Master all exam-relevant pulmonology topics
Jeremy Brown, Professor of Respiratory Infection at UCL, leads you through the core topics of respiratory medicine
Respiratory conditions are very common and often serious, with both infectious diseases and chronic non-commutable conditions contributing to a large global health burden. The wide range of pathologies in the field make mastering the diagnosis and treatment of pulmonary conditions challenging.
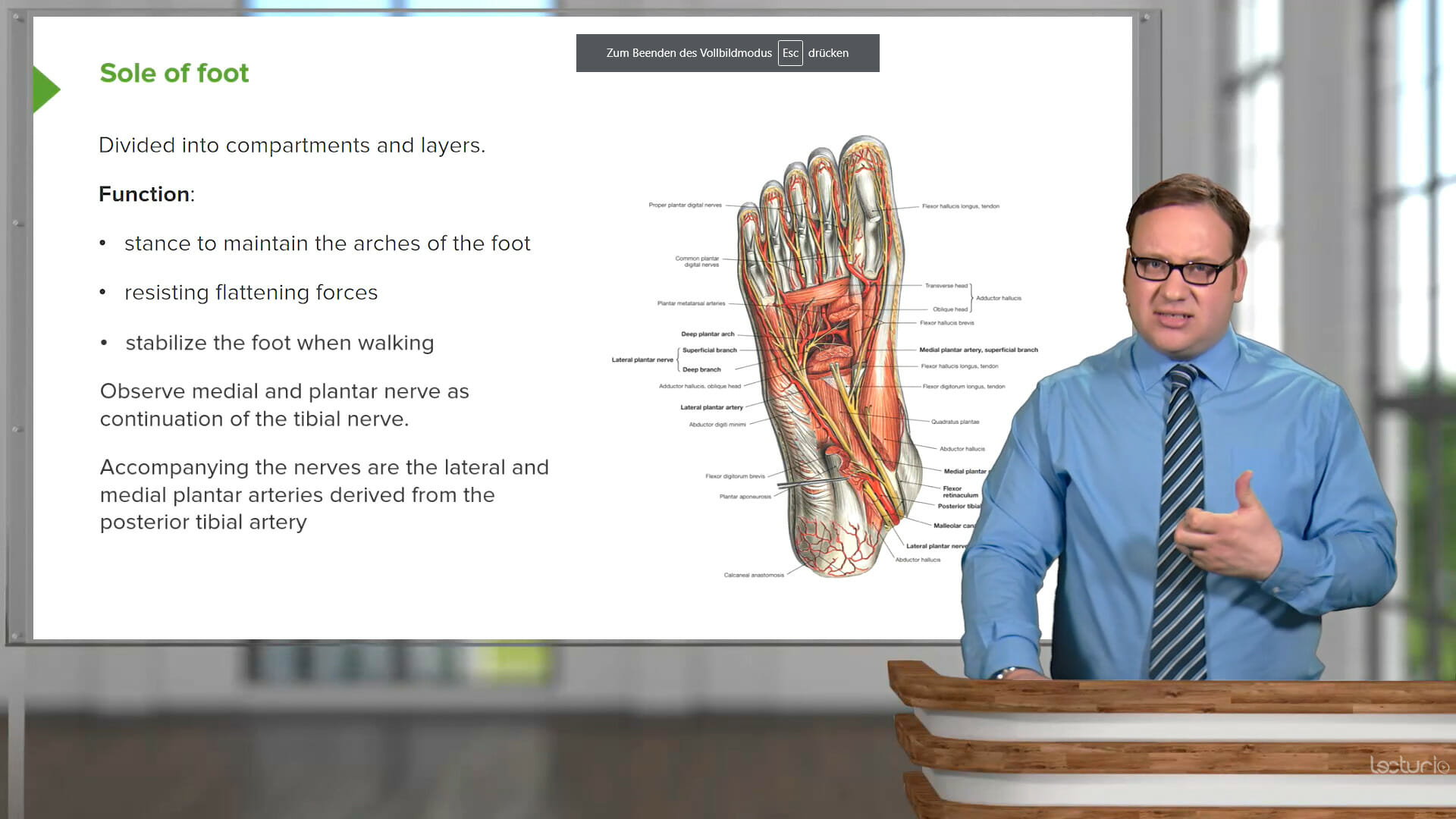
This course covers the causes, diagnosis, and treatment of key pulmonary conditions, from acute cases of pneumonia and bronchitis to long-term management of COPD and asthma. Experienced educator Jeremy Brown, PhD, walks you through the characteristics of each disease, making sure you not only understand the mechanisms and steps, but also are equipped to apply your learning to real clinical cases.
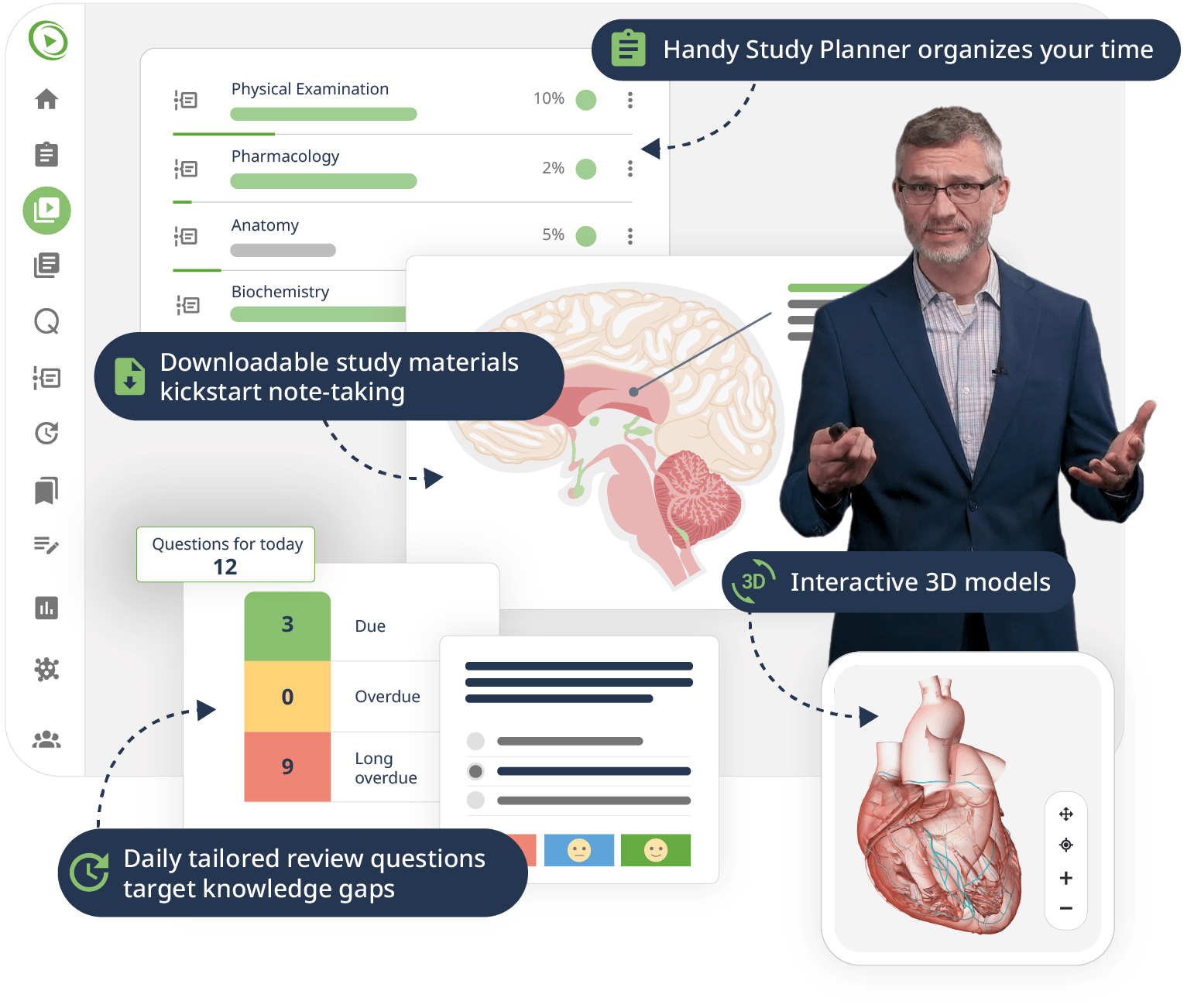
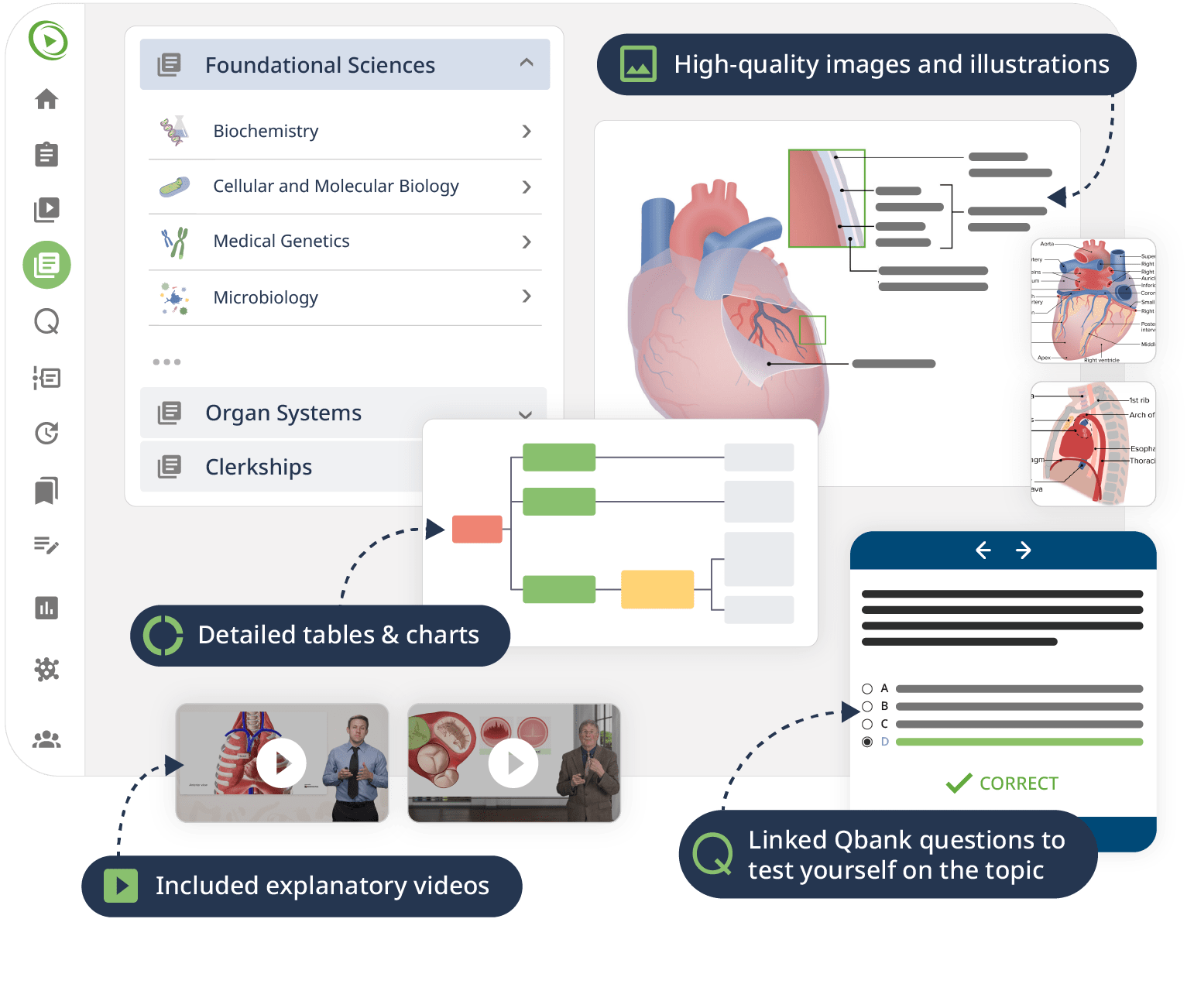
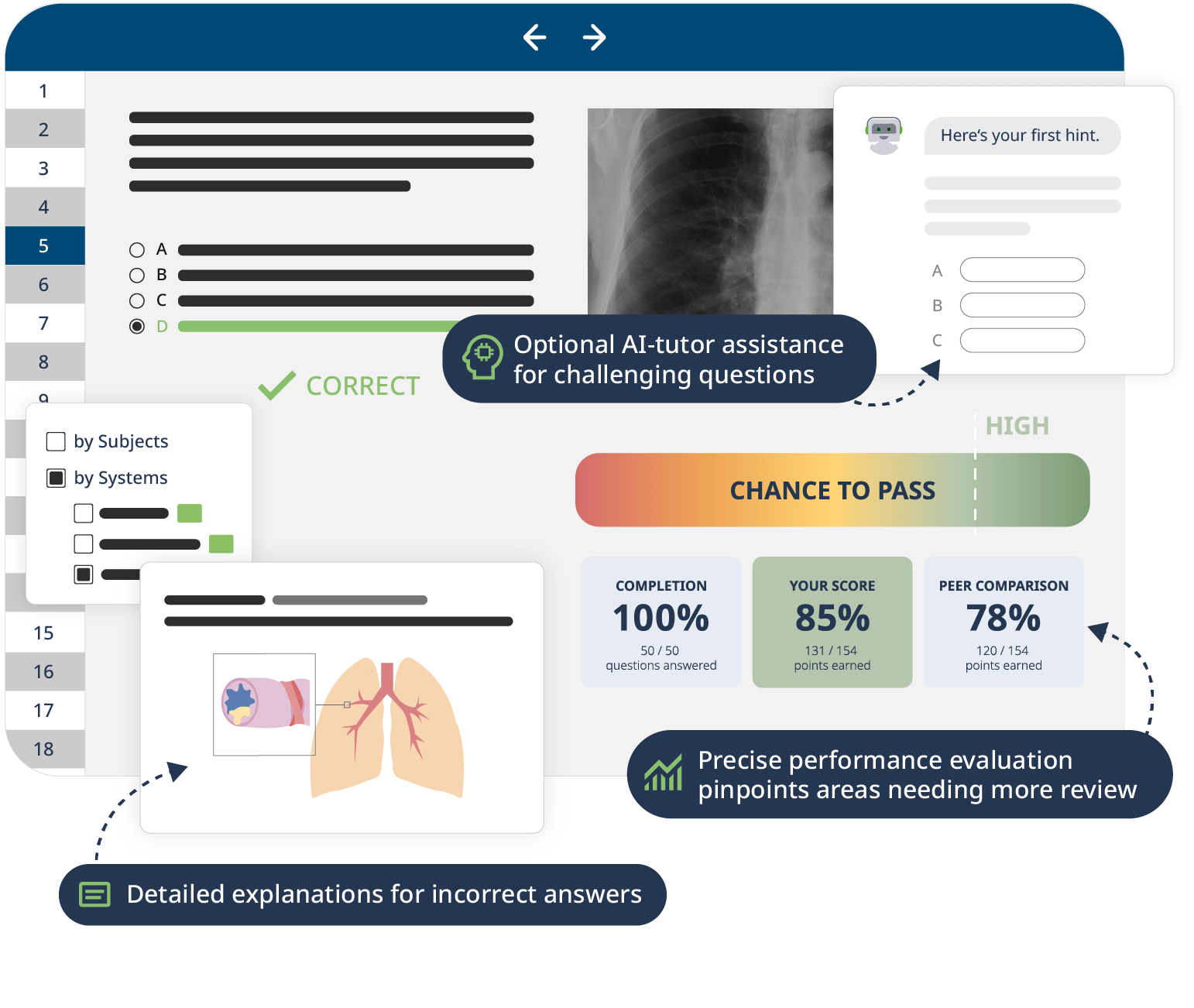
The combination of Video Lessons with interactive quiz questions, downloadable study materials, and a USMLE-style Qbank makes it easy to understand and retain the topics. By the end of this course, you will have a solid foundation in respiratory medicine and feel ready to effectively diagnose and treat a variety of pulmonary conditions.