Autoimmune hepatitis (AIH) is an increasingly recognized chronic inflammatory liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease with rising global incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency. Clinical presentation ranges from asymptomatic cases to symptoms of acute liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy failure ( jaundice Jaundice Jaundice is the abnormal yellowing of the skin and/or sclera caused by the accumulation of bilirubin. Hyperbilirubinemia is caused by either an increase in bilirubin production or a decrease in the hepatic uptake, conjugation, or excretion of bilirubin. Jaundice, right upper quadrant Right upper quadrant Anterior Abdominal Wall: Anatomy pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways). Diagnosis relies on characteristic serological findings, elevated IgG IgG The major immunoglobulin isotype class in normal human serum. There are several isotype subclasses of igg, for example, igg1, igg2a, and igg2b. Hypersensitivity Pneumonitis, and histological evidence of interface hepatitis, with recent consensus moving away from traditional markers like emperipolesis and rosettes. Early recognition is crucial given the significant mortality Mortality All deaths reported in a given population. Measures of Health Status risk without treatment. Standard therapy with corticosteroids Corticosteroids Chorioretinitis and azathioprine Azathioprine An immunosuppressive agent used in combination with cyclophosphamide and hydroxychloroquine in the treatment of rheumatoid arthritis. According to the fourth annual report on carcinogens, this substance has been listed as a known carcinogen. Immunosuppressants achieves a complete biochemical response in most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship. Overlap syndromes present additional diagnostic and therapeutic challenges requiring specialized care.
Last updated: Jun 3, 2025
Epidemiology
Etiology
Associated with other autoimmune conditions (e.g., Hashimoto thyroiditis Thyroiditis Thyroiditis is a catchall term used to describe a variety of conditions that have inflammation of the thyroid gland in common. It includes pathologies that cause an acute illness with severe thyroid pain (e.g., subacute thyroiditis and infectious thyroiditis) as well as conditions in which there is no clinically evident inflammation and the manifestations primarily reflect thyroid dysfunction or a goiter (e.g., painless thyroiditis and fibrous Riedel’s thyroiditis). Thyroiditis, Graves disease, diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus, rheumatoid arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis, celiac disease Celiac disease Celiac disease (also known as celiac sprue or gluten enteropathy) is an autoimmune reaction to gliadin, which is a component of gluten. Celiac disease is closely associated with HLA-DQ2 and HLA-DQ8. The immune response is localized to the proximal small intestine and causes the characteristic histologic findings of villous atrophy, crypt hyperplasia, and intraepithelial lymphocytosis. Celiac Disease, Sjogren syndrome)
Autoimmune hepatitis (AIH) is a differential diagnosis for any patient presenting with at least one of the following:
Autoimmune hepatitis is a diagnosis of exclusion, so the first step is to rule out viral infection, drugs, metabolic, or genetic causes.
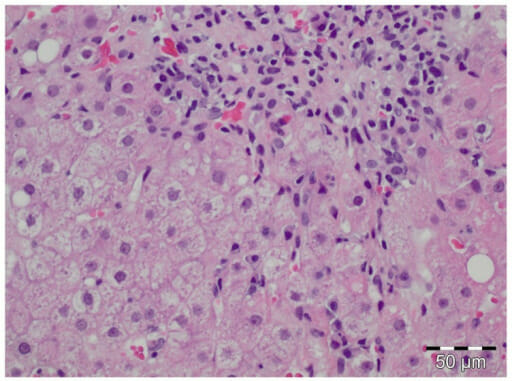
Histology of autoimmune hepatitis in an individual with acute HEV infection HEV: hepatitis E virus
Image: “pone-0085330-g002” by Sven Pischke et al. License: CC BY 4.0The following conditions are differential diagnoses of autoimmune hepatitis:
Autoimmune hepatitis can overlap with other autoimmune liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy diseases, creating diagnostic and therapeutic challenges: