What is Parkinson’s disease?
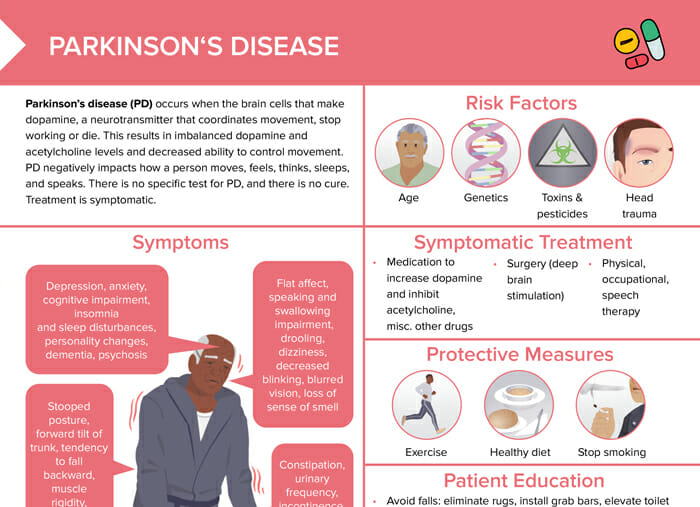
Parkinson’s disease (PD) is a chronic, progressive neurodegenerative disorder. It occurs when the brain cells that make dopamine, a neurotransmitter that coordinates movement, stop working or die. This results in imbalanced dopamine and acetylcholine levels and decreased ability to control movement. PD negatively impacts how a person moves, feels, thinks, sleeps, and speaks. There is no specific test for PD, and there is no cure. Treatment is symptomatic.
What causes Parkinson’s disease?
The exact cause of Parkinson’s disease is unknown, but likely to involve genetic as well as environmental factors.
Risk factors associated with Parkinson’s disease include age, exposure to toxins and pesticides, head trauma, genetics, and a history of depression, anxiety, cognitive impairment, insomnia, and sleep disturbances.
What are the signs of Parkinson’s disease?
Parkinson’s disease is typically characterized by a combination of motor and non-motor symptoms.
Motor symptoms
- Tremor: often starts in a single hand, most noticeable at rest
- Bradykinesia (slowness of movement)
- Rigidity of limbs/trunk
- Postural instability (falls)
- Reduced facial expressions (hypomimia), a stooped posture, decreased arm swing while walking, and changes in speech and handwriting
Non-motor symptoms
- Mental health issues (depression, anxiety, apathy)
- Cognitive changes (mild cognitive impairment to potentially dementia later on)
- Sleep problems
- Autonomic dysfunction (constipation, urinary problems, sexual dysfunction, low blood pressure upon standing [orthostatic hypotension], and excessive sweating)
- Sensory changes (reduced sense of smell, pain, and altered vision)
It’s important as a nurse to remember that symptoms can vary widely among individuals and may progress at different rates. The management and care of clients with Parkinson’s disease should be tailored to their unique set of symptoms and challenges.
How long can you live with Parkinson’s?
Parkinson’s disease is not directly life-threatening. It may slightly reduce affected individuals’ life expectancy due to complications like falls or pneumonia. Disease progress is highly individual and the goal of nursing care is to improve clients’ quality of life over the course of the disease and their life as much as possible.
What are the stages of Parkinson’s disease?
The Hoen-and-Yahr scale is a common way to describe Parkinson’s disease progression and severity:
- Stage 1: mild symptoms only on one side of the body
- Stage 2: bilateral symptoms, but intact balance
- Stage 3: loss of balance, slowness of movement, falls
- Stage 4: noticeable incapacitation, assistance required for daily living
- Stage 5: around-the-clock nursing care needed
Note: The progression of Parkinson’s disease is highly individual, and not every affected person will go through every stage.
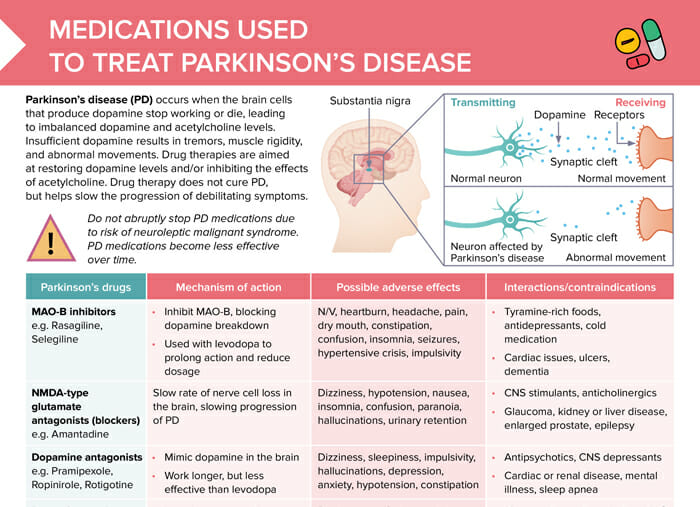
What is the treatment for Parkinson’s disease?
There is no cure for Parkinson’s disease, so treatment aims to alleviate symptoms and improve quality of life. Management of Parkinson’s needs to be tailored to the individual symptoms the client experiences, disease severity, age, and lifestyle.
Medical treatment
- Goal: increase dopamine levels or mimic dopamine effect in the brain
- Most common drugs: levodopa/carbidopa
- Also used: dopamine agonists, MAO-B inhibitors, COMT inhibitors
Recommended protective measures for fall-prevention
To prevent falls in individuals with Parkinson’s, it is recommended to:
- Eliminate rugs
- Install grab bars
- Elevate toilet seat
- Ensure adequate lighting
- Wear supportive and sturdy low-heeled shoes
- Utilize a rolling walker or cane when walking
- Maintain proper posture
- Consciously lift feet when walking
- Avoid prolonged sitting
Client education and lifestyle modifications
Encourage clients and make sure to:
- Avoid monoamine oxidase inhibitors
- Inform clients that effects of levodopa/carbidopa diminish over time
- Avoid high-protein foods with levodopa/carbidopa
- Encourage high-fiber soft diet, increase fluids
- Maintain regular bowel elimination
- Use adaptive silverware and cups with lids
- Use thickeners with liquids, as appropriate
Other measures
- Physical, occupational and speech and language therapy
- Surgical treatment (deep brain stimulation)
Parkinson’s disease: nursing diagnosis and nursing care plan
Nursing diagnoses for Parkinson’s disease are individualized based on the client’s specific symptoms, the stage of the disease, and other factors like their overall health status. Here are some potential nursing diagnoses that might be relevant:
- Impaired physical mobility:
- Related to rigidity, bradykinesia, and postural instability
- Care plan: maintain as much mobility and independence as possible through physical therapy and other interventions
- Impaired verbal communication:
- Due to voice and speech changes
- Care plan: Speech therapy can be beneficial.
- Risk for falls:
- Due to postural instability and gait disturbances
- The plan may involve safety measures in the home and use of assistive devices as needed.
- Activity intolerance:
- Related to fatigue and the energy-consuming effort of daily activities
- Care plan: might include energy conservation techniques and scheduled rest periods
- Constipation:
- Due to slower gut motility
- Care plan: dietary adjustments, increasing fluid intake, regular exercise, and potentially stool softeners or laxatives
- Chronic confusion/impaired memory:
- Care plan: strategies to support memory and cognitive function