What is preeclampsia?
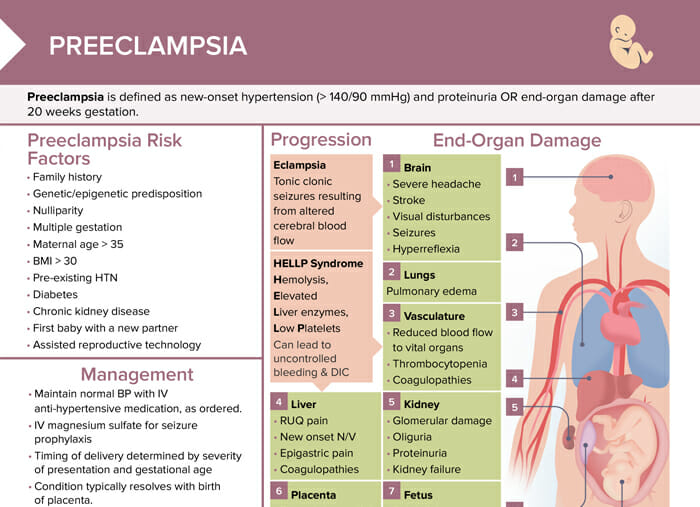
Preeclampsia as a medical diagnosis is defined as new-onset hypertension (> 140/90 mm Hg) and proteinuria OR end-organ damage after 20 weeks gestation.
Related videos
What causes preeclampsia (risk factors)?
Preeclampsia is believed to be caused by a combination of genetic, dietary, vascular, and immune factors. The exact cause is unknown.
Risk factors for developing preeclampsia include:
- Family history
- Genetic/epigenetic predisposition
- Nulliparity
- Multiple gestation
- Maternal age > 35
- BMI > 30
- Pre-existing HTN
- Diabetes
- Chronic kidney disease
- First baby with a new partner
- Assisted reproductive technology
How to prevent preeclampsia
Here are some key strategies:
- Education: Ensure that clients understand risk factors for preeclampsia as well as the importance of prenatal care.
- Monitoring: Regularly monitor blood pressure, urine protein levels, and report any sudden changes to a healthcare provider. Look out for signs and symptoms of preeclampsia such as persistent headaches, vision changes, upper abdominal pain, and sudden weight gain.
- Advocacy: Support and encourage clients to maintain a healthy lifestyle, including a balanced diet, regular physical activity, and avoiding substances like alcohol and tobacco.
- Medication management: For high-risk clients, low-dose aspirin may be recommended after the first trimester to help prevent preeclampsia. Ensure clients understand the medication regimen if prescribed.
- Early detection: Encourage regular prenatal visits to detect any issues as early as possible.
Preeclampsia progression: how quickly can it develop?
Preeclampsia can develop quite rapidly.
It typically occurs after the 20th week of pregnancy, but it can also develop in the late second trimester or even postpartum. Once signs and symptoms begin to manifest, preeclampsia can progress from mild to severe within a matter of days or weeks. In some rare and severe cases, it can progress to full-blown eclampsia (seizures caused by preeclampsia) within a very short time frame.
Preeclampsia generally starts with an improperly developed placenta, which can lead to placental ischemia. The body then responds by releasing substances into the bloodstream that can lead to systemic inflammation, blood vessel damage, and endothelial dysfunction, contributing to high blood pressure.
What are signs of preeclampsia?
The disease may begin with mild symptoms:
- Slight increase in blood pressure
- Protein in the urine
- Swelling in the hands and face
- Rapid weight gain due to fluid retention
- Sometimes headache, changes in vision, or upper abdominal pain
If not properly managed, preeclampsia can progress to severe preeclampsia, characterized by:
- More significant increases in blood pressure
- More protein in the urine
- Potentially severe headaches
- Blurred vision
- Impaired liver function
- Shortness of breath due to fluid in the lungs
- Decreased urine output
- Platelet count changes
In extreme cases, preeclampsia can progress to eclampsia, a serious condition that can cause seizures and is a major cause of maternal and fetal morbidity and mortality.
Preeclampsia nursing diagnoses
Potential nursing diagnoses related to preeclampsia may include:
- Anxiety: provide emotional support and concise information
- Powerlessness
- Risk for imbalanced fluid volume: risk factors are hypertension, altered kidney function; regular assessments for input/output, weight, and signs of fluid overload, if prescribed, administer diuretics
- Risk for maternal injury: prevent by providing safe environment in case of seizures or stroke secondary to severe preeclampsia/eclampsia; monitor neurologic status
- Risk for unstable blood pressure
Diagnostic lab values of preeclampsia
- Proteinuria: > 300 mg/24h, protein/creatinine ration > 0.3, dipstick 1 + persistent
- Thrombocytopenia: platelets < 100,000/µL
- Renal insufficiency: creatinine > 1.1 mg/dL or doubling of baseline
- Liver involvement: serum transaminase levels twice normal
How is preeclampsia managed during pregnancy?
Preeclampsia is managed by maintaining normal blood pressure with IV anti-hypertensive medication as ordered and administering IV magnesium sulfate for seizure prophylaxis. The timing of delivery is determined by the severity of presentation and gestational age. The condition typically resolves with the birth of placenta.
Nursing interventions that can help prevent end-organ damage in patients with preeclampsia
Nursing interventions that can help prevent end-organ damage in patients with preeclampsia include:
- Monitoring blood pressure and reporting elevations to the provider
- Evaluating deep tendon reflexes per protocol
- Assessing presence/progression of symptoms
- Administering medications as ordered
- Educating clients regarding condition/plan
- Assisting in preparation for birth, if indicated
Potential complications associated with preeclampsia
Potential complications associated with preeclampsia include:
- Eclampsia (tonic clonic seizures resulting from altered cerebral blood flow)
- HELLP syndrome (hemolysis, elevated liver enzymes, low platelets): can lead to uncontrolled bleeding and DIC
- Reduced blood flow to vital organs
- Glomerular damage
- Fetal distress and growth restriction
- RUQ pain
- New-onset N/V
- Epigastric pain
- Coagulopathies
- Placental syncytial stress and placental abruption
- Pulmonary edema