Podcast with Stephen Pasquini, PA-C
Insert media file (up to 50 MB)
Presentation
Patient will present as → a 25-year-old woman presents to the ER after a syncopal episode. She had a loss of consciousness 3 times over the past 12 months. Each event occurred during or just after physical exercise. On PE: BP 110/70 mm Hg, HR 75/min, normal S1/S2, and an III/VI systolic ejection murmur is heard best at the left sternal border that decreases with squatting and increases with Valsalva and standing. The EKG shows a normal sinus rhythm with diffuse increased QRS voltage.
Pearls
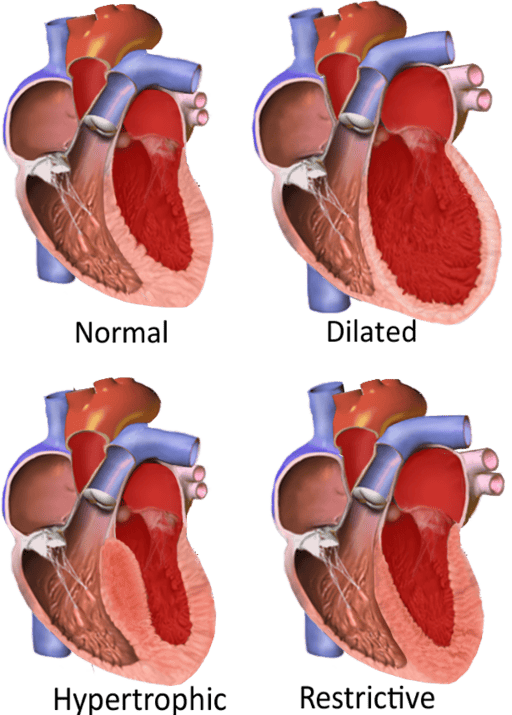
Hypertrophic cardiomyopathy (HCM) is a congenital or acquired disorder characterized by marked ventricular hypertrophy with diastolic dysfunction
- Myocardium gets sick, heavy, and hypercontractile
- Will present at an early age, patients may have chest pain, dyspnea, palpitations, syncope, and sometimes sudden death, typically triggered by exertion
- Characterized by a medium-pitched, mid-systolic crescendo-decrescendo murmur that decreases with squatting and increases with standing or Valsalva
- It is the most common cause of sudden cardiac death in young athletes in the United States. Intense competitive sports, strenuous exercise, and heavy lifting should be restricted because of the high risk of sudden cardiac death
- Genetic autosomal dominant affects the sarcomere (must screen family members if there is a known history). It looks like aortic stenosis and will present with angina, syncope, and heart failure.
- S4 gallop and apical lift with a thick, stiff left ventricle
- Jugular venous pulsations with a prominent “a” wave
“There are two main types of Hypertrophic cardiomyopathy: HCM vs. HOCM
- Obstructive: The most common type, hypertrophic obstructive cardiomyopathy (HOCM), means the wall (septum) between the left ventricle and right ventricle thickens. This can block (obstruct) blood flow from the left ventricle to the aorta (the body’s main artery).
- Nonobstructive: In nonobstructive HCM, the heart muscle thickens but doesn’t block blood flow.”
Diagnosis
Diagnosis is by echocardiography or MRI
Echocardiography is the key to diagnosis and will show left ventricular hypertrophy with a thickened septum, small left ventricle, and diastolic dysfunction
- EKG will show nonspecific ST and T-wave changes and left ventricular hypertrophy
The murmur will decrease with squatting or handgrip and get louder when patients stand or Valsalva
- Squatting increases venous return (preload) and, therefore, increases left ventricular chamber size and volume. If preload is increased, the end-systolic dimension of the left ventricle increases and there is less obstruction in the left ventricular outflow tract with a resulting decrease in murmur intensity
- If the venous return is decreased (standing), left ventricular chamber size decreases, which results in more obstruction and a resulting increase in murmur intensity
- Increase preload = squatting and handgrip
- Decrease preload = standing, and Valsalva
Treatment
β-blockers (metoprolol) and/or rate-limiting Ca channel blockers (usually verapamil) to decrease myocardial contractility and slow the heart rate and thus prolong diastolic filling and decrease outflow obstruction
- Avoid nitrates and other drugs that decrease preload (e.g., diuretics, ACE inhibitors, angiotensin II receptor blockers) because these decrease LV size and worsen LV function
- Digoxin is contraindicated since it increases the force of contraction, which can increase the obstruction
- Consider an implantable cardioverter-defibrillator for patients with syncope or sudden cardiac arrest
Flashcards
to be integrated if allowed