What is COPD?
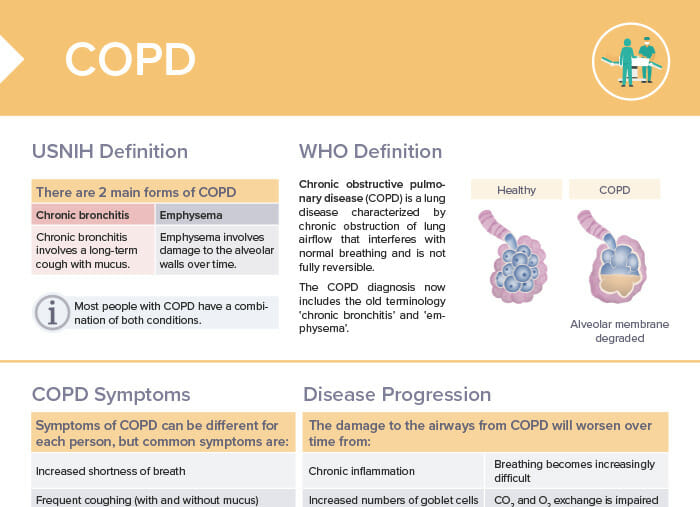
Chronic obstructive pulmonary disease (COPD) is a lung disease characterized by chronic obstruction of lung airflow that interferes with normal breathing and is not fully reversible. COPD is an umbrella term for two distinct respiratory conditions, emphysema and chronic bronchitis. They are both characterized by chronic inflammation, airflow limitation, and tissue destruction. While the condition is chronic and frequent exacerbations can occur, it is treatable through lifestyle measures and pharmacologic treatment.
What causes COPD?
The most common cause of COPD is long-term exposure to lung irritants (harmful particles or gases), the most common being cigarette smoke.
Other risk factors for the development of COPD include:
- Exposure to air pollutants in environment or workplace (dust, chemical fumes)
- Alpha-1 antitrypsin deficiency
- History of respiratory diseases
- Aging
- Interference with lung development e.g. through secondhand smoking in childhood
As a nurse, part of your role will be educating clients and communities about these risk factors and promoting behaviors to reduce risk, such as smoking cessation and avoiding exposure to lung irritants.
Click here for a step-by-step NCLEX question walkthrough about COPD ➜
What are the symptoms of COPD?
The symptoms of COPD can vary from person to person. Common symptoms of COPD include:
- Frequent coughing (with and without mucus)
- Increased breathlessness
- Wheezing
- Tightness in the chest
- Narrowing and reduction in the number of small airways
- Air hunger
- Pursed-lip breathing
- Chronic cough
- Barrel chest
- Low oxygen level
- High carbon dioxide
What are the 4 stages of COPD?
The GOLD staging system of COPD by the Global Initiative for Chronic Obstructive Lung Disease classifies the severity of COPD into 4 stages, primarily based on lung function:
- Mild COPD:
- Chronic cough possible
- FEV1: >= 80%
- Moderate COPD:
- Symptoms more noticeable (breathlessness, cough, sputum production)
- FEV1: 50–80%
- Severe COPD:
- More severe breathlessness
- Possible fatigue, respiratory infections, exacerbations
- FEV1: 30–50%
- Very severe COPD (end-stage COPD):
- Poor quality of life, dyspnea even at rest
- FEV1: < 30% of expected value or < 50% with chronic respiratory failure
Note: While classifying COPD into these stages can be helpful, individual symptoms and impact of the disease can vary significantly.
Emphysema vs COPD: What is the difference?
Emphysema is a type of COPD. COPD is an umbrella term that includes both chronic bronchitis and emphysema.
Emphysema specifically involves damage to the alveoli (air sacs) in the lungs, leading to shortness of breath. Chronic bronchitis involves inflamed airways and mucus production. Patients can have one or both conditions. Diagnosis and management require healthcare provider input.
Chronic bronchitis
- Chronic bacterial colonization
- Inflammation of bronchial tubes
- Thick mucus limits air exchange.
Emphysema
- Alveoli damaged and enlarged
- Membrane between alveolar sacs destroyed
- Air trapping limits air exchange.
Bonus download: pharmacological treatment of COPD
COPD Medications
Causes, symptoms, similarities and differences, diagnosis and treatment of Cushing Disease and Cushing Syndrome
How does COPD progress?
The damage to the airways from COPD will worsen over time from:
- Chronic inflammation: continuous exposure to irritants like cigarette smoke leads to chronic inflammation in the airways; causes the airway walls to thicken and become scarred
- Increased mucus production: due to increased numbers of goblet cells and mucus gland hyperplasia; further obstructs airway
- Loss of elasticity: alveolar walls in the lungs become damaged; leads to the loss of elasticity in the lung tissues, making it harder for the lungs to expand and contract during breathing
- Air trapping in lungs: due to the collapse of small airways and destruction of alveolar walls; further impairs the exchange of oxygen and carbon dioxide
- Pulmonary fibrosis: formation of scar tissue in the lungs; further restricts airflow
Signs of COPD getting worse
- Increased shortness of breath
- Frequent respiratory infections
- Increased fatigue
- Increased coughing
- Changes in mucus
- Decreased activity
- Weight loss
- Swelling in ankles, feet, or legs
If you notice these signs in your client, it’s important to report them to the healthcare provider as soon as possible for further assessment and treatment adjustments.
What is a COPD flare-up/exacerbation?
A COPD exacerbation is a period of time when COPD symptoms are significantly worse than usually. Exacerbations may be triggered by respiratory infections or exposure to environmental pollutants. COPD exacerbations can be serious and lead to other complications like respiratory failure, so it’s important to seek medical attention promptly. As a nurse, part of your role will be teaching clients to recognize the signs of a flare-up and understand when to seek help, as well as how to avoid known triggers.
Symptoms include:
- Increased shortness of breath
- Increased coughing
- Changes in the color, thickness, or amount of mucus
- Increased fatigue
- Difficulty sleeping
- Decreased appetite
- Confusion or decreased alertness (in severe cases)
How is COPD treated?
Some specific aspects of COPD treatment from the perspective of nursing care include:
- Medication management: educating clients on how to properly use prescribed medications/inhalers, such as bronchodilators, corticosteroids, or antibiotics
- Patient education on medication adherence, how to recognize and manage exacerbations, and lifestyle modifications such as smoking cessation, exercise, and a healthy diet
- Breathing techniques and exercise: teaching strategies to manage shortness of breath, encouraging physical activity
- Managing oxygen therapy and teaching clients and families how to safely use and maintain oxygen equipment at home
- Monitoring vital signs, lung function, and overall symptoms
- Care coordination with respiratory therapists, physiotherapists, dietitians, and social workers
- Emotional support for client and family
- End-of-life care: discussions about advance directives, palliative care options, and hospice care in advanced cases
In general, the nursing care for a client with COPD should be individualized, client-centered, and focused on optimizing quality of life and reducing the risk of exacerbations.
Lifestyle measures
- Smoking cessation, if applicable
- Pulmonary rehabilitation
Pharmacological treatment of COPD
Long-term treatment:
- Bronchodilators
- Promote smooth muscle relaxation and prevent bronchoconstriction
- LABAs, LAMAs, methylxanthines
- Inhaled corticosteroids
- Decrease inflammation
- Combine with LABA or LAMA
- Beclomethasone
- Budesonide
- Fluticasone
- Methylxanthines
- Phosphodiesterase-4 inhibitors
- Used in severe cases
- Reduce inflammation by preventing breakdown of intracellular cyclic AMP
- Roflumilast
Acute treatment:
- Short-acting bronchodilators (SABAs)
- Oral corticosteroids
- Antibiotics if concern for bacterial infection
- Oxygen therapy, ranging from nasal cannula to mechanical ventilation based on severity
Emphysema vs COPD: What is the difference?
Emphysema is one of the 2 main forms of COPD: chronic bronchitis and emphysema.
- Chronic bronchitis: involves a long-term cough with mucus
- Emphysema: involves damage to the alveolar walls over time
Note: Most people with COPD have a combination of both conditions.
Asthma vs COPD: What is the difference?
The difference between asthma and COPD is based on the combination of conditions and symptoms present:
- Asthma with reversible airflow obstruction → not COPD
- Chronic bronchitis and/or emphysema but no airflow obstruction → not COPD
- Chronic bronchitis and/or emphysema with non-reversible airflow obstruction → COPD
Asthma–COPD overlap syndrome is identified in clinical practice by the features that it shares with both asthma and COPD. (Global Initiative for Chronic Obstructive Lung Disease (GOLD) and GINA Science Committees)