Omphalocele is a congenital anterior abdominal wall Abdominal wall The outer margins of the abdomen, extending from the osteocartilaginous thoracic cage to the pelvis. Though its major part is muscular, the abdominal wall consists of at least seven layers: the skin, subcutaneous fat, deep fascia; abdominal muscles, transversalis fascia, extraperitoneal fat, and the parietal peritoneum. Surgical Anatomy of the Abdomen defect in which the intestines are covered by peritoneum Peritoneum The peritoneum is a serous membrane lining the abdominopelvic cavity. This lining is formed by connective tissue and originates from the mesoderm. The membrane lines both the abdominal walls (as parietal peritoneum) and all of the visceral organs (as visceral peritoneum). Peritoneum: Anatomy and amniotic membranes. The condition results from the failure of the midgut Midgut Development of the Abdominal Organs to return to the abdominal cavity by 10 weeks' gestation. Omphalocele is frequently associated with genetic syndromes and chromosomal abnormalities. Prenatal diagnosis can be made by prenatal ultrasound, maternal blood elevated ⍺-fetoprotein, and fetal chromosomal analysis. Treatment includes immediate hemodynamic stabilization followed by primary or staged surgical repair.
Last updated: Jan 7, 2025

Large omphalocele containing omphalomesenteric duct cyst
Image: “Large omphalocele containing OMD cyst” by Yousuf Aziz Khan, MBBS, FCPS (Paediatric Surgeon), Department of Paediatric Surgery, National Institute of Child Health, Rafiquee Shaheed Road, Karachi – 75510, Sind, Pakistan. License: CC BY 3.0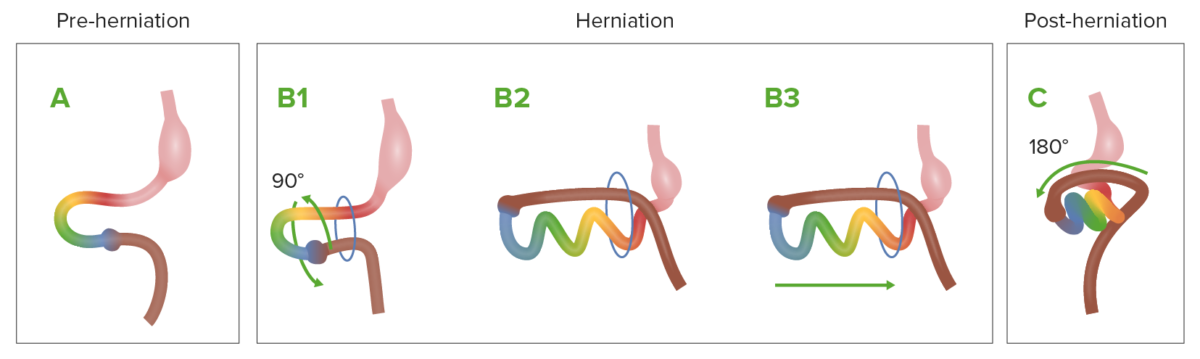
Diagram showing the normal process of intestinal rotation and herniation during embryologic development
A: The midgut (multi-colored loop) before herniation
B1–B3: As it grows rapidly, the midgut herniates through the umbilical ring and begins rotation.
C: The midgut returns to the abdominal cavity.
Pathophysiology is not definitively understood; 2 main theories:

Obstetric ultrasound at 37 weeks showing an omphalocele containing intestines and part of the liver
Image: “Obstetric ultrasound at 37 weeks containing intestines and part of the liver” by Gynaecology and Obstetrics Department I, University Hospital Hassan II, Fez, Morocco. License: CC BY 2.0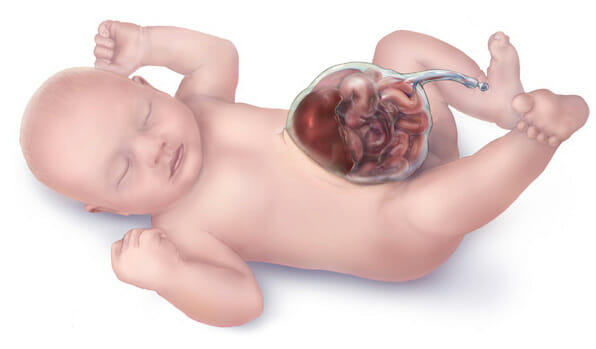
Illustration of an omphalocele
Most cases of omphalocele (90%) are diagnosed prenatally:

Staged closure of a giant omphalocele using synthetic mesh: Daily sequential reduction of synthetic mesh silo content
Image: “Daily sequential reduction of synthetic mesh silo content” by Department of Pediatric Surgery, GMC Hospital, Ajman, United Arab Emirates. License: CC BY 3.0
Staged closure of a giant omphalocele using synthetic mesh: complete closure of a giant omphalocele
Image: “Complete closure of giant omphalocele” by Department of Pediatric Surgery, GMC Hospital, Ajman, United Arab Emirates. License: CC BY 3.0