What are traumatic brain injuries?
Traumatic brain injuries (TBIs) are dysfunctions caused by an outside force, usually a violent blow or jolt to the head or body. They range in severity from mild (concussion) to severe and can result in physical, cognitive, and emotional symptoms.
Immediate medical attention is essential, and management depends on the severity of the injury.
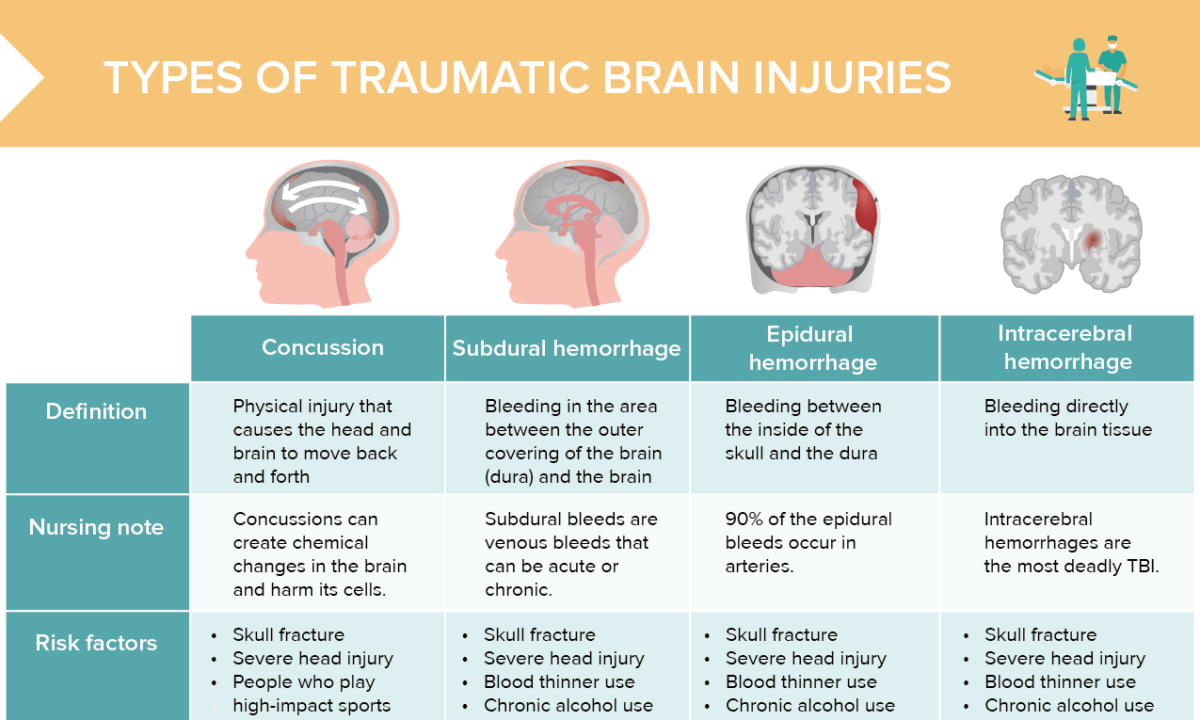
What is a concussion?
A concussion is a physical injury that causes the head and brain to move back and forth.
Concussions can create chemical changes in the brain and harm its cells.
Risk factors for concussion
- Skull fracture
- Severe head injury
- Playing high-impact sports
Signs and symptoms of concussion
- Headache
- GI upset
- Vision changes
- Confusion
- Balance changes
- Light sensitivity
- Fatigue
- Difficulty concentrating
- Memory loss
- Personality changes
- Loss of consciousness
How to check for concussion (eyes)
Common initial concussion tests involve assessing pupil reactions and abnormal eye movements.
Pupillary response tests for concussion
- Shine a penlight into one eye and observe the pupil’s reaction in both eyes. The pupil being illuminated should constrict (direct response), and the opposite pupil should also constrict (consensual response).
- Check for unequal pupil size (anisocoria). While some people naturally have slightly different pupil sizes, a significant disparity or a change after an injury may be concerning.
Eye movement tests for concussion
- Ask the client to follow a moving object, such as a finger or a pen, with their eyes only, not turning their head. The eyes should smoothly track the object.
- Check for nystagmus (involuntary rhythmic shaking or “jittering” of the eyes). While some nystagmus can be normal, sudden onset after trauma can be indicative of a brain injury.
- Ask the patient if they’re experiencing diplopia/double vision.
Convergence test for concussion
Ask the patient to focus on a close object (like a finger) moving towards the bridge of their nose. In a concussion, a patient might have difficulty converging their eyes or experience diplopia with this test.
What is a subdural hemorrhage?
Bleeding in the area between the outer covering of the brain (dura) and the brain is called subdural hemorrhage.
Subdural bleeds are venous bleeds that can be acute or chronic.
Risk factors for subdural hemorrhage
- Skull fracture
- Severe head injury
- Blood thinner use
- Chronic alcohol use
- People who play high-impact sports
- Older age (can be mistaken for dementia)
Signs and symptoms of subdural hemorrhage
- Worsening headache
- Personality changes
- Vision changes
- Confusion
- Fatigue
- Dysarthria
- Speech changes
- Partial body weakness
- Seizures
- Loss of consciousness
What is an epidural hemorrhage?
Epidural hemorrhage defines bleeding between the inside of the skull and the dura.
90% of the epidural bleeds occur in arteries.
Risk factors for epidural hemorrhage
- Skull fracture
- Severe head injury
- Blood thinner use
- Chronic alcohol use
- Skull fracture in childhood
Signs and symptoms of epidural hemorrhage
- Severe headache
- GI upset
- Anisocoria
- Confusion
- Dizziness
- Fatigue
- Partial body weakness
- Seizures
- Loss of consciousness
What is an intracerebral hemorrhage?
Intracerebral hemorrhage means bleeding directly into the brain tissue.
Intracerebral hemorrhages are the most deadly TBI.
Risk factors for intracerebral hemorrhage
- Skull fracture
- Severe head injury
- Blood thinner use
- Chronic alcohol use
- Hypertension
- Older age
- History of stroke
- Liver disease
Signs and symptoms of intracerebral hemorrhage
- Severe headache
- GI upset
- Vision changes
- Confusion
- Partial body weakness
- Balance changes
- Speech changes
- Seizures
- Loss of consciousness
Nursing care for traumatic brain injuries
- Perform regular neurological assessments.
- Regularly assess blood pressure and temperature.
- Review fall risk prevention strategies.
- Monitor for any new symptoms or increased intensity of present symptoms (e.g. increased blurry vision or more painful headaches).
- Educate client and caregivers on post-TBI care management.
- Educate on the importance of attending follow-up visits.