The prostate Prostate The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid. is a gland in the male reproductive system. The gland surrounds the bladder Bladder A musculomembranous sac along the urinary tract. Urine flows from the kidneys into the bladder via the ureters, and is held there until urination. Pyelonephritis and Perinephric Abscess neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess and a portion of the urethra Urethra A tube that transports urine from the urinary bladder to the outside of the body in both the sexes. It also has a reproductive function in the male by providing a passage for sperm. Urinary Tract: Anatomy. The prostate Prostate The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid. is an exocrine gland that produces a weakly acidic secretion Secretion Coagulation Studies, which accounts for roughly 20% of the seminal fluid. The prostate Prostate The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid. consists of multiple lobes and is made up of glandular and fibromuscular tissue. The glandular tissue has ducts that empty into the prostatic portion of the urethra Urethra A tube that transports urine from the urinary bladder to the outside of the body in both the sexes. It also has a reproductive function in the male by providing a passage for sperm. Urinary Tract: Anatomy, and the fibromuscular tissue encircles the urethra Urethra A tube that transports urine from the urinary bladder to the outside of the body in both the sexes. It also has a reproductive function in the male by providing a passage for sperm. Urinary Tract: Anatomy.
Last updated: Nov 18, 2024
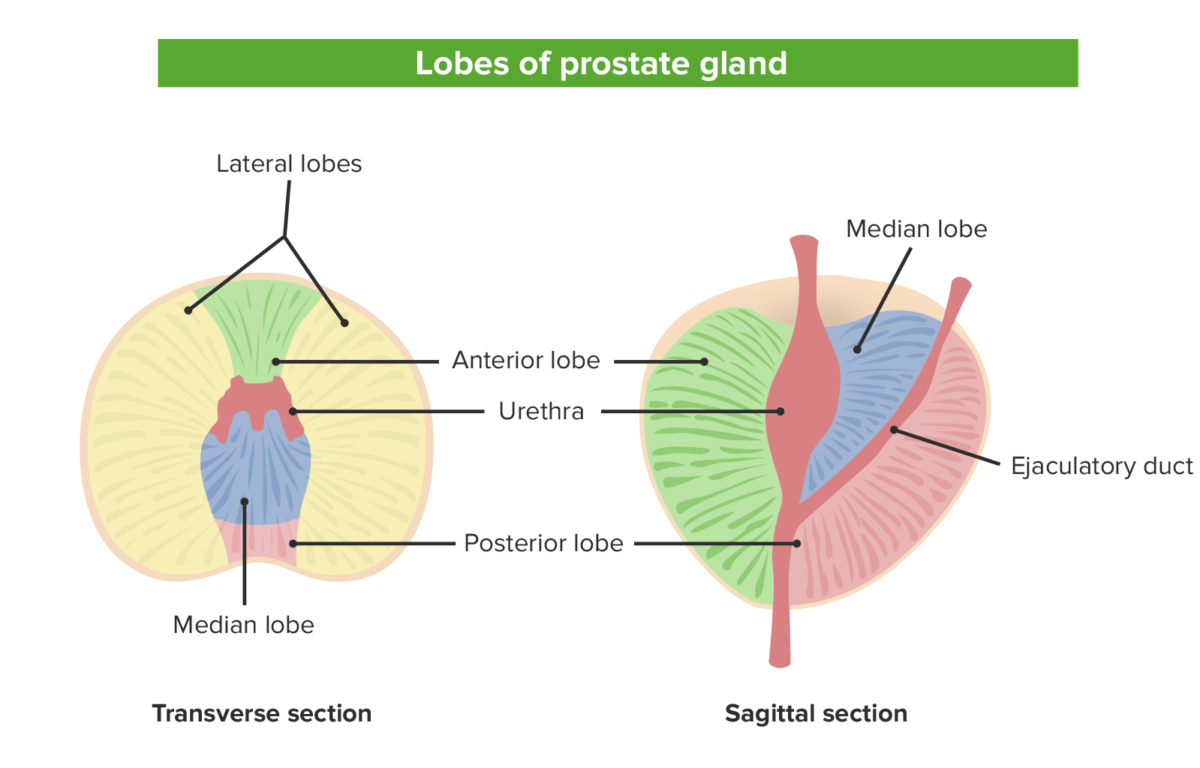
The 5 lobes of the prostate from both the sagittal view on the left and the transverse view on the right: Note the relationship between the various lobes and the locations of the urethra and ejaculatory duct.
Image by Lecturio.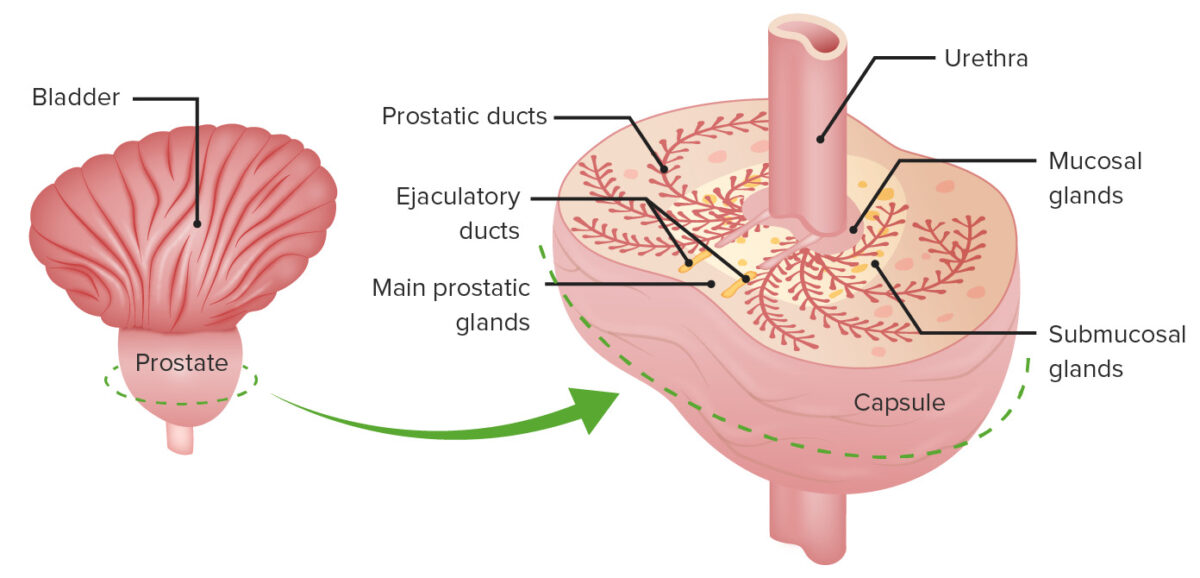
The different zones: the mucosal gland that surrounds the prostatic urethra, the central submucosal glands, and the peripheral main prostatic glands
Image by Lecturio.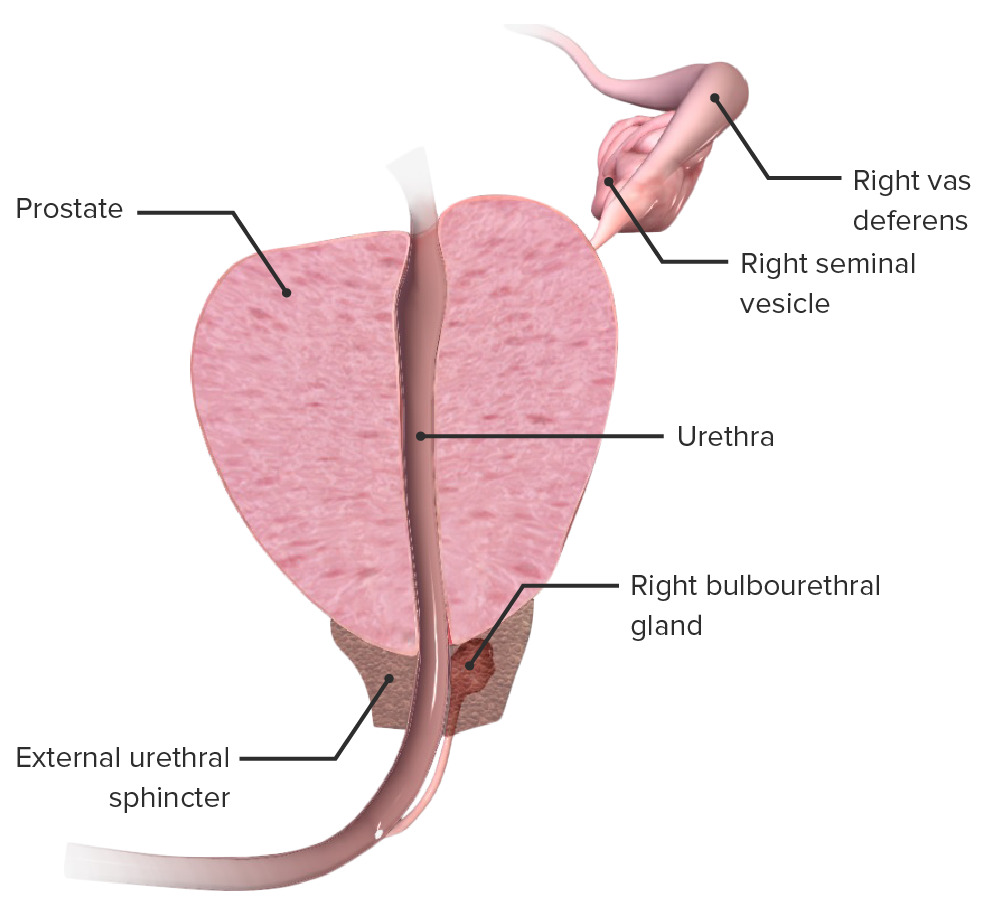
Anatomy of the prostate:
Cross-section of the prostate demonstrating its relation to the prostatic urethra, urethral sphincter, seminal vesicles, and bulbourethral gland
Blood vessels supplying the prostate Prostate The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid. arise from the internal iliac artery and enter the gland from the posterolateral region.
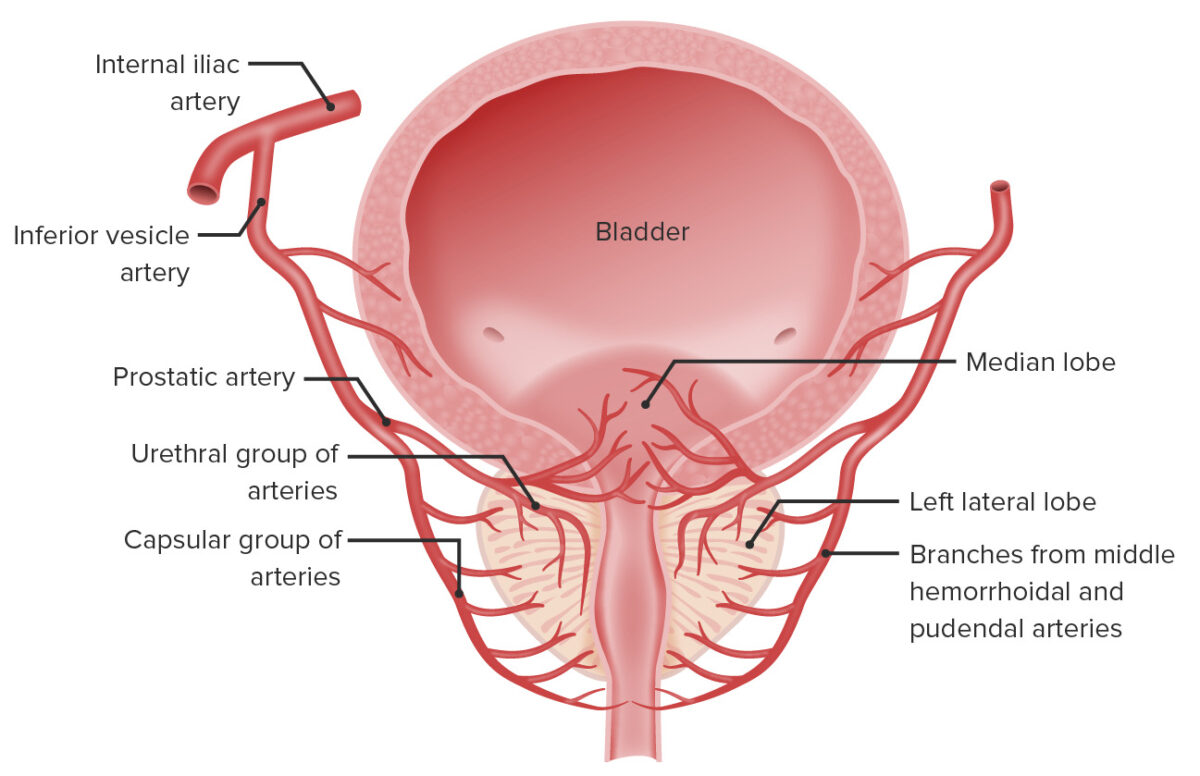
Anatomy of the vascular supply of the prostate and bladder:
The arterial blood supply of the prostate and bladder originates from the internal iliac artery, which gives off the inferior vesicle artery. This in turn gives rise to the prostatic artery, which branches in urethral and capsular groups which feed those portions of the prostate.
The prostate Prostate The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid. consists of glandular tissue and fibromuscular tissue.
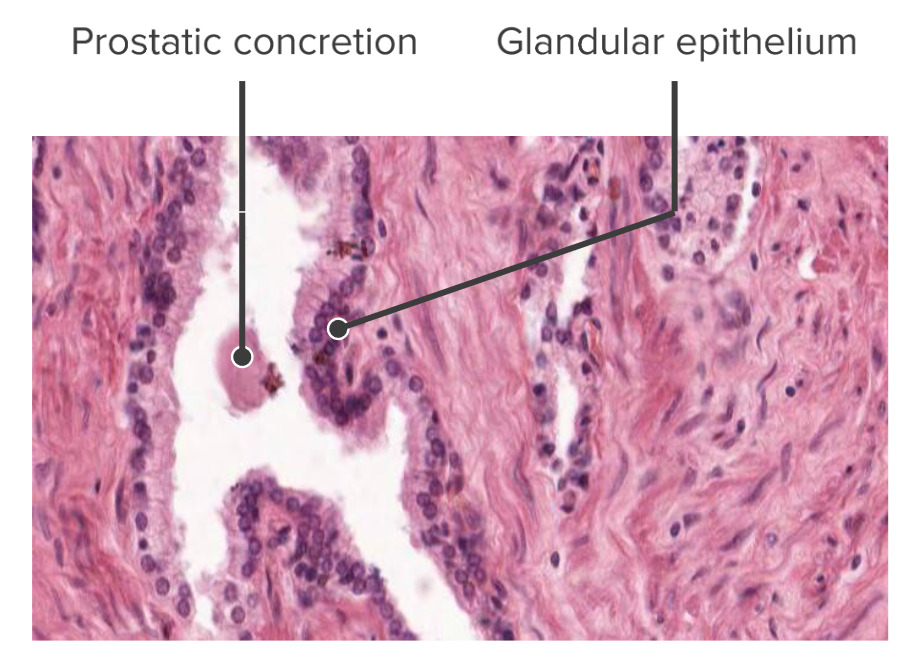
The glandular columnar epithelium of the prostate gland (histological):
Note, on this slide, the prostatic concretion; these concretions can have a clinical application if they build up and impinge on the urethra → difficulty urinating