Legg-Calvé-Perthes disease (LCPD) is characterized by idiopathic Idiopathic Dermatomyositis avascular necrosis Avascular Necrosis Hip Fractures of the femoral head. The disease presents as a limp with an insidious onset and associated hip pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways. Legg-Calvé-Perthes disease primarily affects school-age children and has a male predominance. The exact mechanism of this disease is unknown and the diagnosis is made by clinical findings and imaging. Management can be conservative or surgical, depending on severity and the age of the patient.
Last updated: Dec 15, 2025
Legg-Calvé-Perthes disease (LCPD), also called coxa plana, is a disorder of the hip in which blood supply to the proximal femoral epiphysis Epiphysis The head of a long bone that is separated from the shaft by the epiphyseal plate until bone growth stops. At that time, the plate disappears and the head and shaft are united. Bones: Structure and Types is temporarily interrupted, resulting in avascular necrosis Avascular Necrosis Hip Fractures and permanent deformity Deformity Examination of the Upper Limbs of the femoral head and acetabulum.
Legg-Calvé-Perthes disease is a multifactorial disease caused by a combination of genetic, environmental, and vascular factors. The interruption of blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure to the capital femoral epiphysis Epiphysis The head of a long bone that is separated from the shaft by the epiphyseal plate until bone growth stops. At that time, the plate disappears and the head and shaft are united. Bones: Structure and Types is the inciting cause. The following have been implicated as potential contributors to vascular compromise:
There are 4 stages of LCPD:
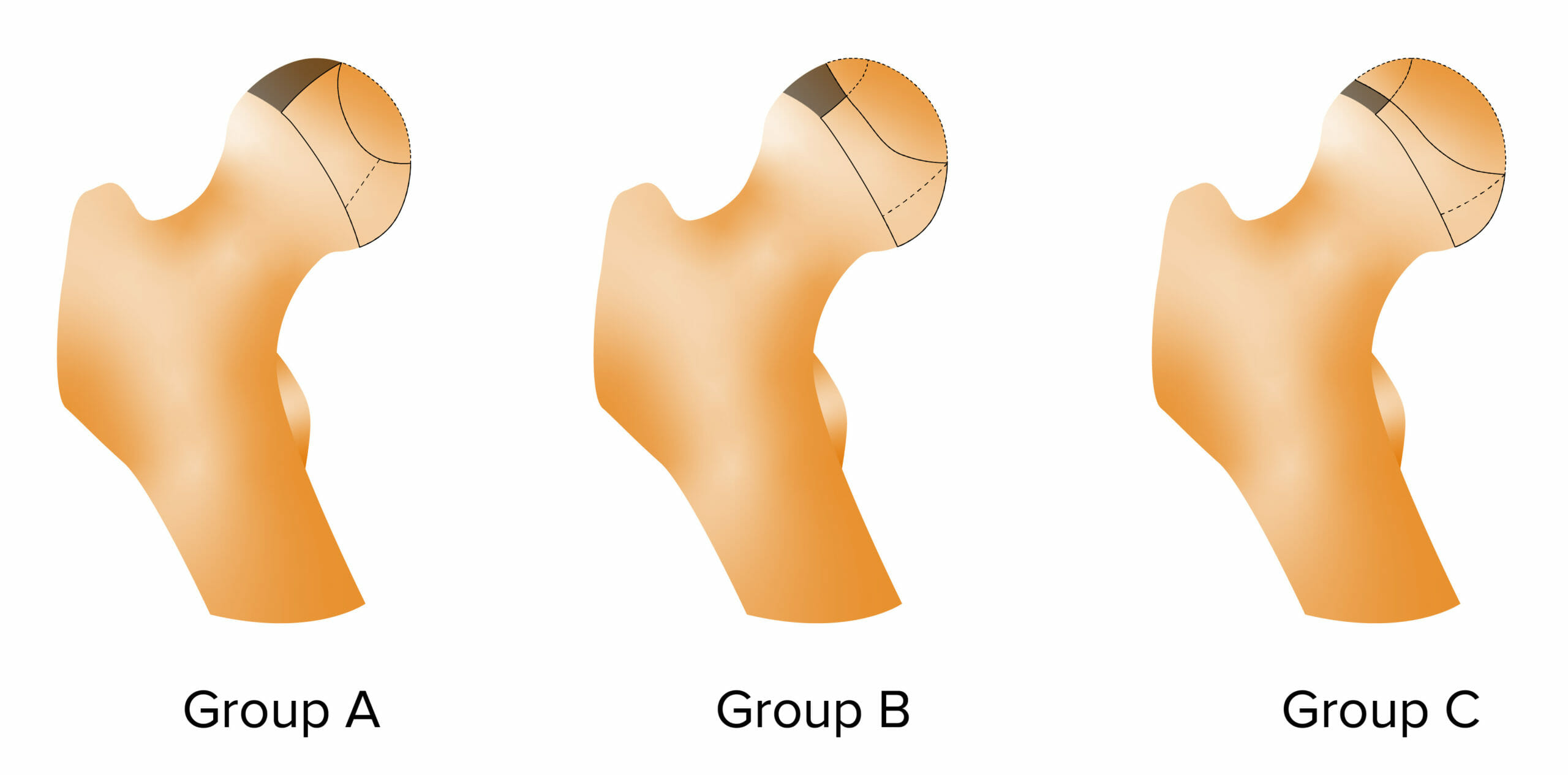
Herring lateral pillar classification for Legg-Calvé-Perthes disease (LCPD):
Group A has no evident involvement of lateral pillar (lateral ⅓ of epiphysis) and the lateral pillar height is normal.
Group B has lost < 50% of lateral pillar height.
Group C has lost > 50% of lateral pillar height
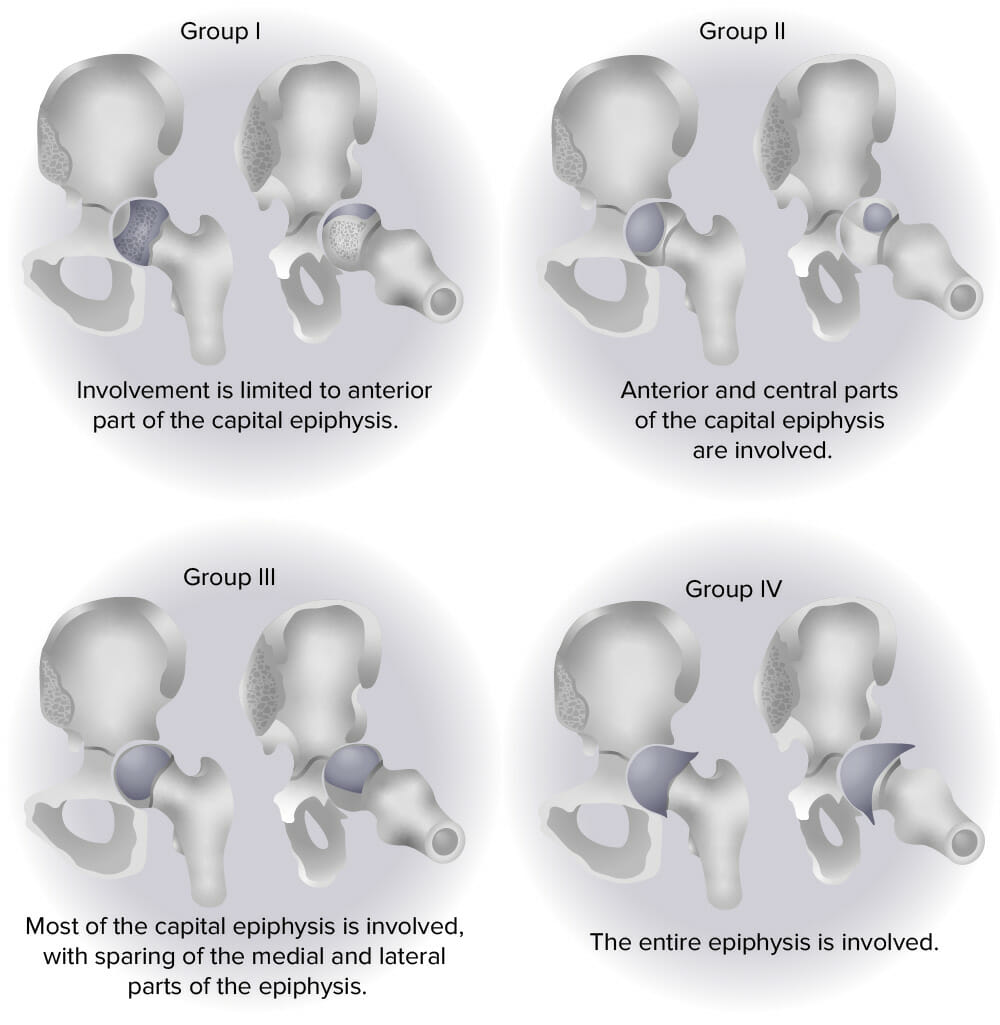
Catterall classification for Legg-Calvé-Perthes disease (LCPD)
Image by Lecturio.
Deformation of the head of the femur due to LCPD
Legg-Calvé-Perthes disease is a disorder of the hip in which blood supply to the proximal femoral epiphysis is temporarily interrupted, resulting in avascular necrosis and permanent deformity of the femoral head and acetabulum.
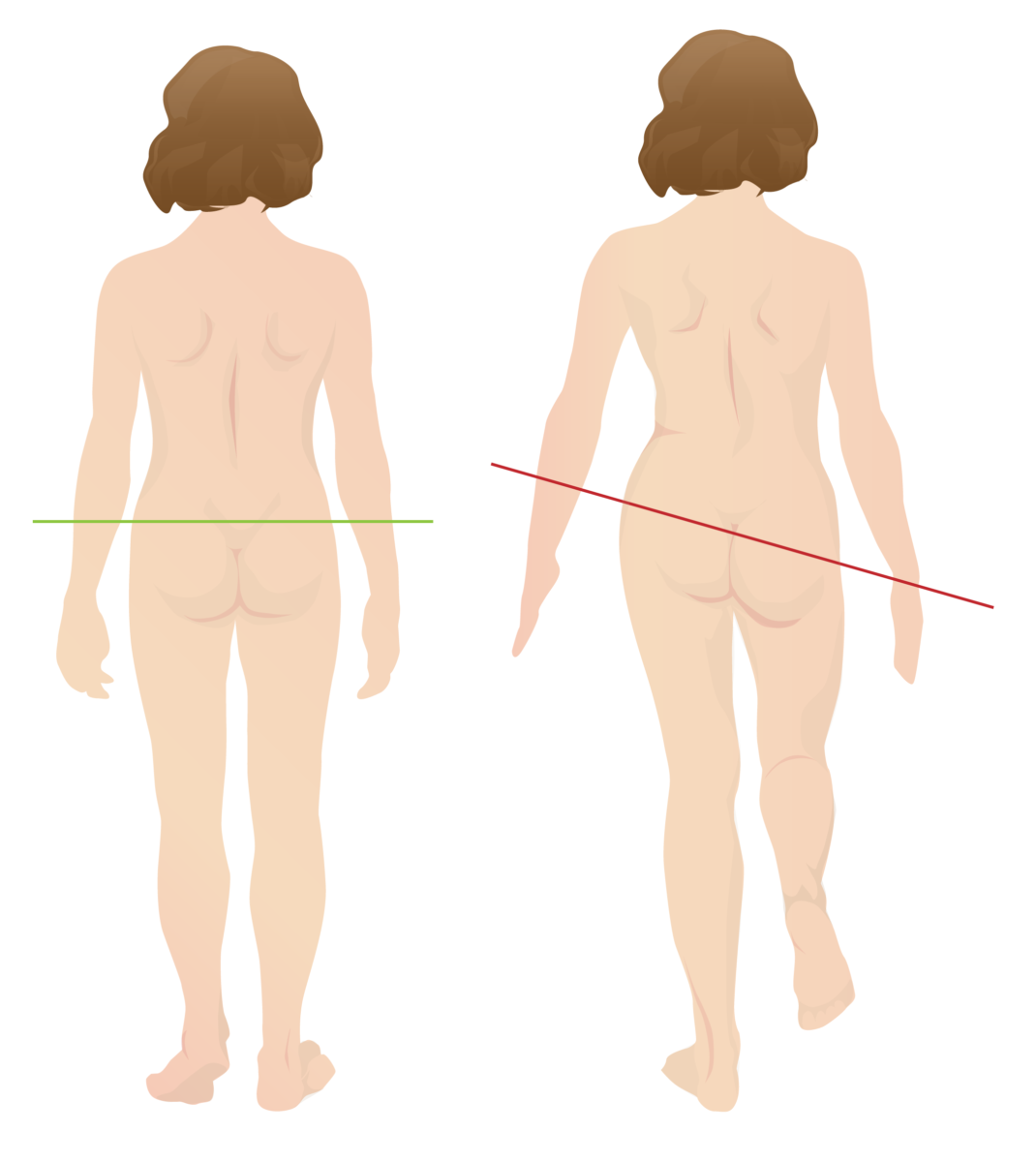
Trendelenburg gait
Seen in patients with LCPD, this gait features a downward tilt of the pelvis opposite to the affected hip during the swing phase of walking.
The diagnosis of LCPD is clinical and confirmed through targeted imaging, so a high degree of suspicion is required in the approach to the limping child.
Short stature: due to genetics Genetics Genetics is the study of genes and their functions and behaviors. Basic Terms of Genetics, developmental disorders, and leg-length discrepancy, child may be shorter in stature.
Osteoarthritis (OA): most common form of arthritis, often referred to as “wear and tear” arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis. Principally a disease of aging, characterized by hyaline articular cartilage Cartilage Cartilage is a type of connective tissue derived from embryonic mesenchyme that is responsible for structural support, resilience, and the smoothness of physical actions. Perichondrium (connective tissue membrane surrounding cartilage) compensates for the absence of vasculature in cartilage by providing nutrition and support. Cartilage: Histology loss, but also involving changes to subchondral bone Subchondral Bone Osteochondritis Dissecans, synovium, and surrounding joint structures. Anatomical abnormalities produced by LCPD increase the risk for degenerative changes Degenerative Changes Spinal Stenosis of the hip joint Hip joint The hip joint is a ball-and-socket joint formed by the head of the femur and the acetabulum of the pelvis. The hip joint is the most stable joint in the body and is supported by a very strong capsule and several ligaments, allowing the joint to sustain forces that can be multiple times the total body weight. Hip Joint: Anatomy and the need for surgical replacement of the hip.