Wound documentation: step-by-step
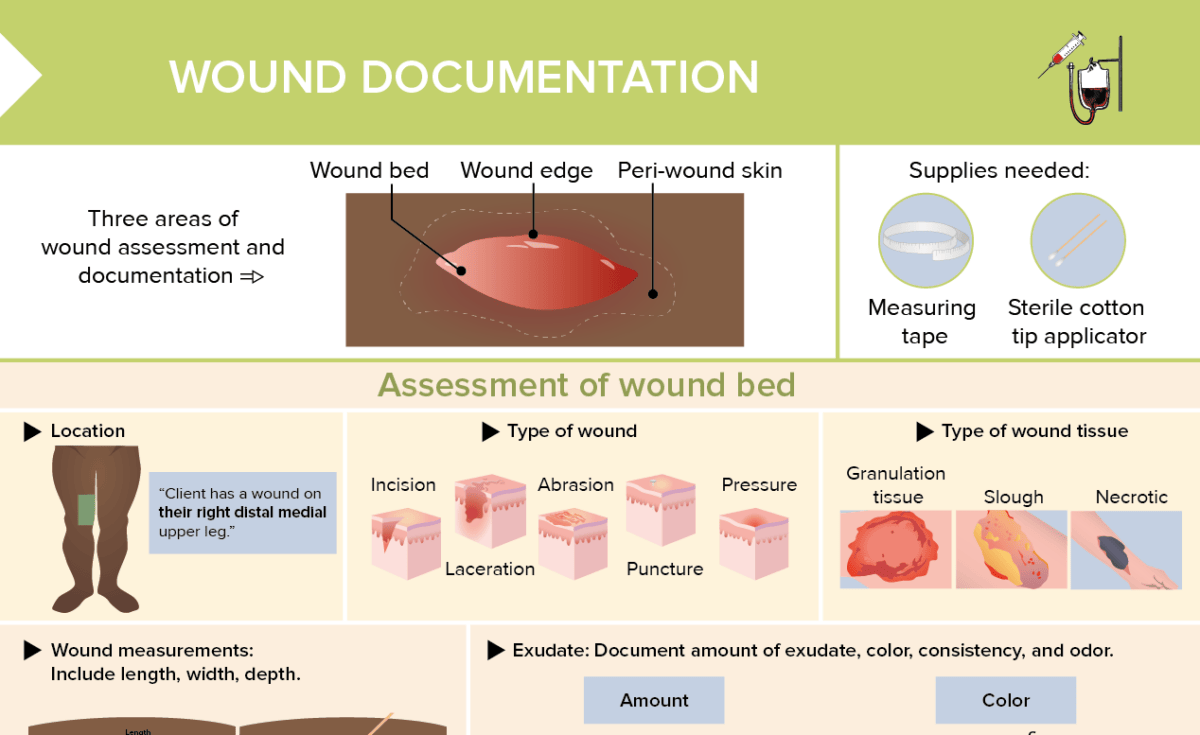
There are 3 overall areas of wound assessment and documentation:
- Wound bed
- Wound edge
- Peri-wound skin
How to assess the wound bed
Assess and document the following:
- Location: Where is the wound?
- Type: What kind of wound is it?
- Wound tissue: Granulation, slough, or necrotic tissue?
- Wound measurements: Include length, width, and depth.
- Exudate: Note amount of exudate, color, consistency, and odor.
How to assess the wound edge
Check for:
- Maceration (softening of tissues by soaking in fluids)
- Tunneling (erosion of tissue under wound edges causing pocket beneath skin)
- Rolled edge (wound edges rolling over themselves causing body to think wound has healed → healing ceases prematurely)
How to assess periwound skin
Assess for:
- Redness, warmth, edema, pain, skin breakdown
- Areas of maceration, excoriation, dry skin, hyperkeratosis, callous, eczema
What supplies are needed for assessing wounds?
- Measuring tape
- Sterile cotton tip applicator
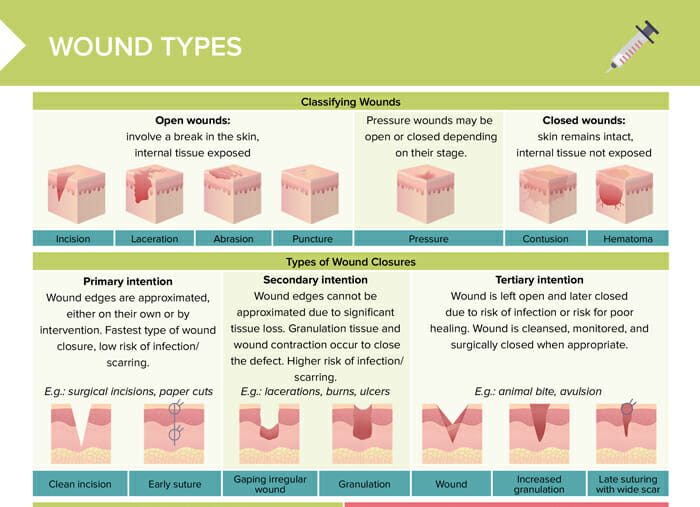
What are the different types of wounds?
The different types of wounds include:
- Incision
- Laceration
- Abrasion
- Puncture wound
- Pressure wound
How to classify and document wound exudate
- Amount: scant, moderate, large, copious
- Color: serous, sanguineous, serosanguineous, purulent
- Consistency: thin, thick, tenacious
- Odor: no odor, foul
What are the signs of abnormal wound healing?
Signs of abnormal wound healing include:
- Increased pain or swelling
- Stiff movement in affected limb
- Pus or odorous exudate
- Tunneling
- Erythema of peri-wound skin
- Wound gaping open or not healing
- Red streaking from or around the wound
When do wounds need to be documented?
- When a client is first admitted and wounds are found during head-to-toe assessment
- When there is a change in an existing wound
- On a regular schedule depending on the situation
- Following procedures related to the wound like dressing changes (documenting procedure as well as client’s response)
- Upon discharge or transfer
Wound documentation example
Date: June 28, 2023
Location: right lower leg, lateral
Size: length 4 cm, width 3 cm, depth 2 mm
Wound bed appearance: wound bed 70% covered in red granulation tissue, 30% yellow slough; no necrotic tissue present
Exudate: moderate amount of serosanguinous drainage noted, no odor detected
Pain: client reports pain level as 4 on a 0–10 scale, describes a ‘burning’ sensation
Peri-wound skin: skin pink, warm to touch, no signs of infection; mild edema present
Wound edges: well-defined, not rolled
Treatment: wound cleansed with normal saline; topical hydrogel applied then absorbent dressing applied and secured with paper tape
Client Response: tolerated procedure well, reports decreased pain following dressing application
Progress: compared to last assessment on June 26, 2023, wound length decreased by 1 cm, width remains the same, depth decreased by 1 cm; granulation tissue increased by 20%