Autoimmune Hemolytic Anemia
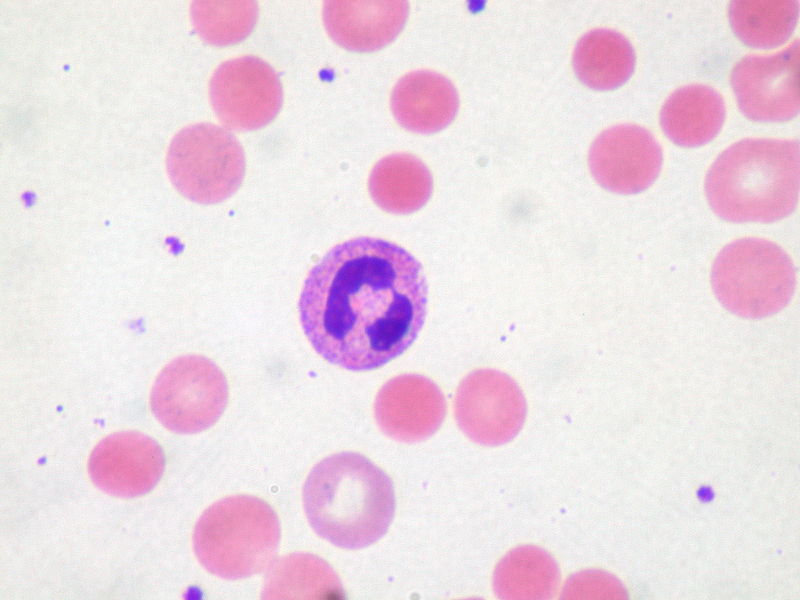
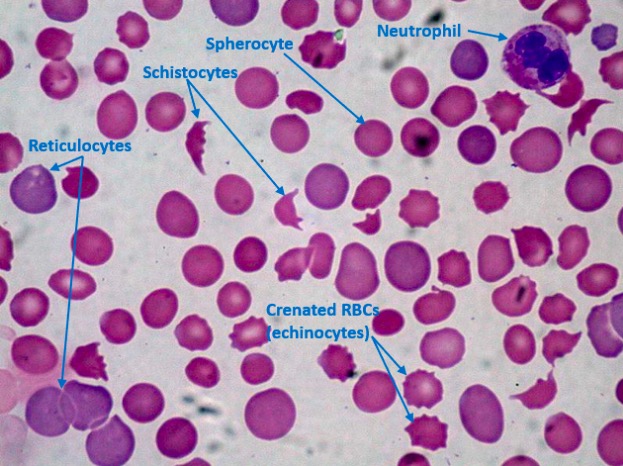
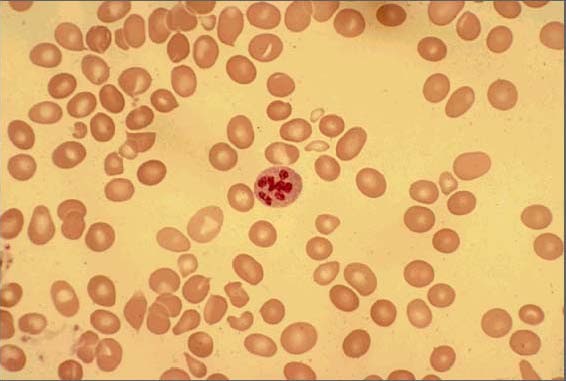
Overview Definition Autoimmune hemolytic anemia (AIHA) is hemolysis or premature destruction of RBCs due to autoantibodies. There are 2 categories of AIHA based on the thermal reactivity of autoantibodies: Epidemiology Etiology Warm AIHA: Cold AIHA: Mixed-type AIHA: Specific causes of AIHAs Table: Specific causes of warm AIHA (antibody type mostly IgG) Type Specific cause Primary […]
Hodgkin Lymphoma
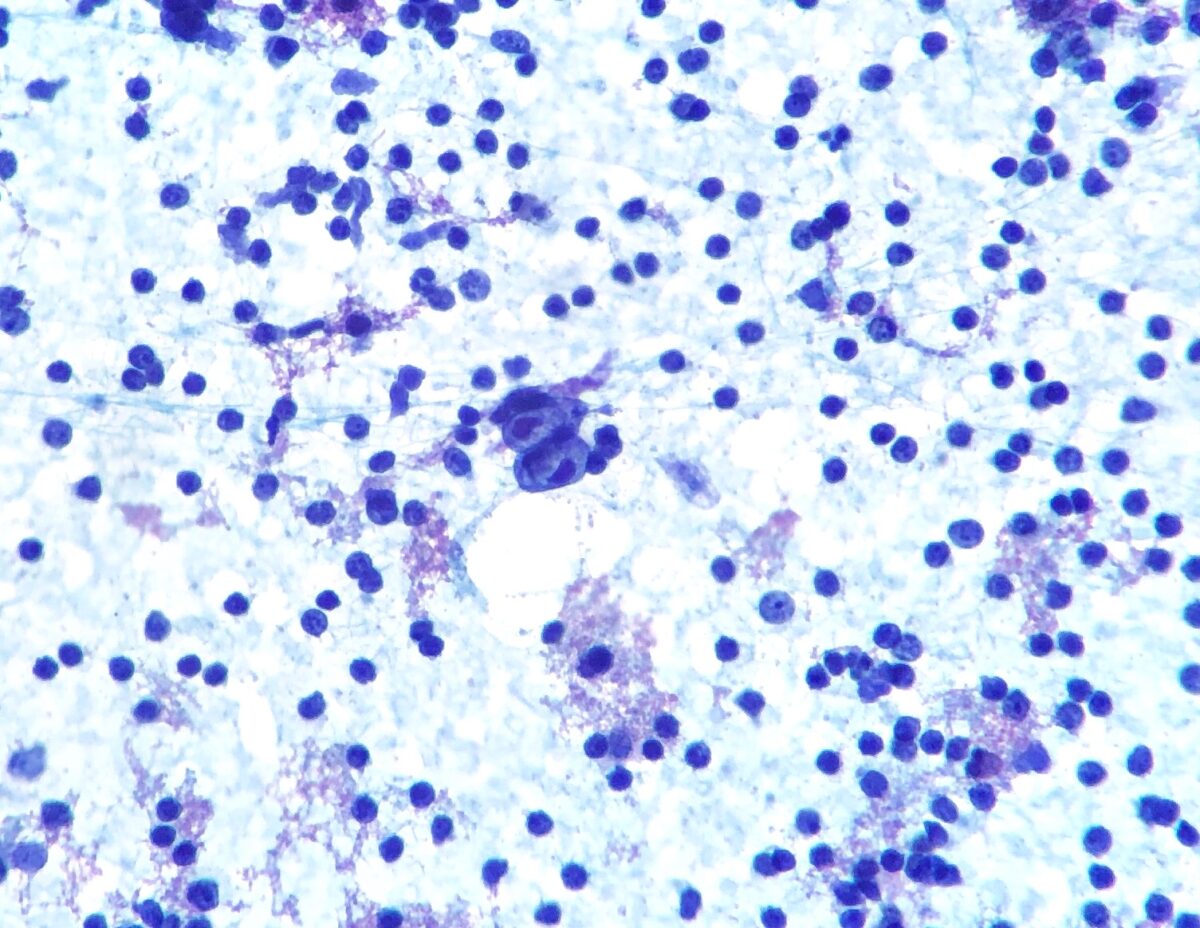
Overview Definition Hodgkin lymphoma (HL) is a monoclonal B-cell lymphoma (neoplasm) originating in lymph nodes in which the malignant Hodgkin/Reed-Sternberg (HRS) cells are mixed with a heterogeneous population of nonneoplastic inflammatory cells. Epidemiology Etiology Classification Based on WHO classification, HLs have the following types and subtypes according to immunophenotype and morphology. Classic HL (95%): Nodular […]
Methemoglobinemia
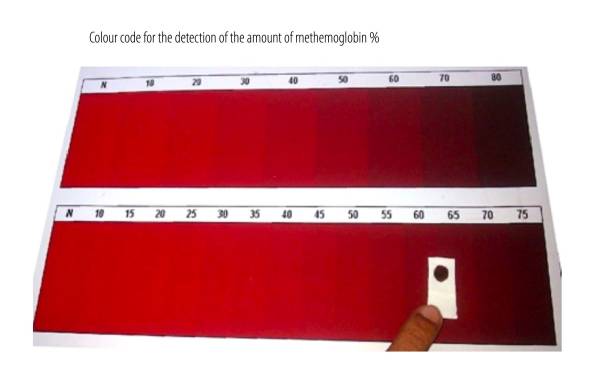
Overview Definition Methemoglobinemia occurs when RBCs contain elevated methemoglobin levels (normal range in adults is 0%–3%). Methemoglobin is a form of hemoglobin in which ferrous (Fe2+) heme iron is oxidized to the ferric (Fe3+) state, which is unable to bind O2. Etiology Congenital: Acquired due to exposure to oxidizing agents: Epidemiology Pathophysiology Normal hemoglobin Methemoglobin […]
Sideroblastic Anemia
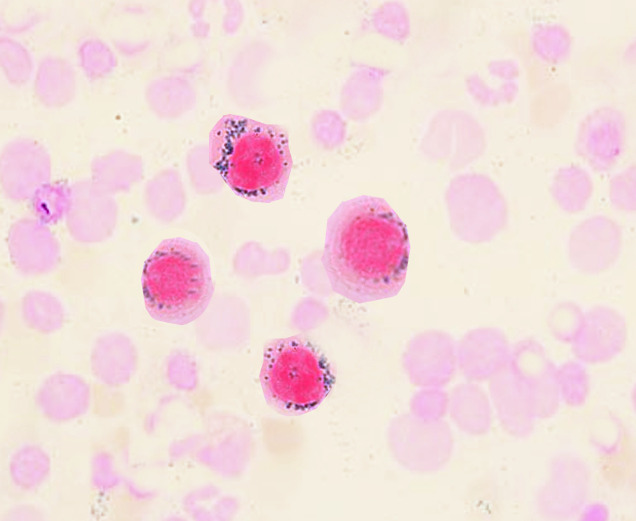
Overview Definition Sideroblastic anemias are a heterogeneous group of bone marrow disorders characterized by abnormal iron accumulation in the mitochondria of erythroid precursors. The distribution of the iron is ringlike around the nucleus, manifested by the precursors (ring sideroblasts) in the bone marrow. Epidemiology A rare disease → incidence and prevalence not well characterized Men […]
Thrombocytopenia
Overview Definition Thrombocytopenia is a deficiency of platelets, typically defined as < 150,000 platelets per microliter of whole blood. Epidemiology Classification Thrombocytopenia can be classified as mild, moderate, or severe on the basis of platelet counts: Etiology Thrombocytopenia can be caused by decreased production, increased destruction, or sequestration of platelets. Causes of thrombocytopenia Table: Causes […]
Megaloblastic Anemia
Overview Definition Megaloblastic anemia is a subset of macrocytic anemias characterized by increased RBC size and an arrest in nuclear maturation arising from abnormal cell division in erythroid precursors. Epidemiology Folate deficiency has been less common in the United States owing to folic acid fortification of grain products and the use of prenatal vitamins. The […]
Hypocoagulable Conditions

Overview Definition Hypocoagulable conditions, also known as bleeding disorders or bleeding diatheses, are a diverse group of diseases that result in abnormal hemostasis and increased bleeding risk. Physiologic hemostasis is dependent on normal structure and function of: Review of hemostasis The following is a summary of the process: Etiology The following conditions can lead to […]
Hemostasis
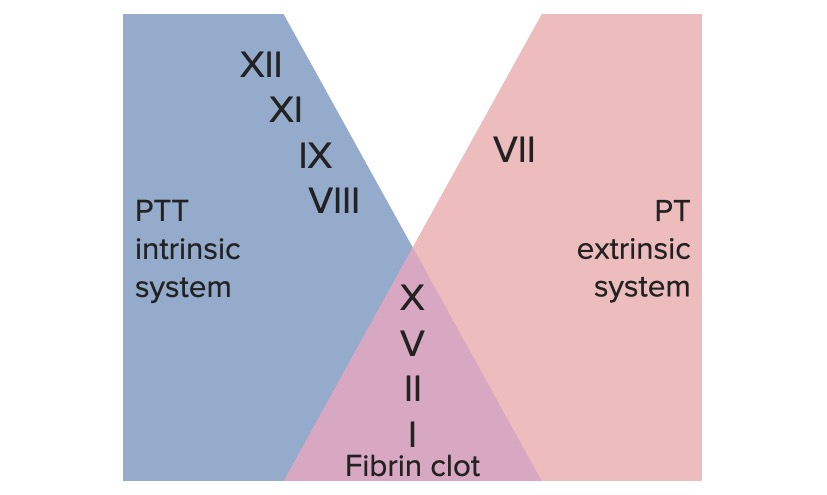
Definition and Phases Definition Hemostasis refers to the innate, stepwise body processes that occur following vessel injury, resulting in clot formation. Phases of the hemostatic process Vasoconstriction and Formation of the Platelet Plug Injured vessels vasoconstrict after endothelial injury. Additionally, exposure of blood to the subendothelial components triggers formation of the platelet plug. Vasoconstriction Endothelial […]
Coagulation Studies
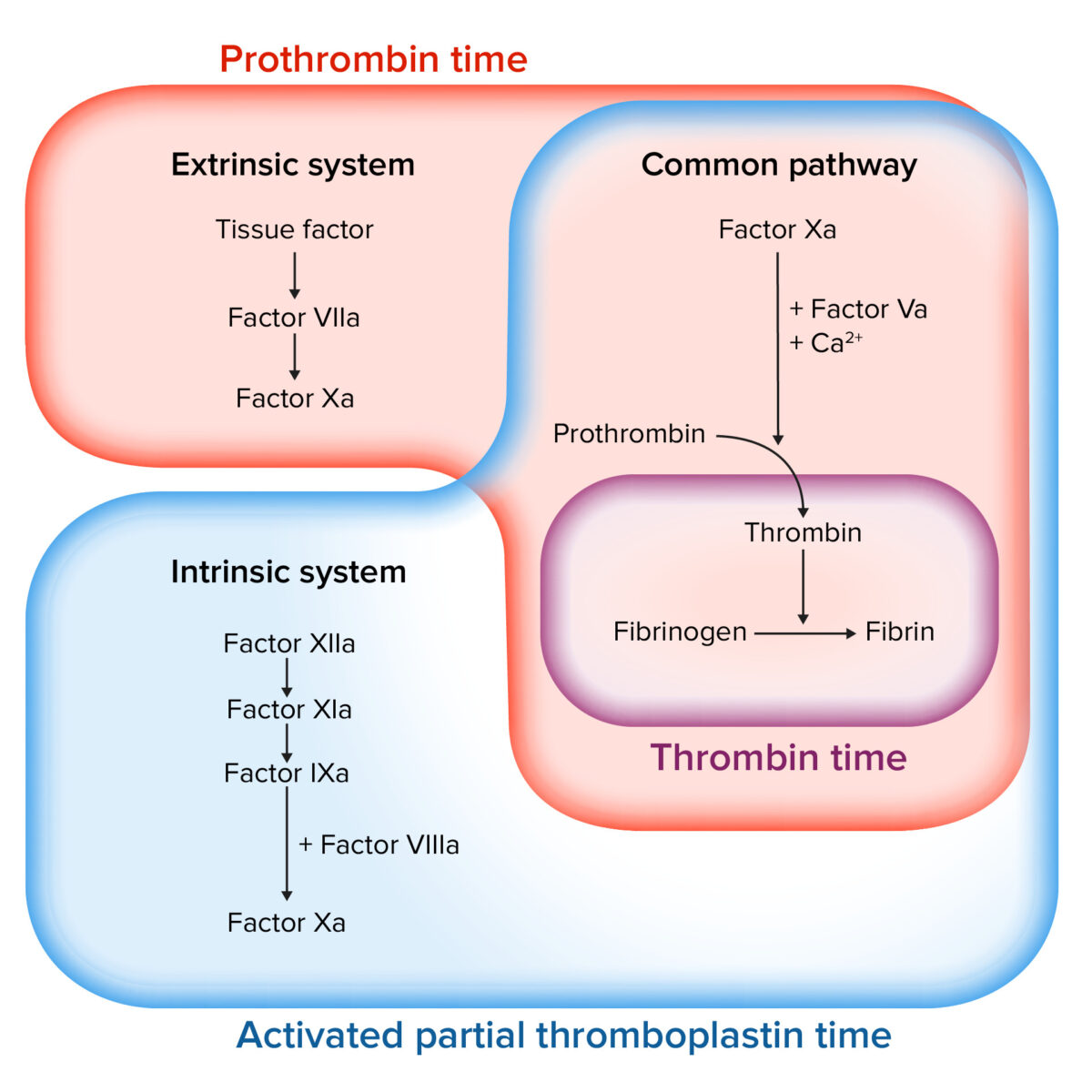
Overview Definition Coagulation studies are a group of hematologic studies that reflect the function of blood vessels, platelets, and coagulation factors, which all work in harmony to achieve hemostasis. Uses of coagulation studies Review: phases of the hemostatic process The following is a summary of the hemostatic process: Coagulation Studies The following studies can assist […]
Immune Thrombocytopenic Purpura

Overview Definition Immune thrombocytopenic purpura (ITP) is an acquired thrombocytopenia that results from autoantibodies targeting platelet antigens. Epidemiology Annual prevalence in the United States: 8 cases per 100,000 children 12 cases per 100,000 adults 40% of patients are younger than 10 years of age. The peak incidence in children is 2–4 years of age. The […]