Start your online nephrology course
taught by Amy Sussman, MD from Tucson University
As challenging as it is, a solid grasp of nephrology helps attain a fuller picture of the most important systemic ailments (for example, medication-resistant hypertension may be due to a secondary cause affecting the kidneys).
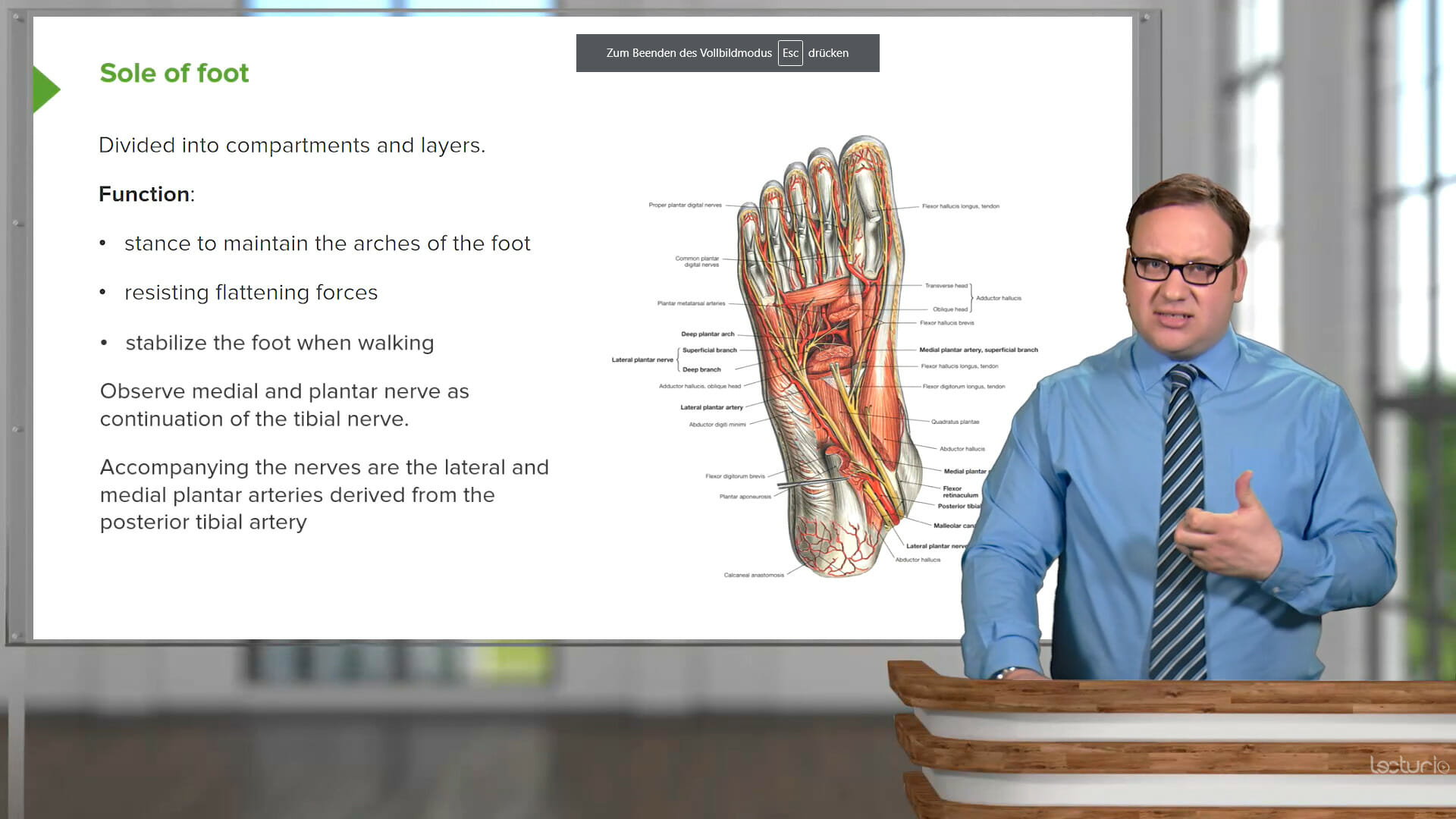
This course uses case-based presentations to review the full spectrum of kidney conditions: acute and chronic kidney injuries, nephrolithiasis, acid-base and electrolyte imbalances, conditions that affect the glomerulus, and urinary tract infections. Dr. Amy Sussman, MD, will not only teach you the key points about the pathophysiologies and treatments of the disorders, but will lead you step-by-step through the diagnostic approaches and how to decide which conditions need to be examined by an internist or nephrologist.
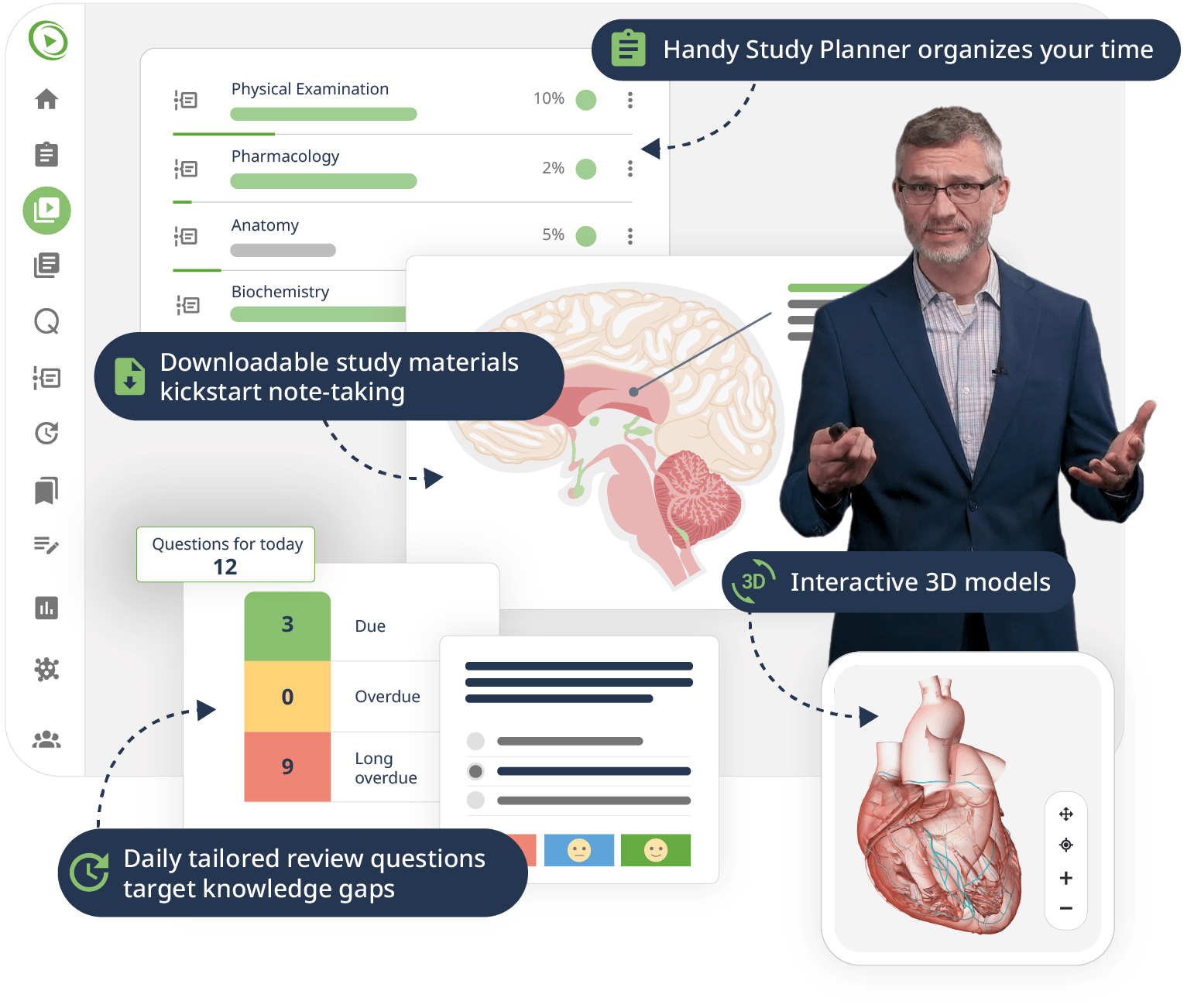
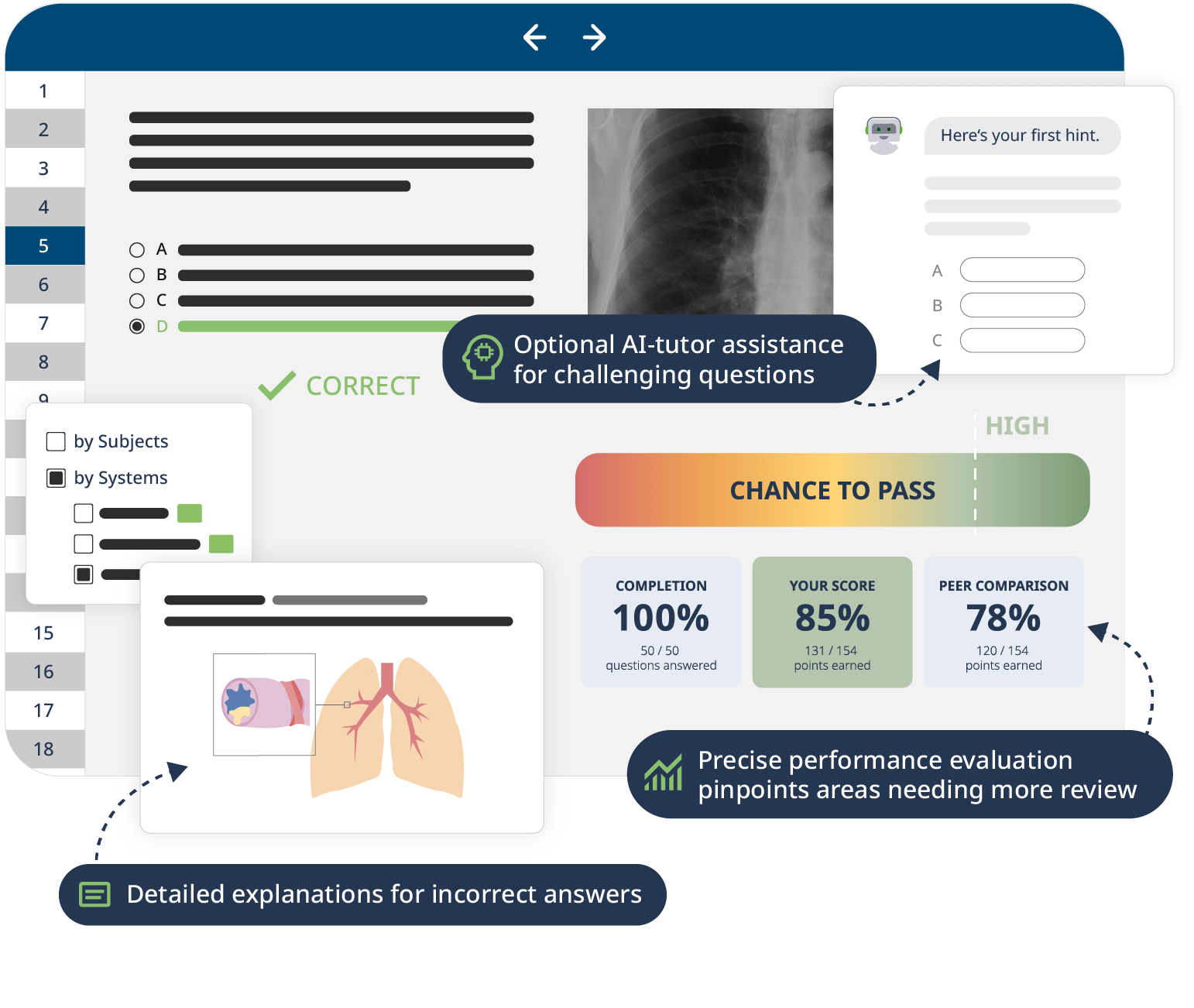
The combination of Video Lessons with interactive quiz questions, downloadable study materials, and a USMLE-style Qbank makes it easy to understand and retain the topics. By the end of this course, you will have a strong foundation in nephrology and be able to strategically think through complex cases to reach a diagnosis – on the boards as well as in clinical practice.