Take your online histology class
taught by Geoffrey Meyer, PhD
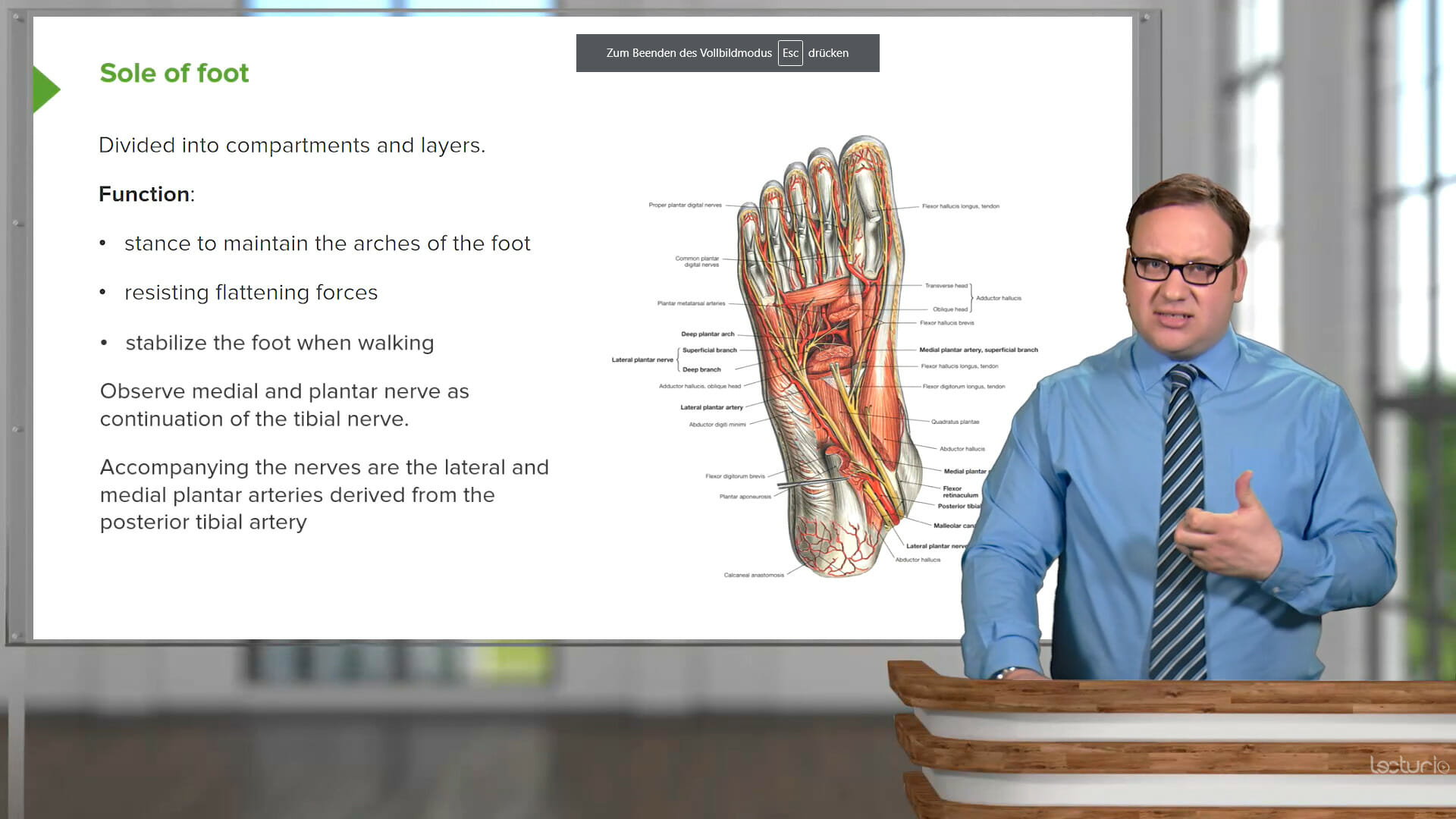
Understanding histology lays the groundwork for recognizing how tissue types contribute to the structure and function of organ systems. Connecting the large amount of information with the ability to visually recognize and distinguish tissues and cells comes with a significant learning curve.
This course covers the characteristics and functions of the body’s tissue types and how they make up the organ systems. Geoffrey Meyer, PhD, is the Coordinator for Histology in the Federative International Program for Anatomical Terminologies (FIPAT) and will break down the information in a systematic way, moving from the basic tissue types to the concept of cell specialization and the histology of each organ system, including cardiovascular, reproductive, gastrointestinal, and sensory histology. The course will also explain the techniques used to prepare tissues for study.
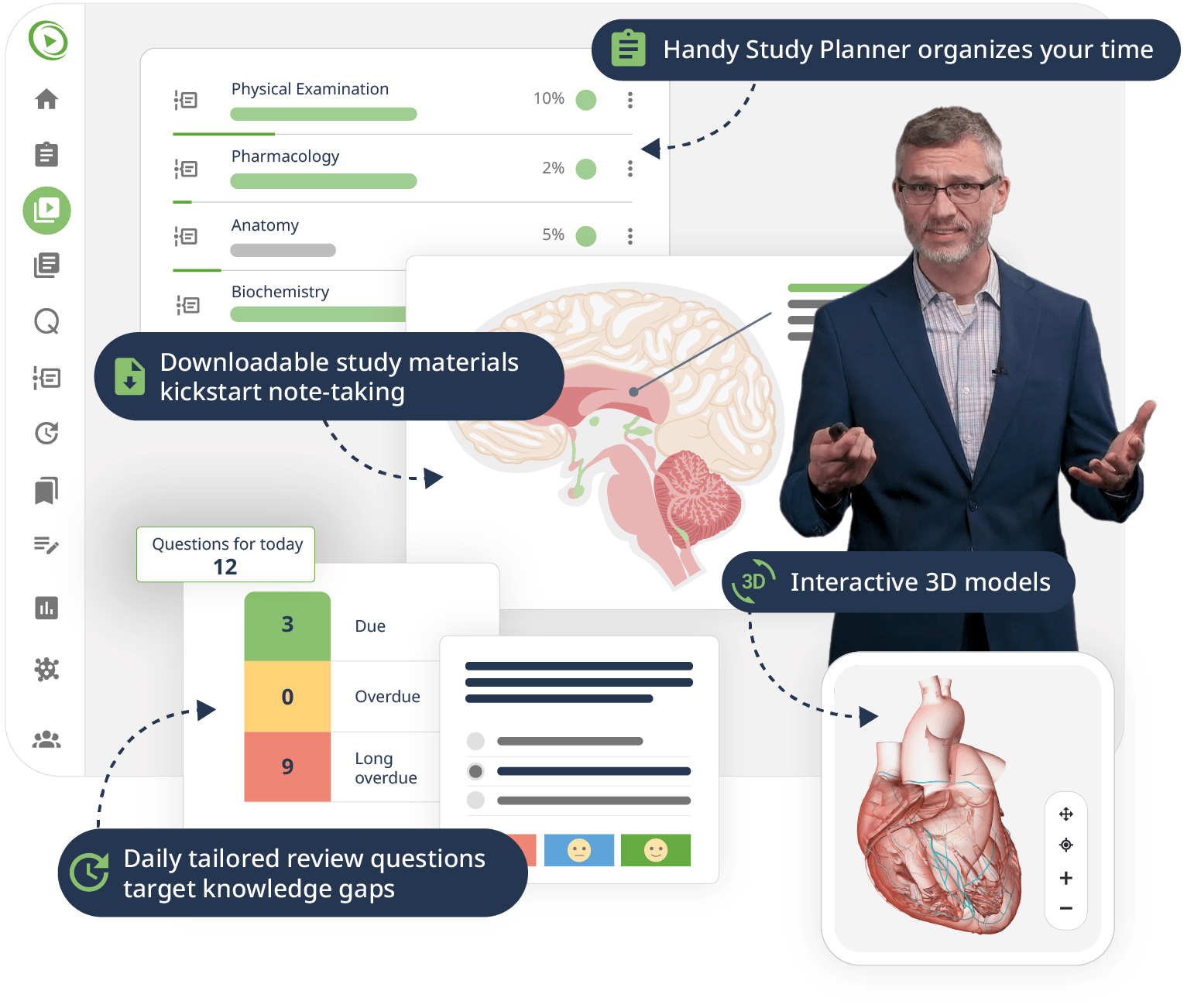
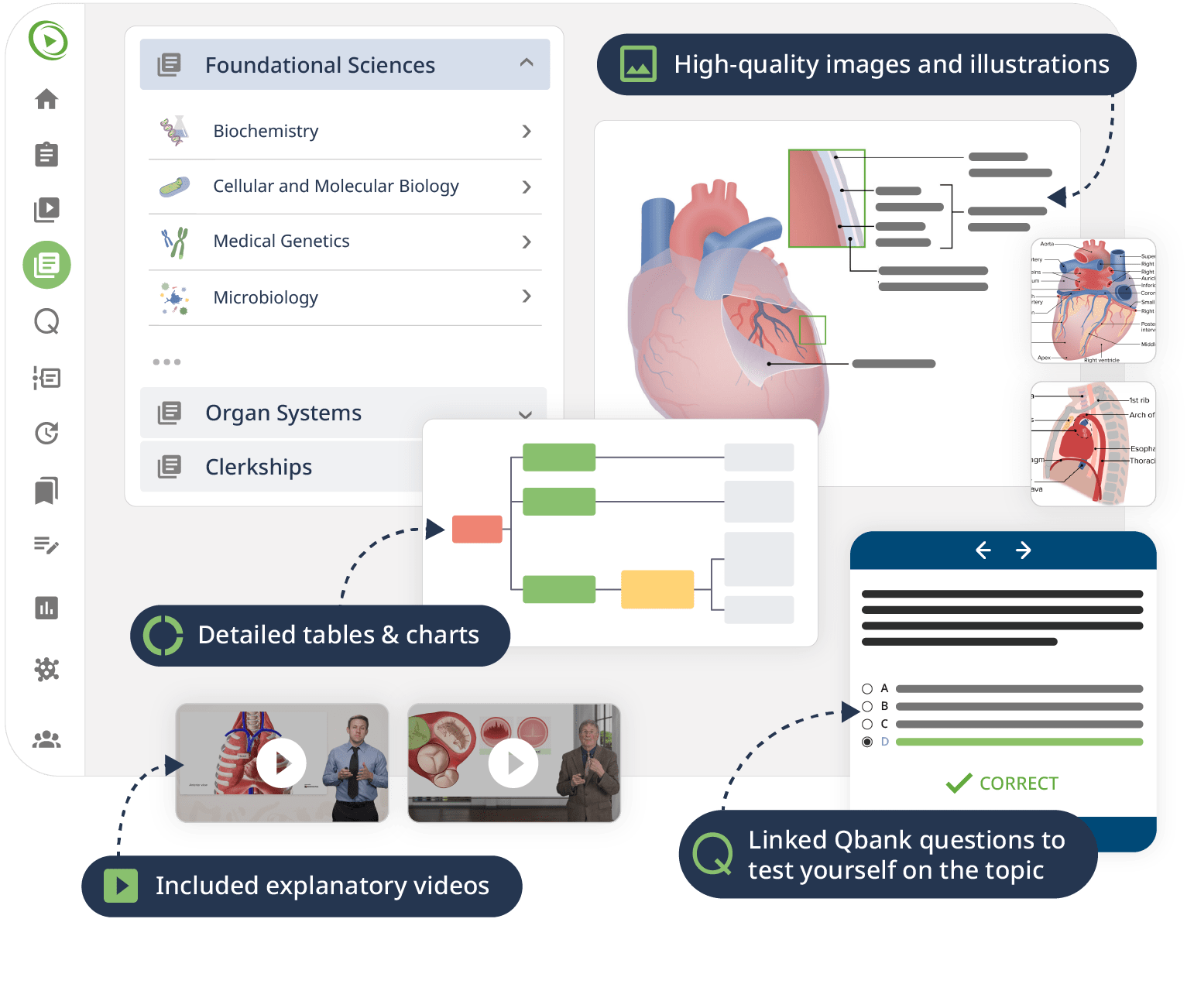
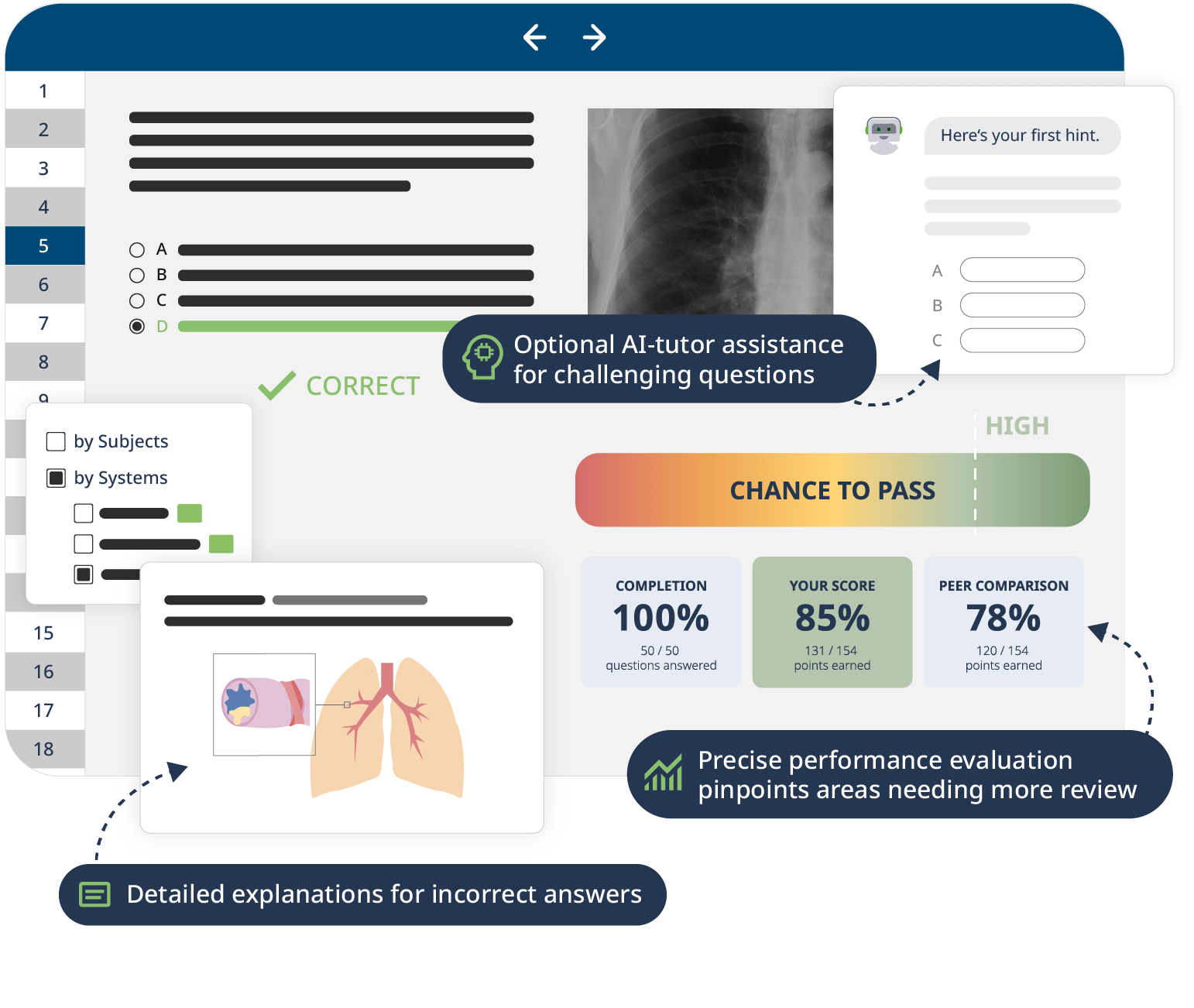
The combination of Video Lessons with interactive quiz questions, downloadable study materials, and a USMLE-style Qbank makes it easy to understand and retain the topics. By the end of this course, you will have a solid foundation in histology, preparing you to excel in your exams and making you ready for further clinical studies building on the understanding of tissues in their normal state.