What is an SBAR report?
An SBAR report is a tool of communication between members of the healthcare team about a client’s condition that follows the SBAR communication technique.
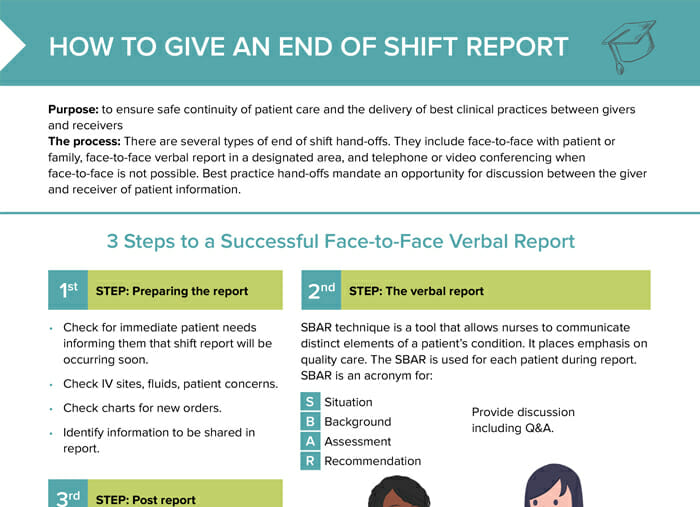
SBAR stands for:
- Situation
- Background
- Assessment
- Recommendation
What is the purpose of the SBAR technique?
Using the SBAR technique, a structured framework for communicating critical information about client conditions, helps ensure clear and concise exchange of this information between healthcare team members.
What are the components of an SBAR report?
The components of an SBAR report are:
- Situation: the current situation and reason for the report
- Background: relevant background information about the client’s condition, including medical history and the reason for current admission
- Assessment: clinical assessment findings including vital signs, changes in condition, and response to treatment so far
- Recommendation: recommendations for changes to the plan of care, further testing, or consultation with other healthcare professionals
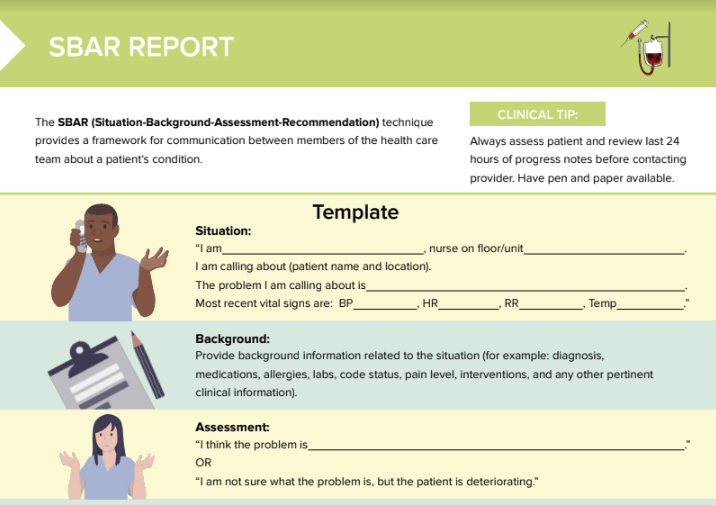
SBAR report template
Download the free PDF cheat sheet for the complete template with examples at a glance.
Situation template
“This is ________, nurse on floor/unit. I am calling about (patient name and location). The problem I am calling about is ______. Most recent vital signs are: BP___ , HR___ , RR___ , Temp___ .”
Background template
Provide background information related to the situation (for example: diagnosis, medications, allergies, labs, code status, pain level, interventions, and any other pertinent clinical information).
Assessment template
“I think the problem is ___________.”
OR
“I am not sure what the problem is, but the client is deteriorating.”
Recommendation template
- State your request, if you have one, AND ask what the provider wants you to do.
- Read back and verify all verbal or telephone orders.
- Request a read-back when reporting critical lab values.
SBAR report example
| Situation | “This is Mary RN, from the Med-Surg floor. I’m calling about Mr. Jones in room 101.He is complaining of shortness of breath and chest pain.His BP is 100/58, HR 124, RR 30, Temp 98.6 °F/37 °C.” |
| Background | “Mr. Jones had a myocardial infarction two weeks ago and was admitted yesterday for observation due to new reports of chest pain. He is restless and experiencing rapid, shallow breathing.” |
| Assessment | “Given his history, I am concerned he may be experiencing a new cardiac event.” |
| Recommendation | “I‘ve initiated 2L oxygen as per standing order. I am requesting an order for an EKG and for you to assess him immediately please. Is this agreeable to you? Do you have any further orders? Let me read these orders back to you.” |