What is uterine rupture?
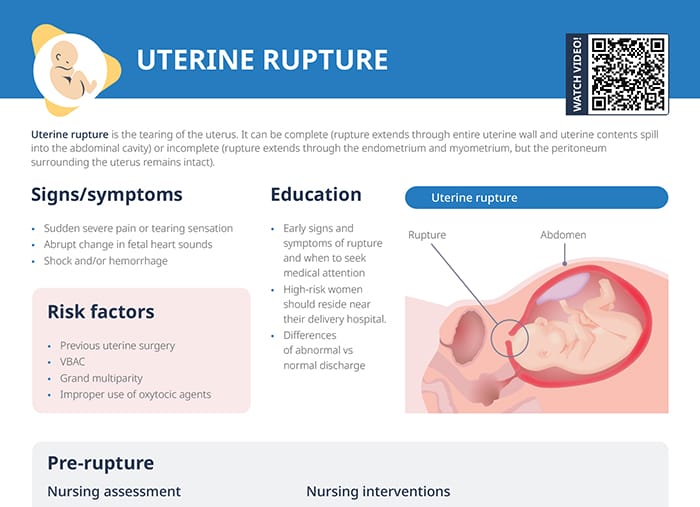
Uterine rupture is the tearing of the uterus.
Along with cord prolapse and shoulder dystocia, it is one of the more important complications in labor and delivery.
How common is uterine rupture?
Uterine rupture is rather rare, about 1 in 5700 to 1 in 50,000 pregnancies.
Uterine rupture types
Uterine rupture can be:
- Complete: Rupture extends through the entire uterine wall and uterine contents spill into the abdominal cavity.
- Incomplete: Rupture extends through the endometrium and myometrium, but the peritoneum surrounding the uterus remains intact.
Signs of uterine rupture
The most common sign of uterine rupture is an abrupt change in fetal heart sounds. Other symptoms are sudden severe pain or a tearing sensation, and shock and/or hemorrhage.
What causes uterine rupture?
Risk factors
Risk factors for uterine rupture include grand multiparity, previous uterine surgery, and vaginal birth after cesarean (VBAC).
Can pitocin cause uterine rupture?
Improper use of oxytocic agents like pitocin is an additional risk factor for uterine rupture, because it can lead to uterine hyperstimulation.
Pre-rupture nursing management
Assessment
- Recognize signs of impending rupture, immediately notify the physician, and call for assistance.
- Continuously monitor the fetal heart rate.
- Monitor maternal vitals and urine output.
- Assess for signs of shock and altered mental status.
- Assess the uterus.
Nursing interventions pre-rupture
- Facilitate rapid transfer of client/patient to OR for emergency C-section.
- Establish large-bore IV access to provide fluids, blood products, and medications as needed to address hypovolemia and shock.
- Administer oxygen (non-rebreather mask) and maintain a patent airway.
- Administer crystalloid and blood products to restore intravascular volume and maintain blood pressure to manage hemorrhage.
- Complete laboratory studies including type/cross.
Nursing care after uterine rupture
- Monitor vital signs and assess for changes in client’s condition.
- Closely monitor newborn and be prepared for potential resuscitation measures.
- Assess lochia and the amount of discharge.
- Scant: 1–2 inch stain (2–5 cm); ~10 mL loss
- Light: ~4 inch stain (10 cm); 10–25 mL loss
- Moderate: 4–6 inch stain (10–15 cm); loss of 25–50 mL loss
- Heavy: pad saturated in 1 hour
- Assess psychological/emotional state.
- Monitor intake and output, fluid status, and labs.
- Assess surgical incision C-section.
- Provide support for the client’s partner and family members.
- Control the pain with NSAIDs or narcotic analgesics.
- Offer specialized counseling to assist parents in coping with altered birth plan and/or fetal demise.
How long to wait to get pregnant after uterine rupture
Clients should be advised to observe about the same waiting period as women who deliver vaginally: 18–23 months until trying to conceive again.