What are vasodilators?
Definition
Vasodilators are medications used to relax (dilate) blood vessels, which leads to a decrease in blood pressure.
How do vasodilators work?
Vasodilators relax the smooth muscle cells in the walls of blood vessels. Their widening decreases systemic vascular resistance and allows blood to flow more easily, lowering blood pressure and reducing the workload on the heart.
Indications
Vasodilators are used to treat various cardiovascular conditions including hypertension, heart failure, angina pectoris, and myocardial infarction. They can also be helpful for clients with Raynaud’s syndrome to alleviate the symptoms of reduced blood flow to the extremities.
What is splanchnic vasodilation?
Vasodilation in the blood vessels supplying blood to the GI organs is called splanchnic vasodilation. It can, for example, be caused by liver cirrhosis or sepsis. The increased blood flow to the splanchnic organs can lead to or exacerbate portal hypertension. Conditions involving splanchnic vasodilation can serve as a contraindication or warrant caution for vasodilators.
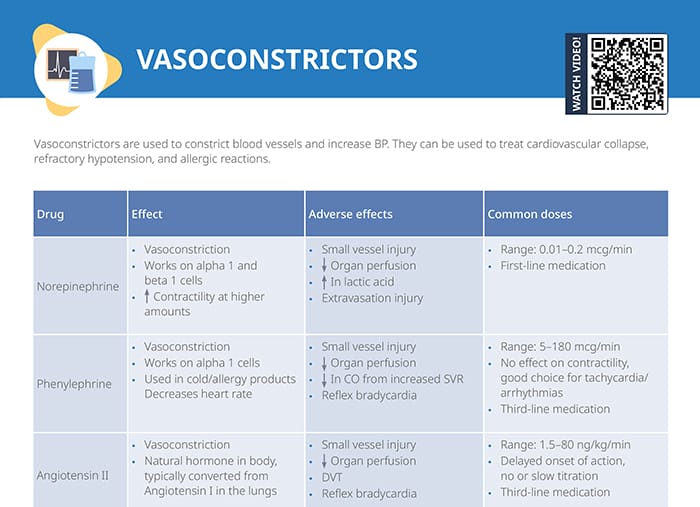
Overview of common vasodilators
Nitroglycerin
Effects:
- Vasodilation of arteries and veins
- < 100 mcg/min primary effect on venous dilation
- > 100 mcg/min primary effect on arterial dilation
Adverse effects:
- Decreased blood pressure
- Headache
- Reflex tachycardia
- Flushing
Common doses:
- Range: 5–200 mcg/min
- Must use polyethylene tubing to infuse
- Packaged in a glass bottle
- Titrate q 3–5 mins until therapeutic response achieved
- Do not abruptly discontinue
Nitroprusside
Effects:
- Vasodilates both arteries and veins
- Almost immediate reduction in preload and afterload
- Protect medication from light exposure
Adverse effects:
- Decreased blood pressure (rapid reduction)
- Nausea, vomiting
- Headache
- Lightheadedness
- Sweating
- Reflex tachycardia
- Risk for cyanide and thiocyanate toxicity
Common doses:
- Range: 0.1–3 mcg/kg/min
- Titrate slowly w/ caution, q 2- mins until therapeutic response achieved
Nicardipine
Effects:
- Vasodilates both arteries and veins
- Calcium channel blocker selective for smooth muscle dilation (not cardiac)
- Vasodilates pulmonary vasculature, ↑ blood flow to heart
Adverse effects:
- Decreased blood pressure
- Infusion site irritation
- Headache
- Dizziness
- Nausea, vomiting
- Reflex tachycardia
Common doses:
- Range: 5–20 mg/hr
- Increase by 5 mg during titration
- May cause negative inotropic effect in severe heart failure
- Rotate IV site q 12 hrs to prevent irritation
Natural vasodilators
Natural vasodilators can be beneficial for cardiovascular health and complement medical treatments. Known natural vasodilators include:
- Garlic
- Dark chocolate
- Nitric oxide-rich foods like leafy greens
- Nuts and seeds for L-arginine
- Hawthorn
Nursing considerations around vasodilation medications
- Hypotensive shock is a potential side effect of all vasodilators. Be prepared to treat per facility policy.
- Monitor for signs of cyanide and thiocyanate toxicity w/ nitroprusside:
- Confusion
- Seizures
- ↓ HR
- ↓ O2 saturation
- Metabolic acidosis
- Closely monitor hemodynamic status to prevent adverse effects and toxicity