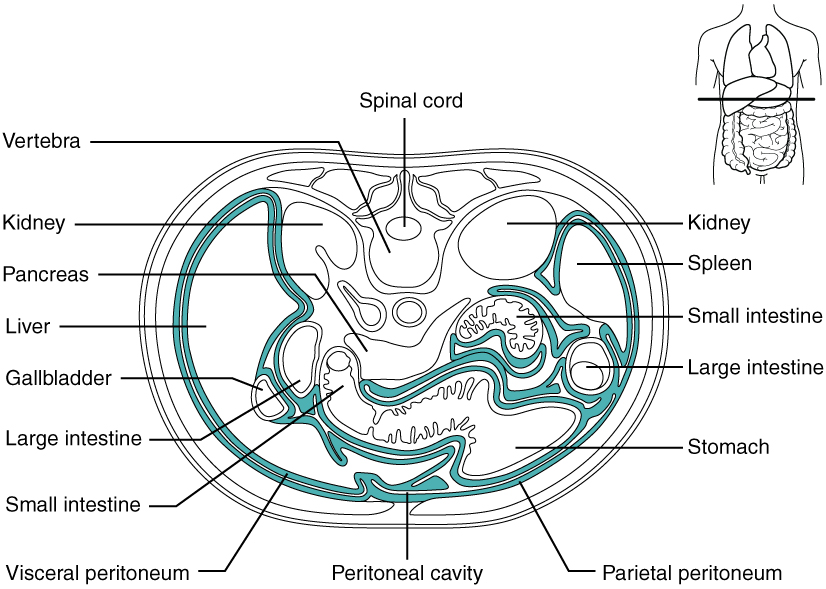
Diagram of the peritoneal cavity
Image: “Illustration from Anatomy & Physiology, Connexions Web site” by OpenStax College. License: CC BY 3.0Organs can be classified according to their peritoneal coverage:
| Location | Organs |
|---|---|
| Intraperitoneal |
|
| Secondarily retroperitoneal |
|
| Primary retroperitoneal |
|
| Subperitoneal |
|
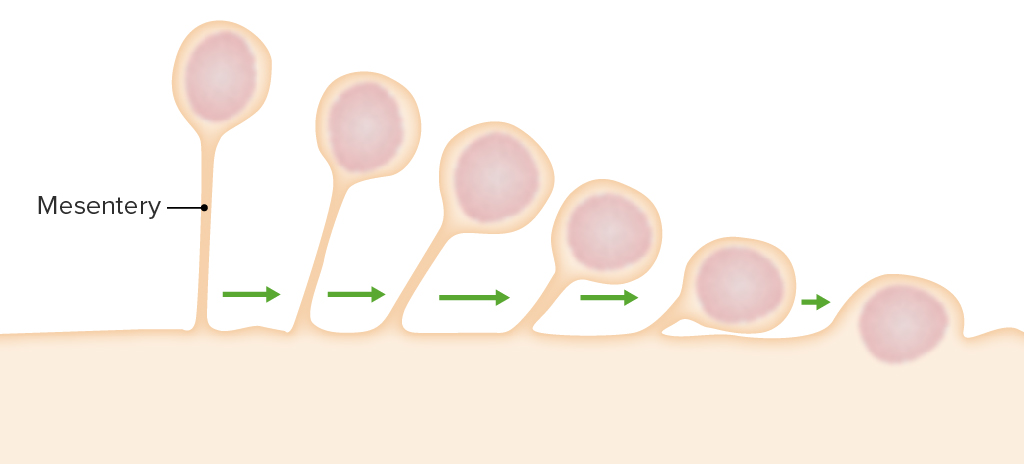
Development of secondarily retroperitoneal organs:
These organs begin suspended by a mesentery. However, as the organ develops, the mesentery regresses until the organ is flush with the posterior wall and ends up as a retroperitoneal organ.
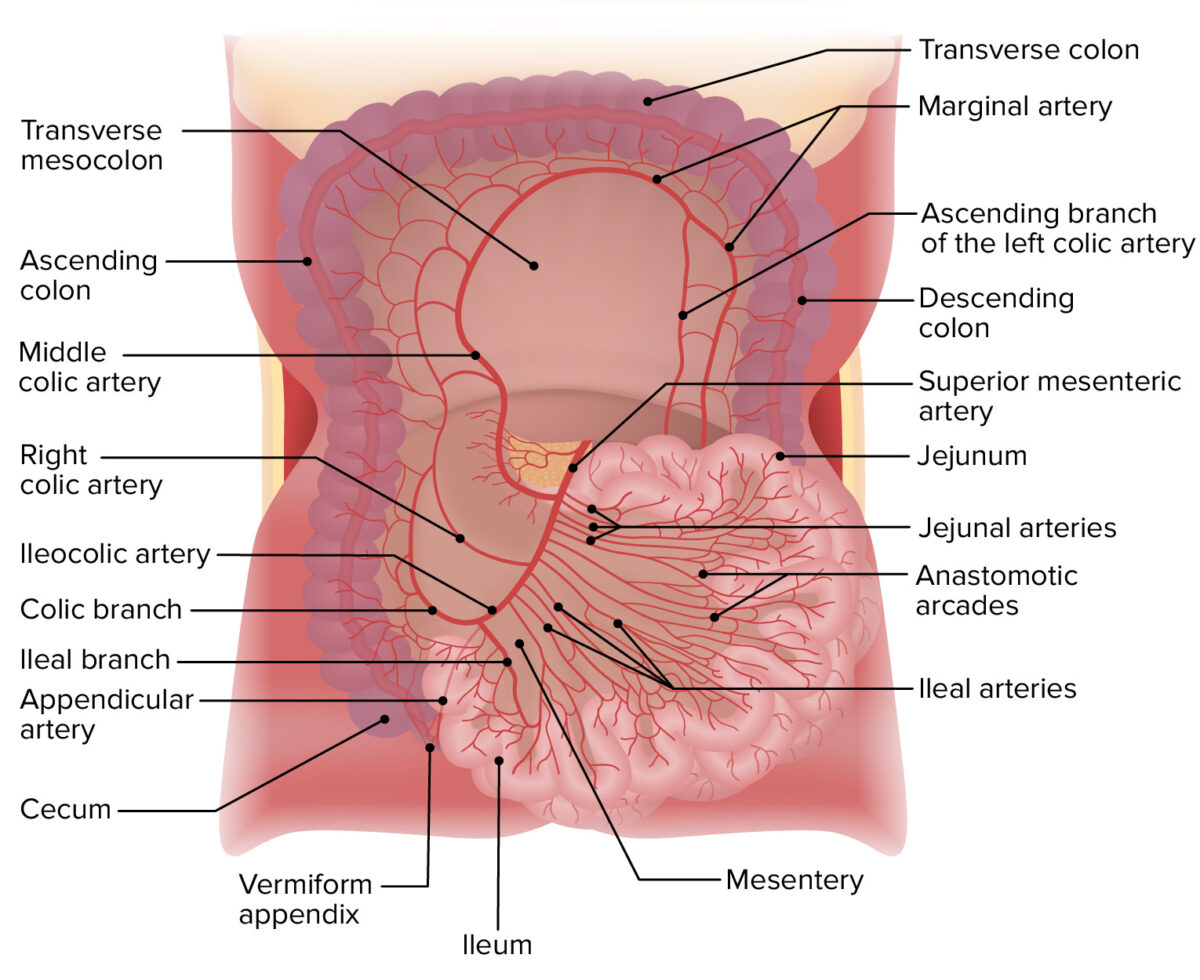
Arterial supply of the jejunum and ileum
Image by Lecturio.The omenta are layered sheets of peritoneum. The greater omentum and the lesser omentum are the 2 omenta.
Greater omentum:
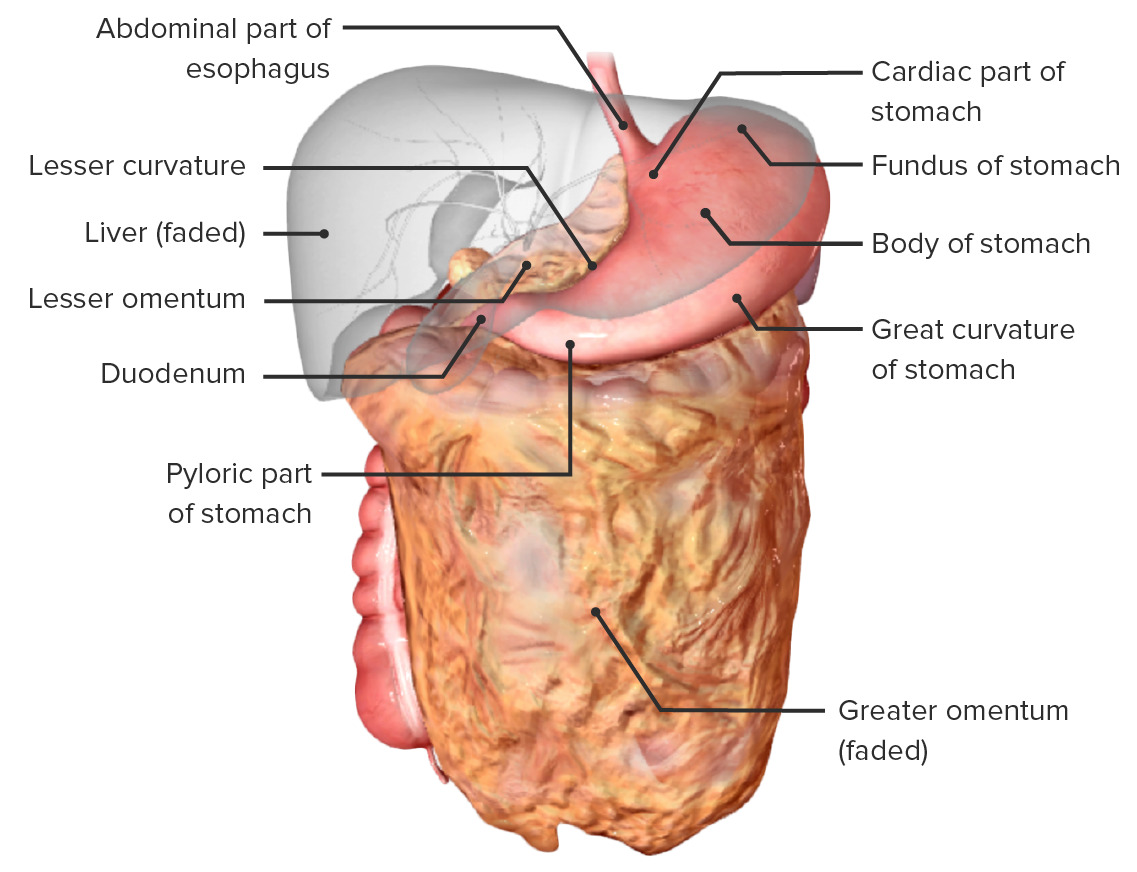
Stomach in situ and the relations to its neighboring structures:
Note the greater and lesser omenta continuing from the greater and lesser curvatures of the stomach, respectively.
Lesser omentum:
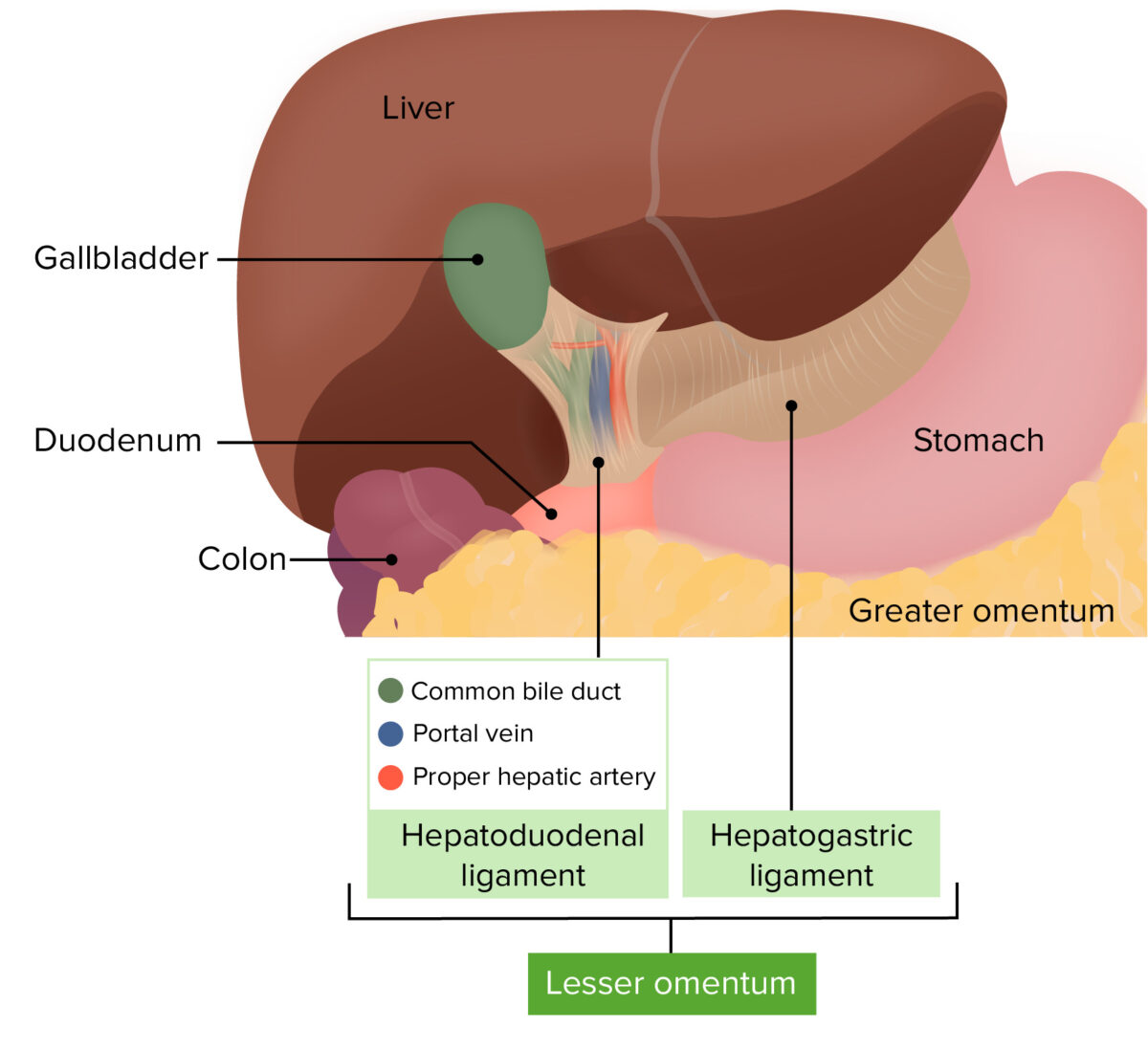
Lesser omentum and omental foramen in situ
Image by Lecturio.The peritoneal cavity is divided into several different compartments by the omenta and transverse mesocolon:
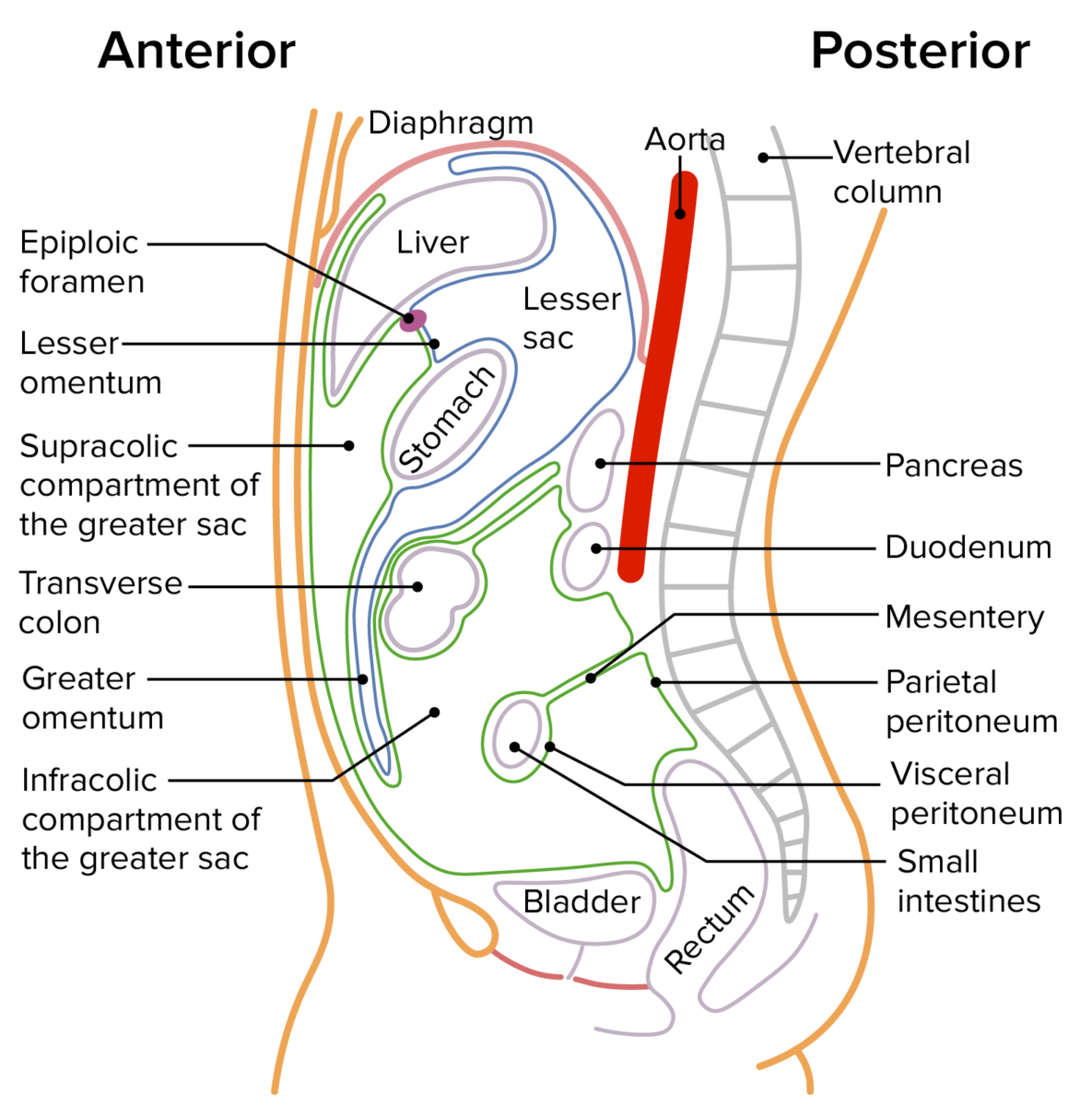
A sagittal section through the abdomen depicting the greater and lesser sacs:
The greater sac is outlined in green, and the lesser sac is outlined in blue.
The greater sac is divided into 2 compartments by the transverse mesocolon.
The lesser sac is also known as the omental bursa.
| Parietal Parietal One of a pair of irregularly shaped quadrilateral bones situated between the frontal bone and occipital bone, which together form the sides of the cranium. Skull: Anatomy peritoneum | Visceral peritoneum | |
|---|---|---|
| Arterial supply | From the abdominal wall Abdominal wall The outer margins of the abdomen, extending from the osteocartilaginous thoracic cage to the pelvis. Though its major part is muscular, the abdominal wall consists of at least seven layers: the skin, subcutaneous fat, deep fascia; abdominal muscles, transversalis fascia, extraperitoneal fat, and the parietal peritoneum. Surgical Anatomy of the Abdomen vasculature | Superior and inferior mesenteric arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology |
| Venous drainage | Veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology drain into the inferior vena cava Inferior vena cava The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy | Veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology drain into the portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy |
| Innervation | Somatic innervation from spinal nerves Spinal nerves The 31 paired peripheral nerves formed by the union of the dorsal and ventral spinal roots from each spinal cord segment. The spinal nerve plexuses and the spinal roots are also included. Spinal Cord: Anatomy T10–L1 ( pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways can be localized) | Autonomic innervation ( pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways is difficult to localize) |