Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy exists due to a stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) of the coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology, typically from atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis. The myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy becomes ischemic when oxygen supply does not meet oxygen demand. Diagnosis is based on history and ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) findings; cardiac stress tests and catheterizations may also be needed. Treatment is primarily based on reducing the heart's oxygen demand and increasing the delivery of oxygen.
Last updated: Jan 16, 2026
Coronary heart disease (CHD) is the manifestation of atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis in the coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology such that there is an imbalance between oxygen supply and myocardial demands resulting in ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage to a portion of the myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy.
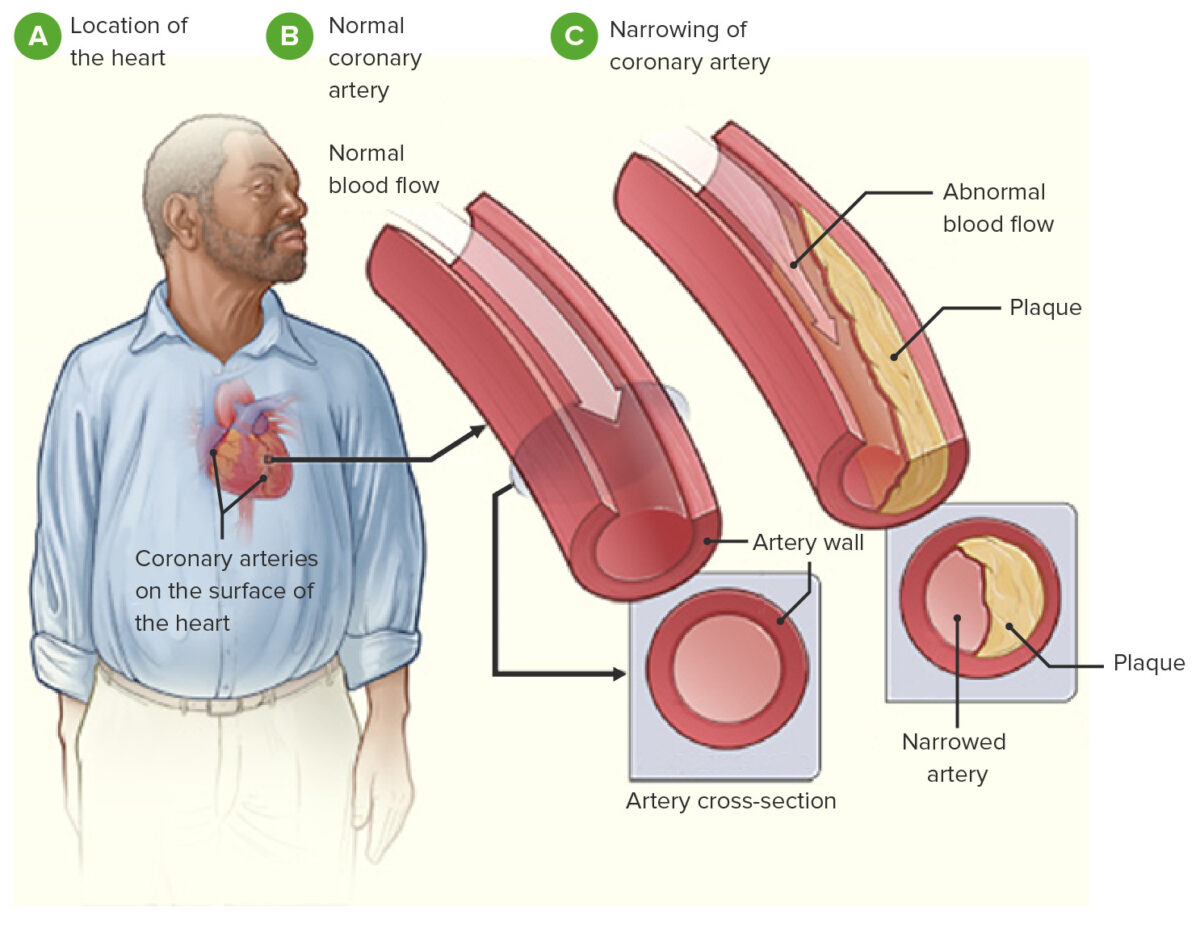
Image demonstrating pathophysiology of coronary heart disease
Image: “Coronary heart disease-atherosclerosis” by National Heart, Lung and Blood Institute. License: Public Domain, edited by Lecturio.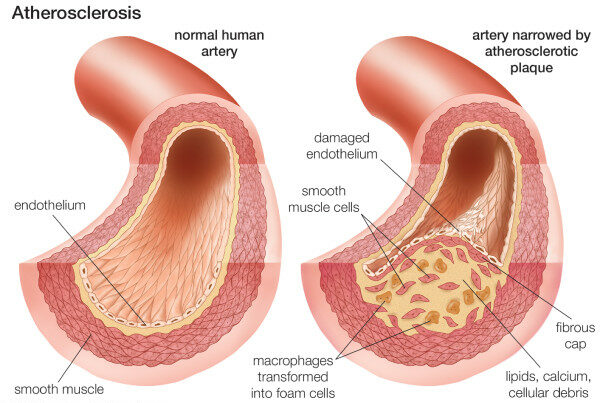
Composition of the atherosclerotic plaque
Image: “Neovascularization of coronary tunica intima (DIT) is the cause of coronary atherosclerosis. Lipoproteins invade coronary intima via neovascularization from adventitial vasa vasorum, but not from the arterial lumen: a hypothesis” by Subbotin, VM/ Encyclopeadia Britannica. License: CC BY 2.0Coronary heart disease has a spectrum of clinical presentations.
General characteristics:
Stable angina Stable angina Persistent and reproducible chest discomfort usually precipitated by a physical exertion that dissipates upon cessation of such an activity. The symptoms are manifestations of myocardial ischemia. Stable and Unstable Angina:
Unstable angina Unstable angina Precordial pain at rest, which may precede a myocardial infarction. Stable and Unstable Angina:
General characteristics:
ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) changes (irreversible):

Myocardial infarction
Image: “Heart attack-NIH” by National Heart, Lung and Blood Institute. License: Public Domain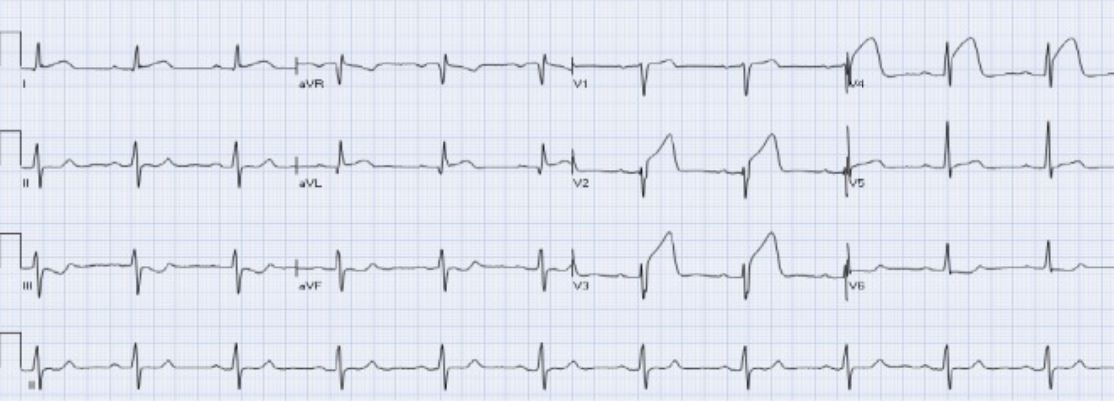
Acute anterior STEMI:
There is ST elevation in leads aVL and V2-V4 with reciprocal ST depression in leads III and aVF.