What is the best treatment for Parkinson’s disease?
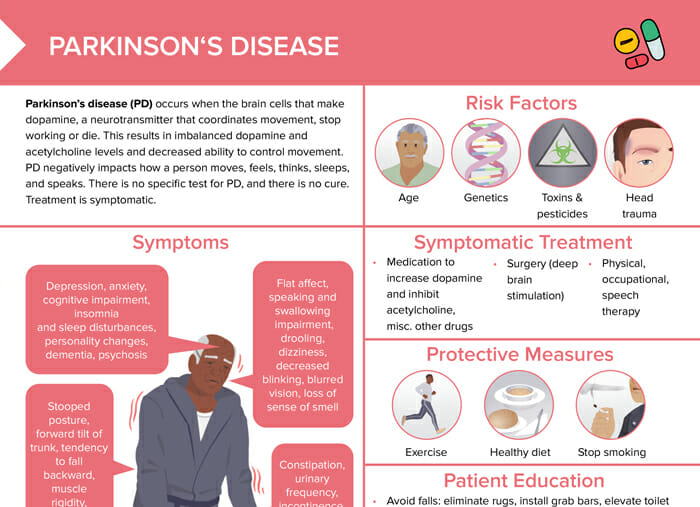
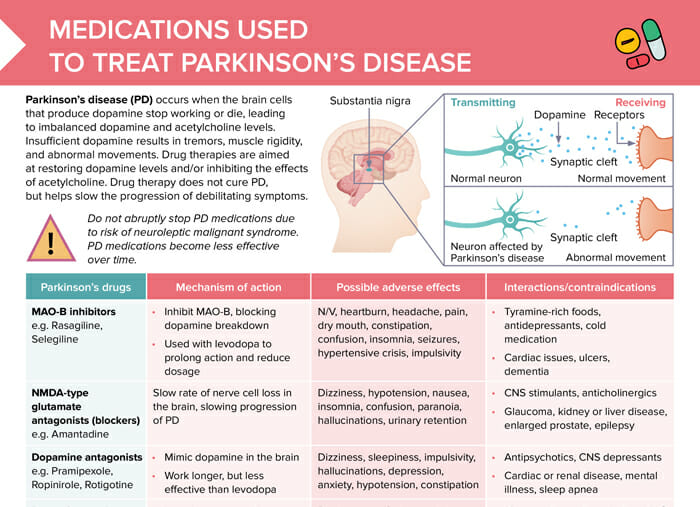
Parkinson’s disease (PD) occurs when the brain cells that produce dopamine stop working or die, leading to imbalanced dopamine and acetylcholine levels.
Insufficient dopamine results in tremors, muscle rigidity, and abnormal movements.
Drug therapies are aimed at restoring dopamine levels and/or inhibiting the effects of acetylcholine. Drug therapy does not cure PD, but helps slow the progression of debilitating symptoms.
Note: Do not abruptly stop PD medications due to risk of neuroleptic malignant syndrome. PD medications become less effective over time.
MAO-B inhibitors
Examples of MAO-B inhibitors are rasagiline or selegiline.
Mechanism of action of MAO-B inhibitors
MAO-B inhibitors inhibit MAO-B, blocking dopamine breakdown. They are used with levodopa to prolong action and reduce dosage.
Possible adverse effects of MAO-B inhibitors
- N/V
- Heartburn
- Headache
- Pain
- Dry mouth
- Constipation
- Confusion
- Insomnia
- Seizures
- Hypertensive crisis
- Impulsivity
Interactions and contraindications to MAO-B inhibitors
MAO-B inhibitors can interact with tyramine-rich foods, antidepressants, and cold medications. Contraindications include cardiac issues, ulcers, and dementia.
NMDA-type glutamate antagonists (blockers)
An example of an NMDA-type glutamate antagonist is amantadine.
Mechanism of action of NMDA-type glutamate antagonists
NMDA-type glutamate antagonists mimic dopamine in the brain. They work longer, but are less effective than levodopa.
Possible adverse effects of NMDA-type glutamate antagonists
- Dizziness
- Hypotension
- Nausea
- Insomnia
- Confusion
- Paranoia
- Hallucinations
- Urinary retention
Interactions and contraindications to NMDA-type glutamate antagonists
NMDA-type glutamate antagonists can interact with CNS stimulants and anticholinergics. Contraindications include glaucoma, kidney or liver disease, enlarged prostate, and epilepsy.
Dopamine antagonists
Dopamine antagonists include pramipexole, ropinirole, rotigotine.
How do dopamine antagonists work?
Dopamine antagonists mimic dopamine in the brain. They work longer, but are less effective than levodopa.
Possible adverse effects of dopamine antagonists
- Dizziness
- Sleepiness
- Impulsivity
- Hallucinations
- Depression
- Anxiety
- Hypotension
- Constipation
Interactions and contraindications to dopamine antagonists
Antipsychotics and CNS depressants can interact with dopamine antagonists. Contraindications include cardiac or renal disease, mental illness, and sleep apnea.
Dopamine prodrugs
The best-known dopamine prodrug is levodopa/carbidopa.
Mechanism of action of dopamine prodrugs
Levodopa crosses the blood–brain barrier and is converted into dopamine. Carbidopa prevents the breakdown of levodopa before it reaches the brain.
Possible adverse effects of dopamine prodrugs
- Dizziness
- Confusion
- Anxiety
- Depression
- Hallucinations
- Impulsivity
- Fatigue
- N/V
- Constipation
- Hypotension
- Dyskinesia
- Neuroleptic malignant syndrome
Interactions and contraindications to dopamine prodrugs
Dopamine prodrugs can interact with 1st-generation antipsychotics, MAO inhibitors. A high-protein diet can influence their effect as well.
Contraindications include glaucoma, a history of melanoma, diabetes, ulcers, cardiac or liver disease, and mental illness.
COMT inhibitors
A prominent example of a COMT inhibitor is opicapone.
Mechanism of action of COMT inhibitors
COMT inhibitors protect levodopa from breakdown by the COMT enzyme.
COMT inhibitors side effects
- Constipation
- Dry mouth
- Dizziness
- Dyskinesia
- Hallucinations
- Behavior changes
Interactions and contraindications to COMT inhibitors
Interactions include MAOs, antihypertensives, CNS depressants. Contraindications include mental illness, sleep apnea, and liver or kidney disease.
Anticholinergics
An example of an anticholinergic is benztropine.
What do anticholinergics do?
Anticholinergics block the action of acetylcholine. This helps decrease muscle stiffness, sweating, saliva production, and difficulty walking.
Possible adverse effects of anticholinergics
- Dry mouth
- Constipation
- Tachycardia
- Sedation
- Dizziness
- Restlessness
- Nervousness
- Insomnia
Interactions and contraindications to anticholinergics
Substances that can interact with anticholinergics include lisinopril, levothyroxine, antidepressants, antipsychotics, alcohol, and many other drugs.
Contraindications are glaucoma, enlarged prostate, liver disease, and urinary blockage.