The arm, or "upper arm" in common usage, is the region of the upper limb that extends from the shoulder to the elbow joint Elbow joint The elbow is the synovial hinge joint between the humerus in the upper arm and the radius and ulna in the forearm. The elbow consists of 3 joints, which form a functional unit enclosed within a single articular capsule. The elbow is the link between the powerful motions of the shoulder and the intricate fine-motor function of the hand. Elbow Joint: Anatomy and connects inferiorly to the forearm Forearm The forearm is the region of the upper limb between the elbow and the wrist. The term "forearm" is used in anatomy to distinguish this area from the arm, a term that is commonly used to describe the entire upper limb. The forearm consists of 2 long bones (the radius and the ulna), the interosseous membrane, and multiple arteries, nerves, and muscles. Forearm: Anatomy through the cubital fossa Cubital Fossa The cubital fossa is the region anterior to the elbow joint. The cubital fossa is seen as the triangular depression between the brachioradialis and pronator teres muscles. The 4 important structures of the cubital fossa (from lateral to medial) are the radial nerve, tendon of the biceps brachii muscle, brachial artery, and median nerve. Cubital Fossa: Anatomy. It is divided into 2 fascial compartments (anterior and posterior) and houses numerous structures, including the humerus; the brachial and profunda brachii arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology; the basilic, cephalic, and brachial veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology; the radial, median, ulnar, and musculocutaneous nerves; and the flexor and extensor muscles of the arm.
Last updated: Jan 12, 2024
The humerus can be divided into 3 parts: the proximal end, the shaft, and the distal end.
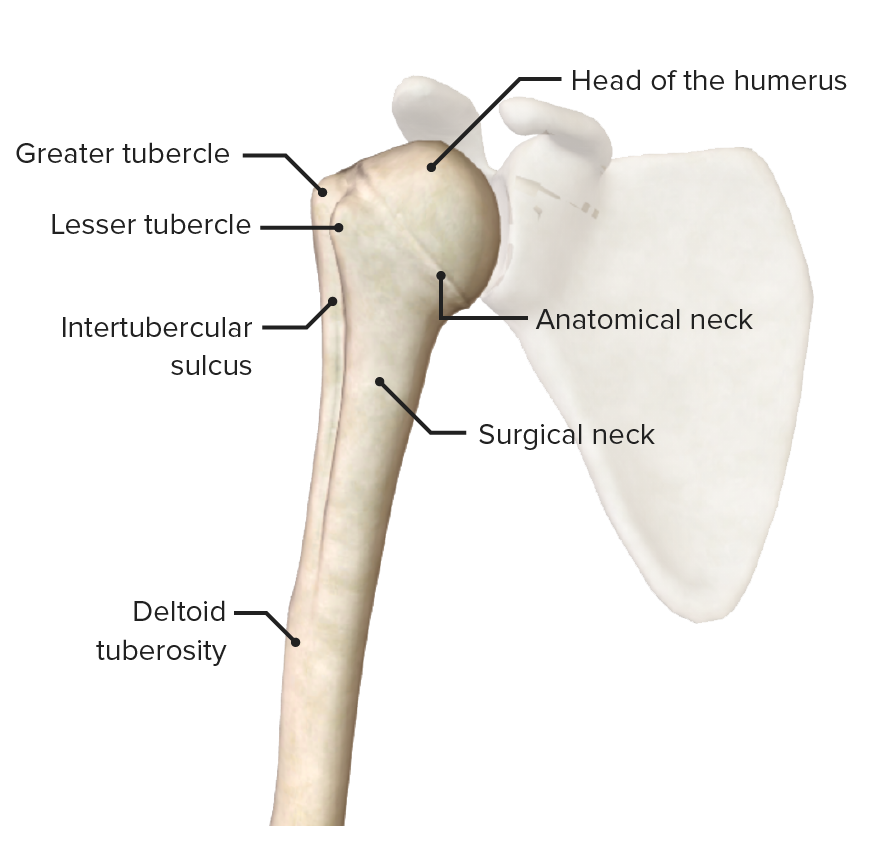
Proximal end of the humerus
Image by BioDigital, edited by Lecturio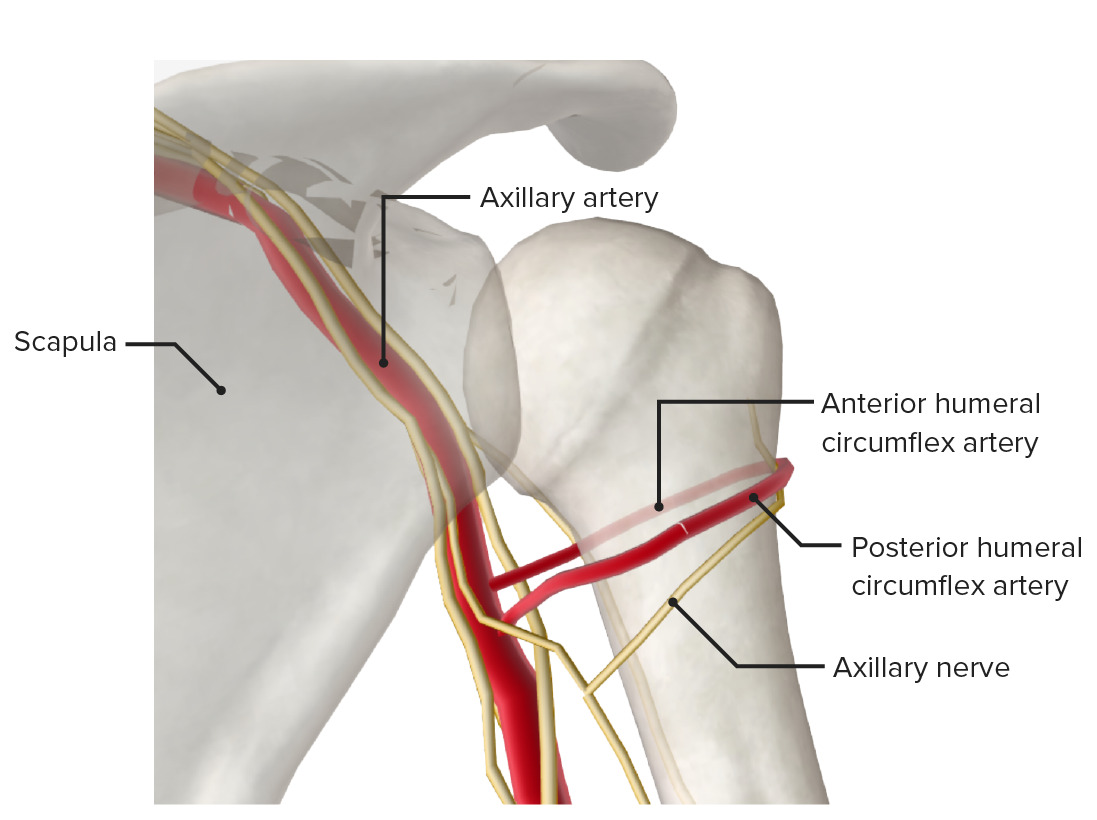
Posterior view of the proximal end of the humerus featuring the surgical neck, a frequent site of fracture. A fracture here may injure the axillary nerve and/or posterior circumflex artery.
Image by BioDigital, edited by Lecturio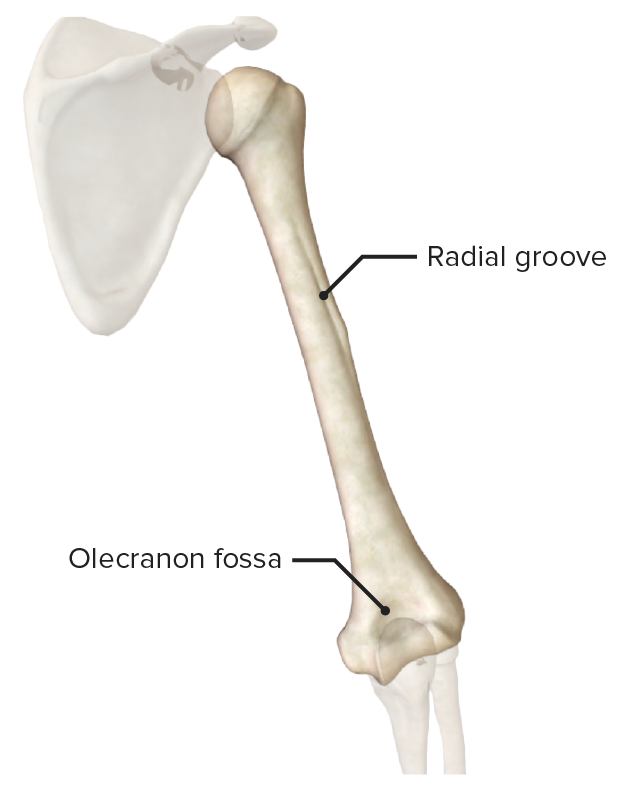
Posterior view of the humerus
Image by BioDigital, edited by Lecturio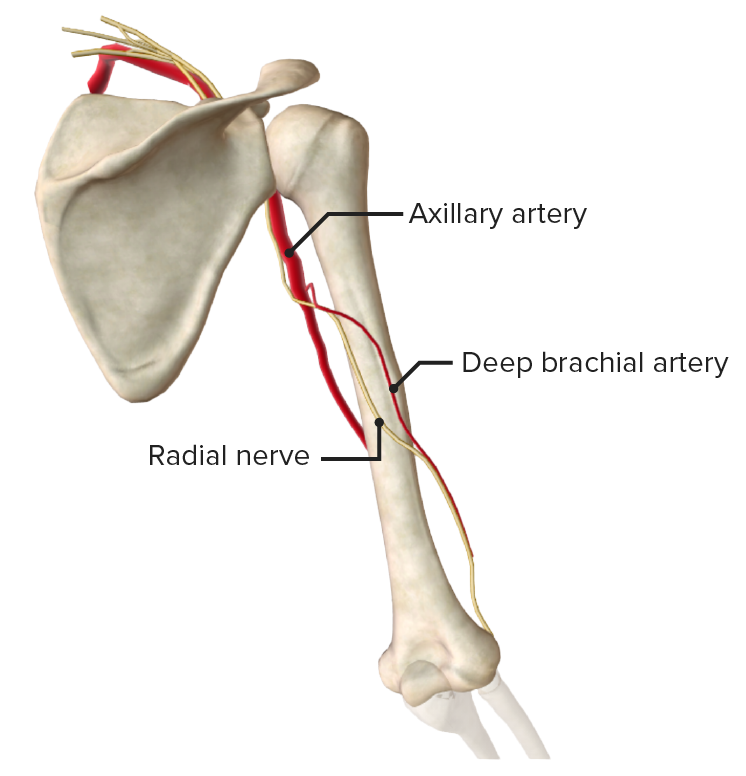
Posterior view of the humerus featuring the radial or spiral groove. The radial nerve runs in this groove and may be injured secondary to pressure or trauma, with resultant wrist drop.
Image by BioDigital, edited by Lecturio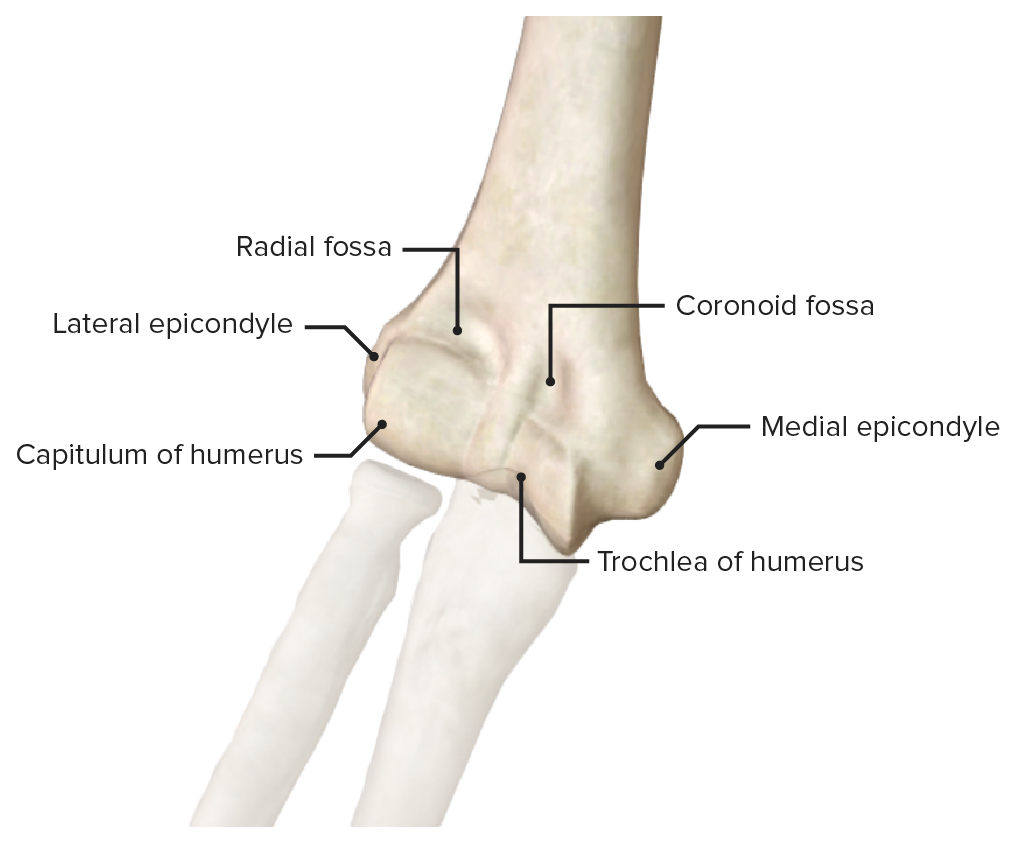
Anterior view of the distal end of the humerus
Image by BioDigital, edited by Lecturio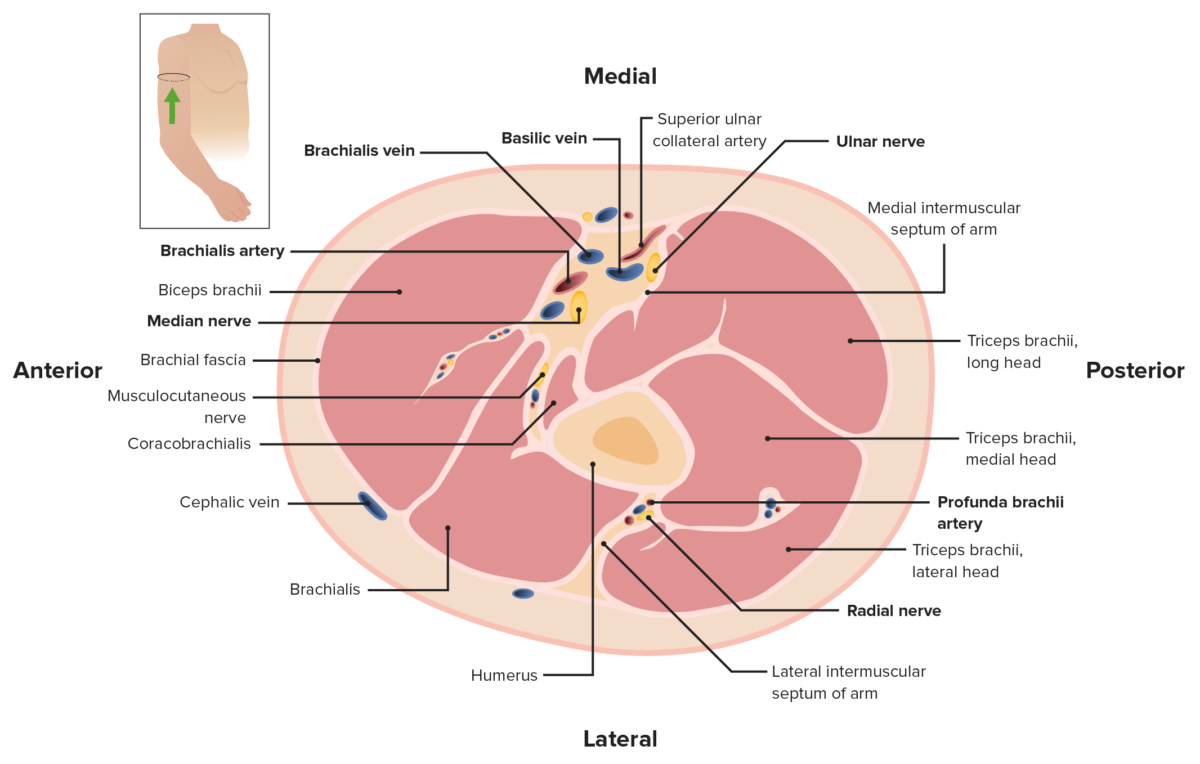
Cross-section of the arm, featuring the anterior and posterior compartments. Note the brachial fascia enclosing all of the muscles and forming the lateral and medial intermuscular septa.
Image by Lecturio. License: CC BY-NC-SA 4.0| Muscle | Origin | Insertion | Innervation | Function |
|---|---|---|---|---|
| Biceps brachii |
|
Radial tuberosity and forearm Forearm The forearm is the region of the upper limb between the elbow and the wrist. The term “forearm” is used in anatomy to distinguish this area from the arm, a term that is commonly used to describe the entire upper limb. The forearm consists of 2 long bones (the radius and the ulna), the interosseous membrane, and multiple arteries, nerves, and muscles. Forearm: Anatomy fascia Fascia Layers of connective tissue of variable thickness. The superficial fascia is found immediately below the skin; the deep fascia invests muscles, nerves, and other organs. Cellulitis via bicipital aponeurosis | Musculocutaneous nerve Musculocutaneous Nerve A major nerve of the upper extremity. The fibers of the musculocutaneous nerve originate in the lower cervical spinal cord (usually C5 to C7), travel via the lateral cord of the brachial plexus, and supply sensory and motor innervation to the upper arm, elbow, and forearm. Axilla and Brachial Plexus: Anatomy (C6) |
|
| Brachialis | Lateral and medial surface of distal half of humerus | Coronoid process and tuberosity of ulna Ulna The inner and longer bone of the forearm. Forearm: Anatomy | Musculocutaneous nerve Musculocutaneous Nerve A major nerve of the upper extremity. The fibers of the musculocutaneous nerve originate in the lower cervical spinal cord (usually C5 to C7), travel via the lateral cord of the brachial plexus, and supply sensory and motor innervation to the upper arm, elbow, and forearm. Axilla and Brachial Plexus: Anatomy (C6) | Flexes elbow joint Elbow joint The elbow is the synovial hinge joint between the humerus in the upper arm and the radius and ulna in the forearm. The elbow consists of 3 joints, which form a functional unit enclosed within a single articular capsule. The elbow is the link between the powerful motions of the shoulder and the intricate fine-motor function of the hand. Elbow Joint: Anatomy |
| Coracobrachialis | Coracoid process | Middle 3rd of humerus | Musculocutaneous nerve Musculocutaneous Nerve A major nerve of the upper extremity. The fibers of the musculocutaneous nerve originate in the lower cervical spinal cord (usually C5 to C7), travel via the lateral cord of the brachial plexus, and supply sensory and motor innervation to the upper arm, elbow, and forearm. Axilla and Brachial Plexus: Anatomy (C6) | Flexes/adducts shoulder joint Shoulder joint The articulation between the head of the humerus and the glenoid cavity of the scapula. Examination of the Upper Limbs |
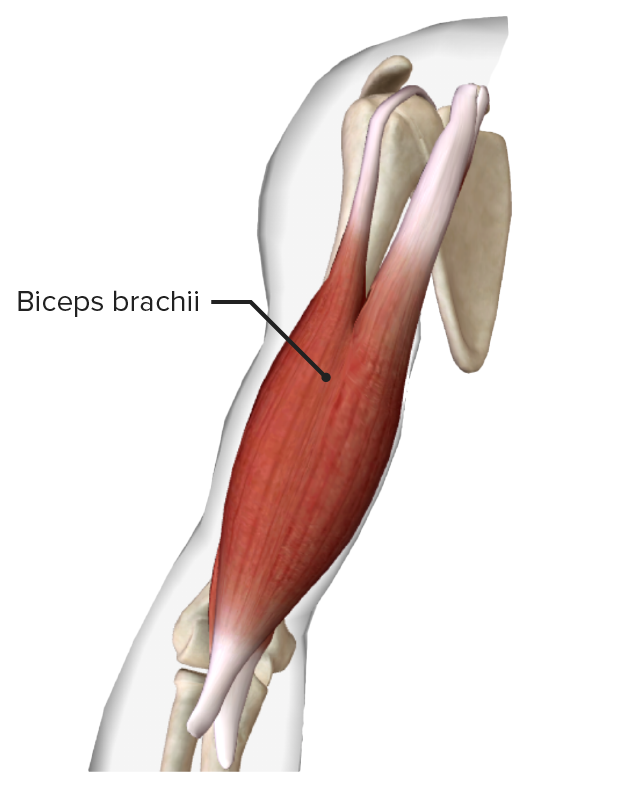
Biceps brachii muscle
Image by BioDigital, edited by Lecturio
Muscles of the anterior compartment of the arm: brachialis and coracobrachialis
Image by BioDigital, edited by Lecturio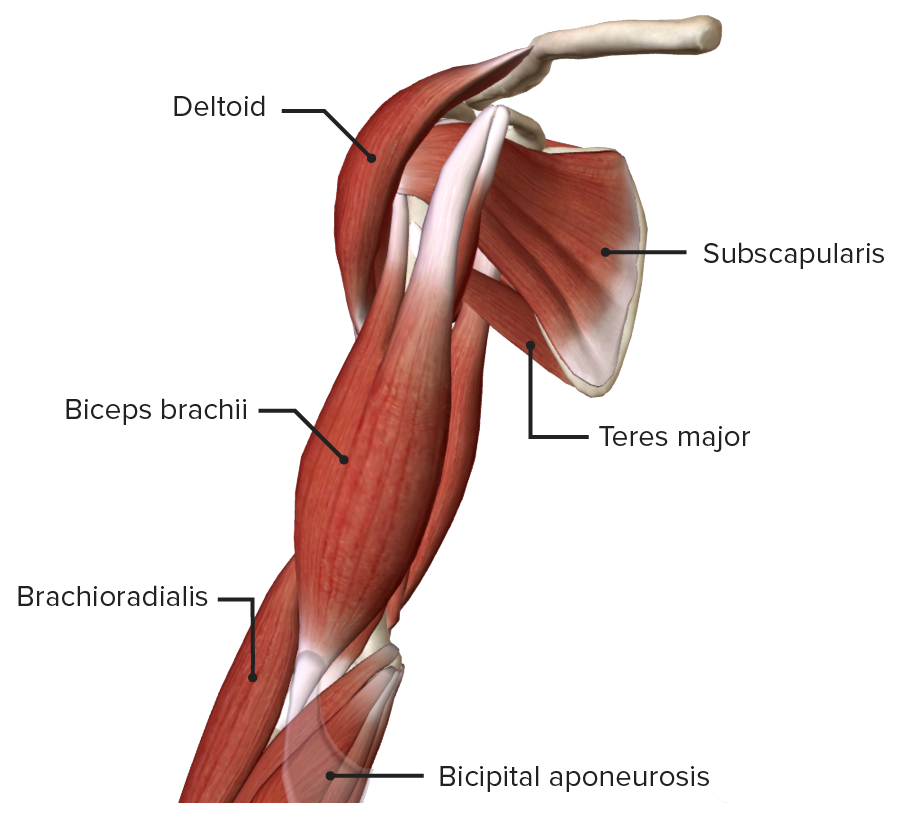
Anterior view of the right arm
Image by BioDigital, edited by Lecturio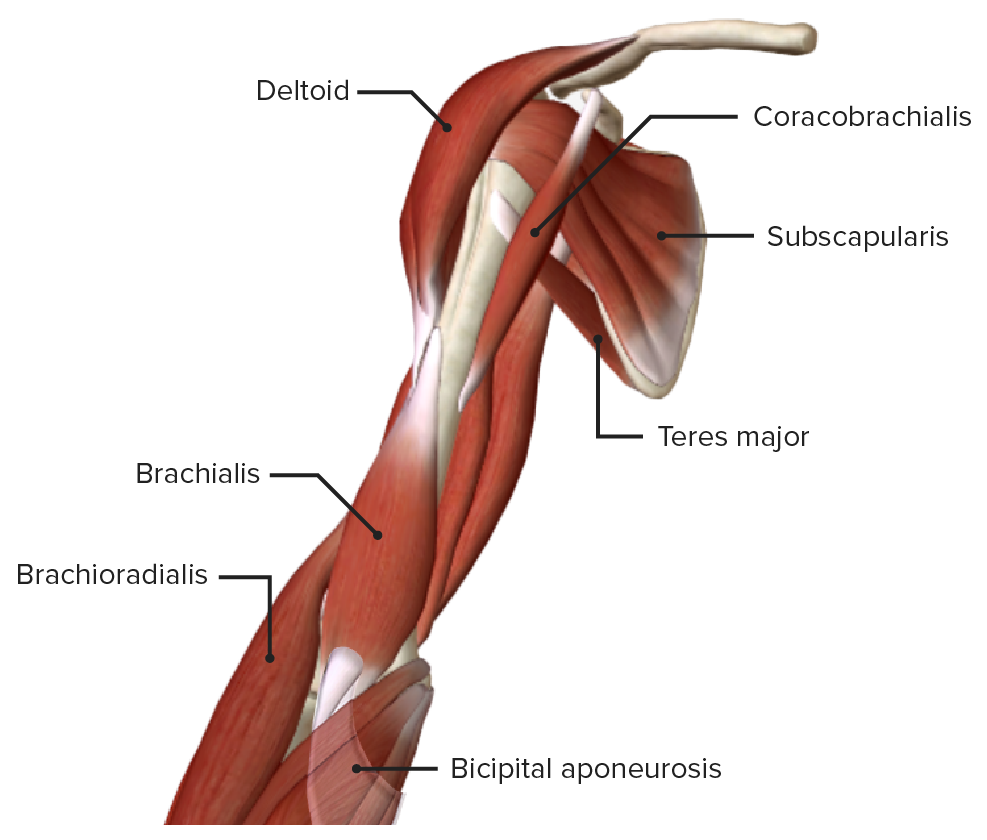
Anterior view of the right arm, featuring the muscles of the anterior compartment with the biceps brachii removed
Image by BioDigital, edited by Lecturio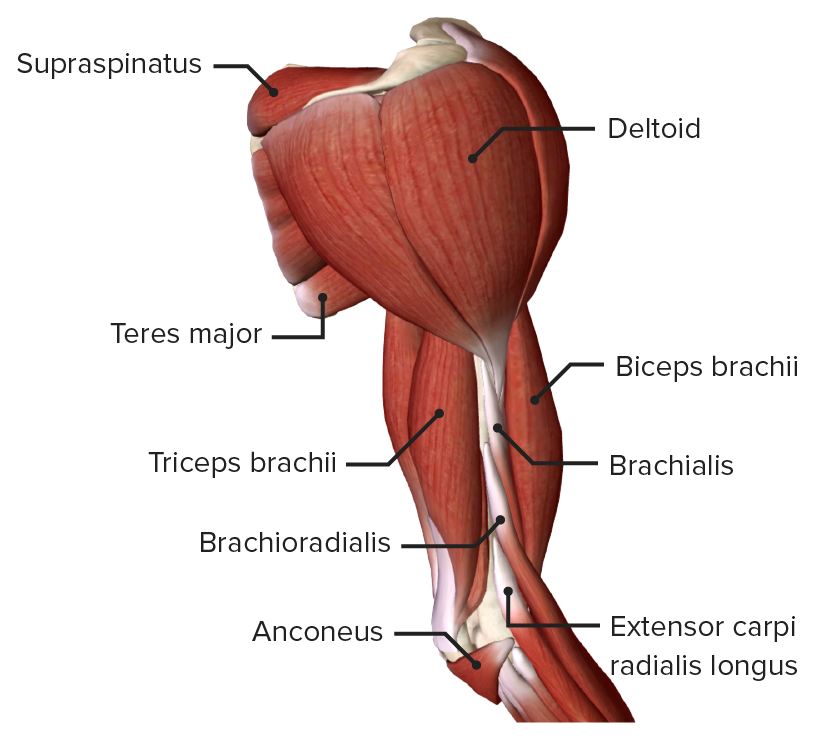
Lateral view of the right arm, featuring the deltoid, the muscles of the anterior compartment (biceps brachii, brachialis, brachioradialis), and the posterior compartment (triceps brachii)
Image by BioDigital, edited by Lecturio| Muscle | Origin | Insertion | Innervation | Function |
|---|---|---|---|---|
| Triceps brachii Triceps brachii Elbow Joint: Anatomy |
|
Olecranon | Radial nerve Radial Nerve A major nerve of the upper extremity. In humans the fibers of the radial nerve originate in the lower cervical and upper thoracic spinal cord (usually C5 to T1), travel via the posterior cord of the brachial plexus, and supply motor innervation to extensor muscles of the arm and cutaneous sensory fibers to extensor regions of the arm and hand. Axilla and Brachial Plexus: Anatomy (C7, C8) |
|
| Anconeus Anconeus Elbow Joint: Anatomy | Inserts on the posterior aspect of lateral epicondyle | Lateral surface of the olecranon | Radial nerve Radial Nerve A major nerve of the upper extremity. In humans the fibers of the radial nerve originate in the lower cervical and upper thoracic spinal cord (usually C5 to T1), travel via the posterior cord of the brachial plexus, and supply motor innervation to extensor muscles of the arm and cutaneous sensory fibers to extensor regions of the arm and hand. Axilla and Brachial Plexus: Anatomy (C7, C8) | Assists in extension Extension Examination of the Upper Limbs of the elbow and stabilizes the joint |
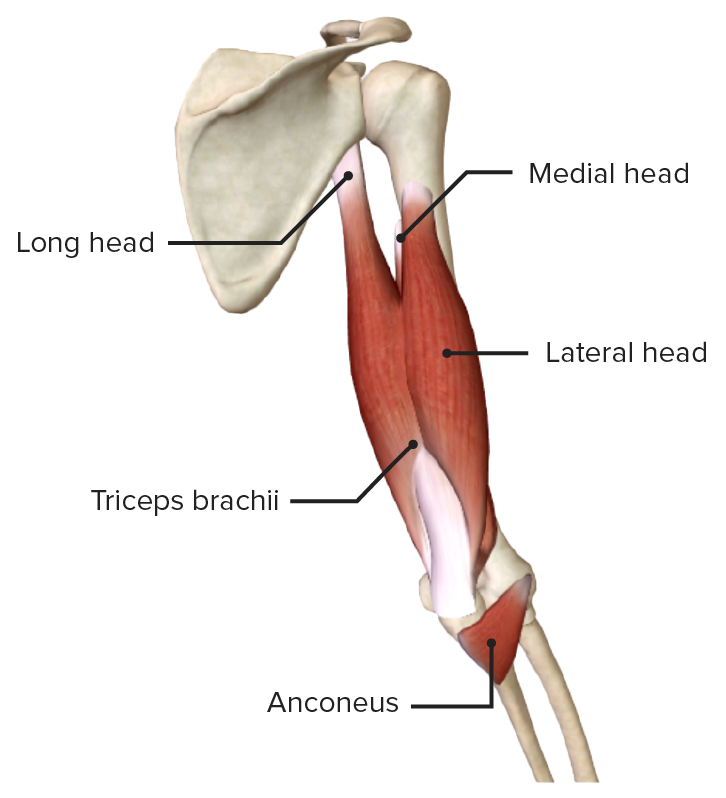
Posterior view of the arm featuring the muscles of the posterior compartment: the triceps brachii and the anconeus
Image by BioDigital, edited by Lecturio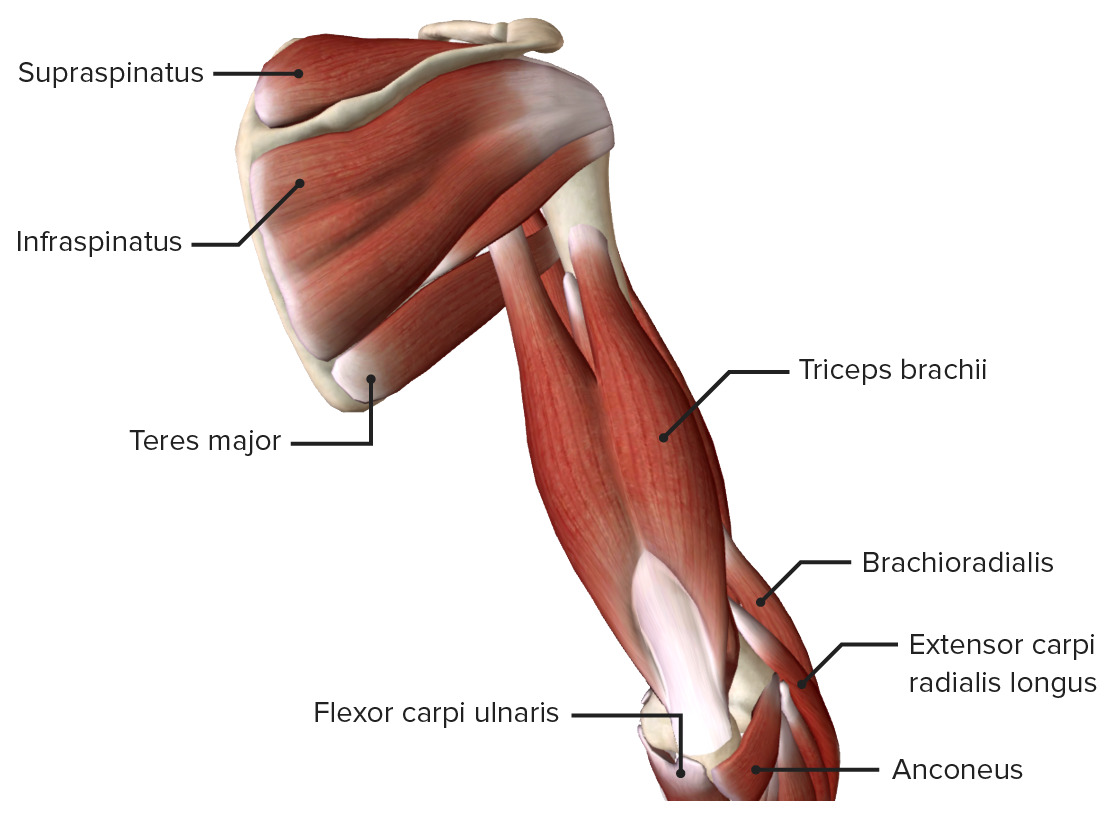
Posterior view of the arm
Image by BioDigital, edited by Lecturio| Medial bicipital groove | Lateral bicipital groove | |
|---|---|---|
| Location | Between the biceps brachii muscle Biceps brachii muscle Elbow Joint: Anatomy and the triceps brachii Triceps brachii Elbow Joint: Anatomy | Between the biceps brachii muscle Biceps brachii muscle Elbow Joint: Anatomy and the brachial muscle |
| Arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology | Brachial artery Brachial Artery The continuation of the axillary artery; it branches into the radial and ulnar arteries. Cubital Fossa: Anatomy | Radial collateral artery |
| Veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology |
|
|
| Nerves |
|
Radial nerve Radial Nerve A major nerve of the upper extremity. In humans the fibers of the radial nerve originate in the lower cervical and upper thoracic spinal cord (usually C5 to T1), travel via the posterior cord of the brachial plexus, and supply motor innervation to extensor muscles of the arm and cutaneous sensory fibers to extensor regions of the arm and hand. Axilla and Brachial Plexus: Anatomy |
The brachial artery Brachial Artery The continuation of the axillary artery; it branches into the radial and ulnar arteries. Cubital Fossa: Anatomy:
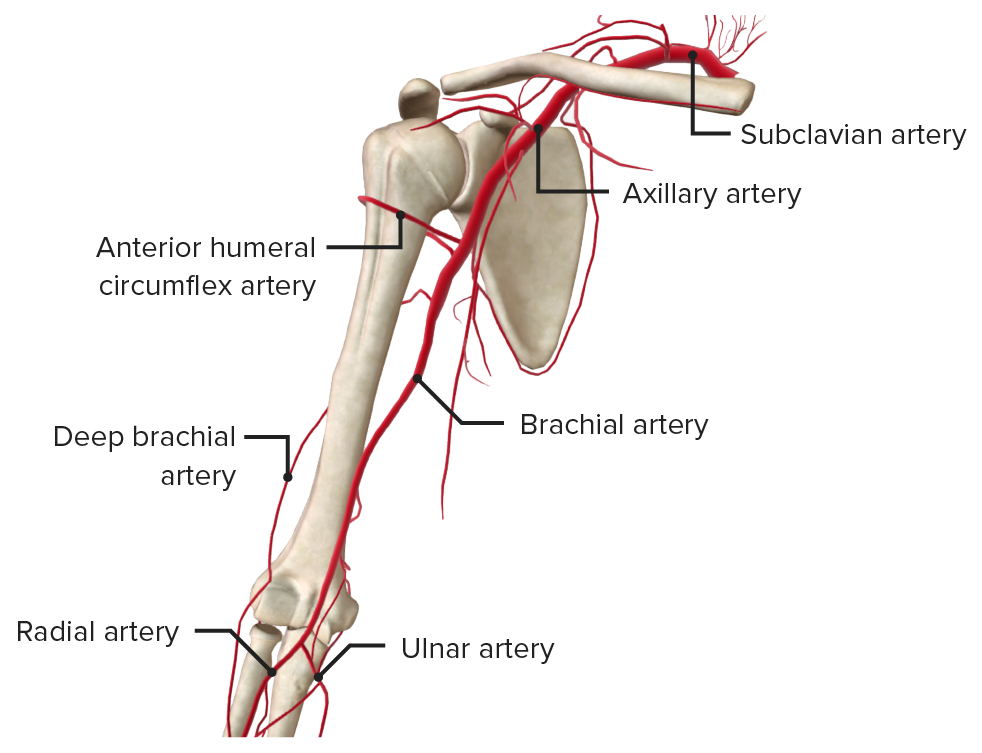
Arteries of the arm
Image by BioDigital, edited by Lecturio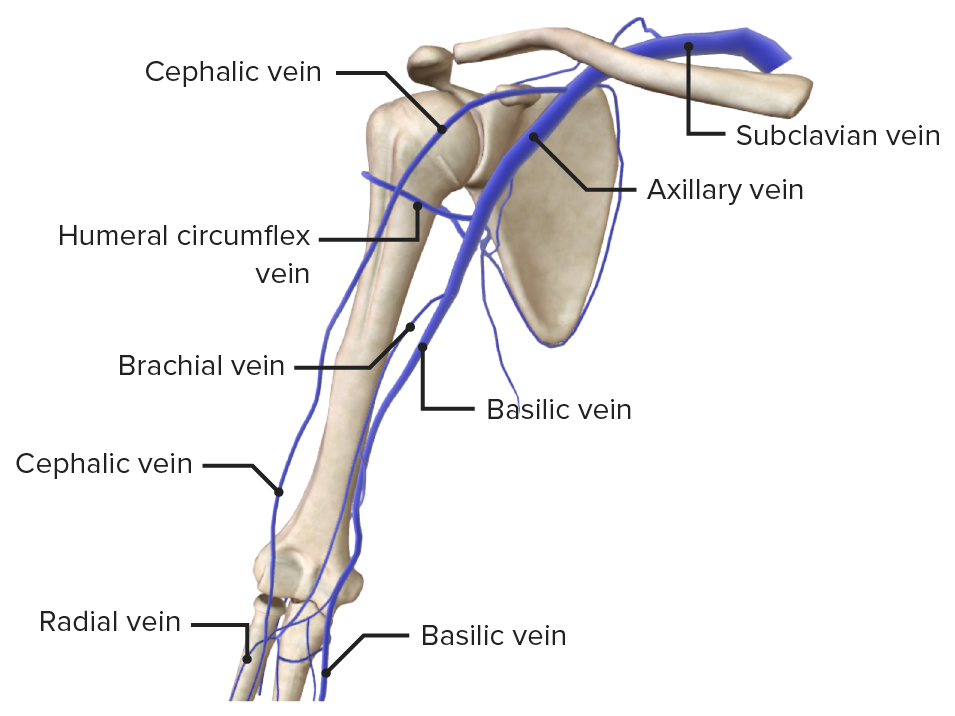
Veins of the arm
Image by BioDigital, edited by Lecturio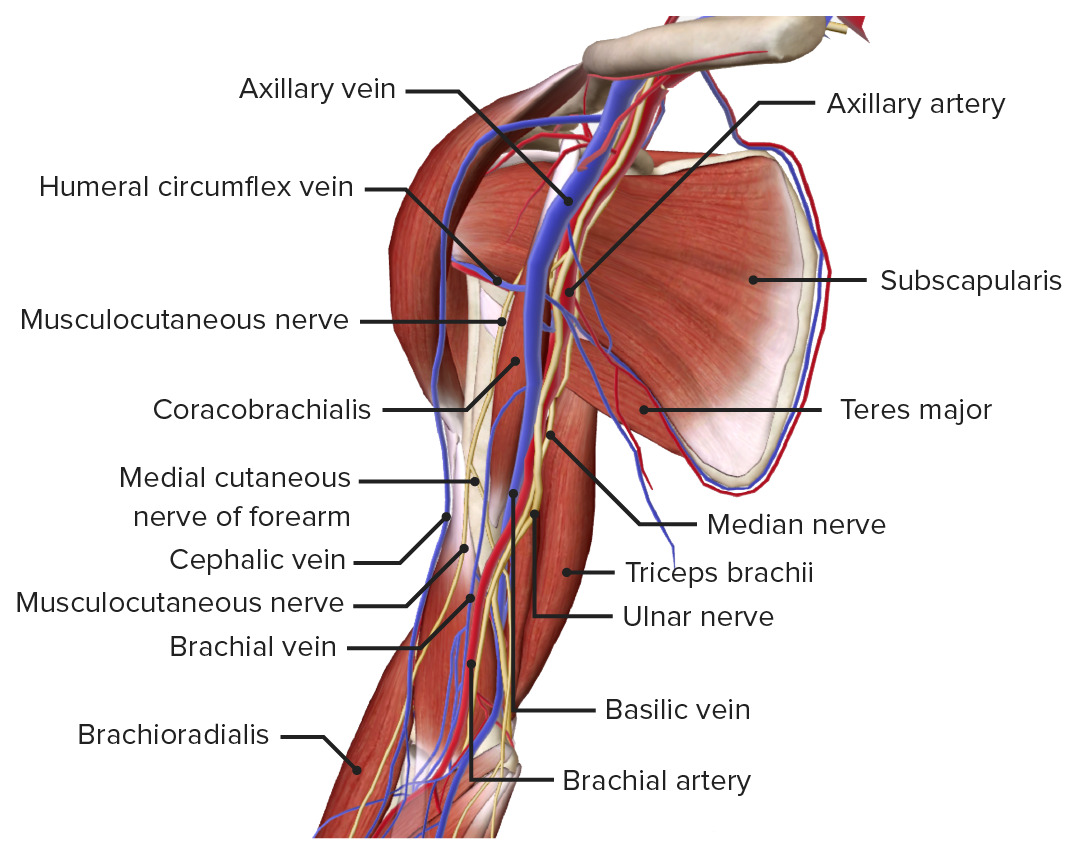
Anteromedial view of the right arm and shoulder joint, featuring the brachial artery and basilic, cephalic, and brachial veins
Image by BioDigital, edited by Lecturio| Nerve | Origin | Branches | Functions |
|---|---|---|---|
| Musculo-cutaneous | Terminal branch of lateral cord of brachial plexus Brachial Plexus The large network of nerve fibers which distributes the innervation of the upper extremity. The brachial plexus extends from the neck into the axilla. In humans, the nerves of the plexus usually originate from the lower cervical and the first thoracic spinal cord segments (c5-c8 and T1), but variations are not uncommon. Peripheral Nerve Injuries in the Cervicothoracic Region (C5–C7) |
|
|
| Median | Unison of medial and lateral roots of brachial plexus Brachial Plexus The large network of nerve fibers which distributes the innervation of the upper extremity. The brachial plexus extends from the neck into the axilla. In humans, the nerves of the plexus usually originate from the lower cervical and the first thoracic spinal cord segments (c5-c8 and T1), but variations are not uncommon. Peripheral Nerve Injuries in the Cervicothoracic Region (C5–T1) |
|
|
| Ulnar | Terminal branch of the medial cord of the brachial plexus Brachial Plexus The large network of nerve fibers which distributes the innervation of the upper extremity. The brachial plexus extends from the neck into the axilla. In humans, the nerves of the plexus usually originate from the lower cervical and the first thoracic spinal cord segments (c5-c8 and T1), but variations are not uncommon. Peripheral Nerve Injuries in the Cervicothoracic Region (C8, T1) |
|
|
| Radial | Posterior cord of the brachial plexus Brachial Plexus The large network of nerve fibers which distributes the innervation of the upper extremity. The brachial plexus extends from the neck into the axilla. In humans, the nerves of the plexus usually originate from the lower cervical and the first thoracic spinal cord segments (c5-c8 and T1), but variations are not uncommon. Peripheral Nerve Injuries in the Cervicothoracic Region (C5–T1) |
|
|
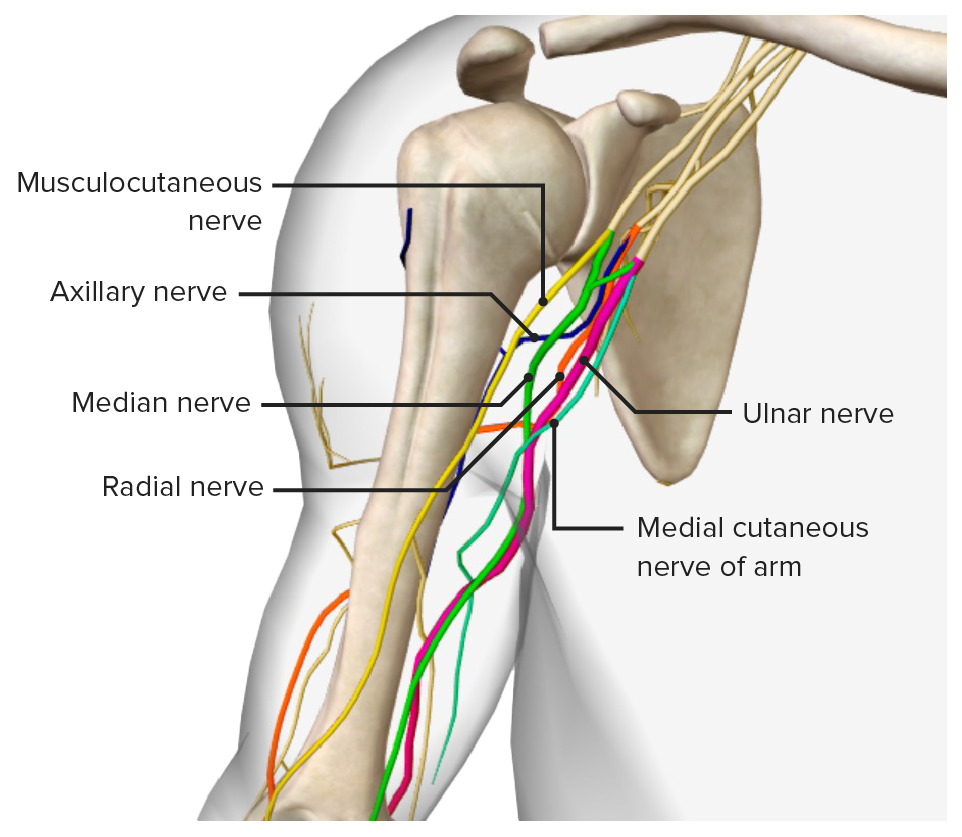
The nerves of the arm, featuring the 5 terminal branches of the brachial plexus: the musculocutaneous, axillary, median, radial, and ulnar nerves
Image by BioDigital, edited by Lecturio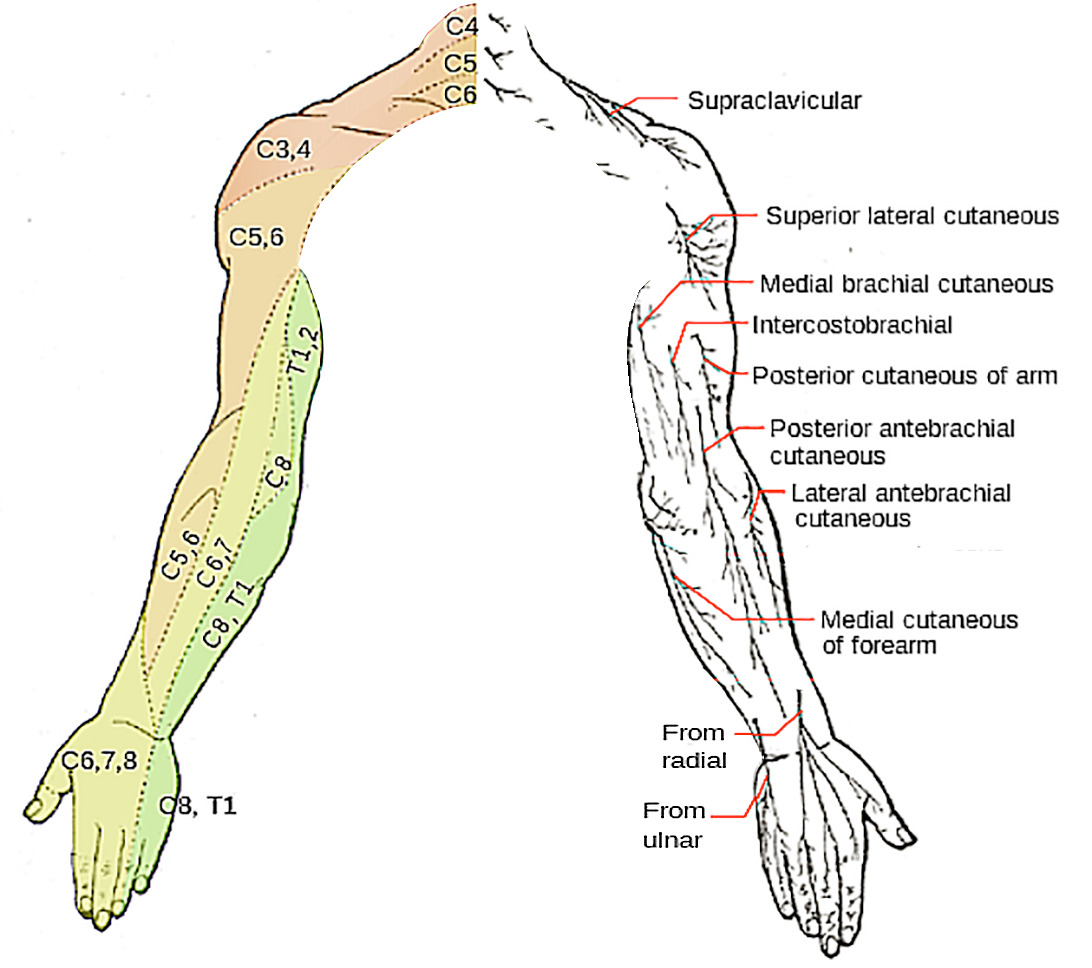
Dermatome map of the nerve roots and superficial innervation of the arm
Image: “Dermatomes and cutaneous nerves” by Mikael Häggström. License: Public Domain, edited by LecturioThe following injuries are important conditions related to the upper arm:
Drake, R.L., Vogl, A.W., & Mitchell, A.W.M. (2014). Gray’s Anatomy for Students (3rd ed.). Philadelphia, PA: Churchill Livingstone.