What is an NG tube?
An NG tube, or nasogastric tube, is a thin, flexible tube that is inserted through the nose, down the esophagus, and into the stomach. Its primary function is to either deliver nutrition, medication, or other necessary substances directly to the stomach (gavage), or to remove contents from the stomach (lavage), such as in the case of gastric decompression.
What are nasogastric tubes (NGTs) used for?
Examples of common applications of NG tubes:
- Nutritional support: delivering liquid nutrition into the stomach
- Medication administration: when clients can not swallow medications
- Gastric decompression: drain contents and air from stomach (e.g. for surgery)
- Collection of gastric content samples: to check for gastrointestinal bleeding
- Lavage: washing out the stomach e.g. in case of drug overdose
What is gastric decompression?
Gastric decompression refers to a procedure that removes air, fluids, and/or solid materials from the stomach to relieve pressure or distention. Indications include pre- or postoperative care, bowel obstruction, gastrointestinal bleeding, or gastroparesis.
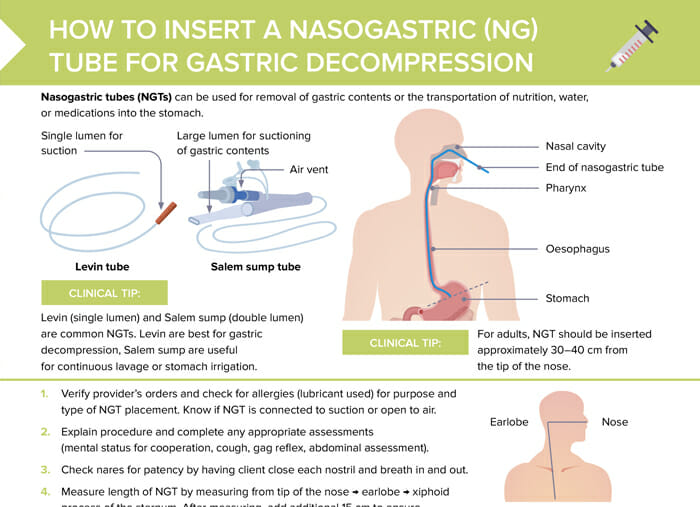
What are the two common types of NGTs?
The two common types of NGTs are Levin (single lumen) and Salem sump (double lumen).
What is the difference between Levin and Salem sump NGTs?
Levin NGTs:
- Best for gastric decompression
- Single-lumen tube → one channel
Salem sump NGTs:
- Useful for continuous lavage or stomach irrigation
- Double-lumen tube → two channels
How far should an NGT be inserted in adults?
For adults, an NGT should be inserted approximately 30–40 cm from the tip of the nose.
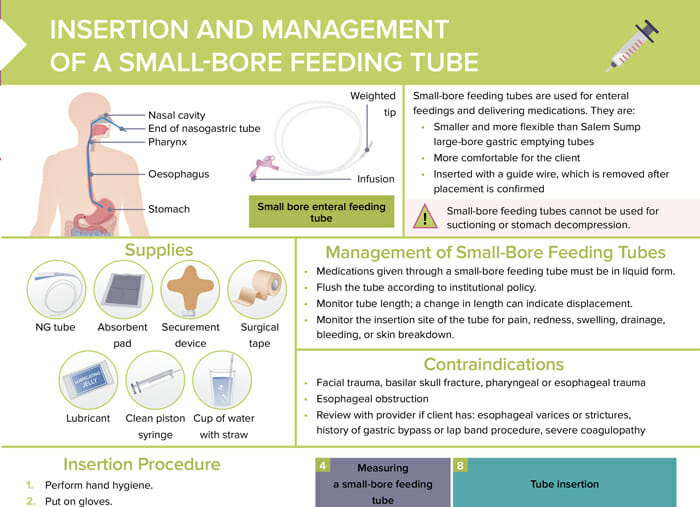
How to measure NG tube length
The nose-ear-xiphoid (NEX) measurement is a common method used to estimate the appropriate length of the NG tube. Remember that individual anatomy can vary, and other factors such as client position can also affect the exact length of tubing needed to reach the stomach.
Steps:
- Nose-to-earlobe: Hold the tip of the NG tube at the client’s nostril, the point where the tube will be inserted. Extend the tube in a straight line down to the client’s earlobe.
- Earlobe-to-xiphoid: From the earlobe, extend the tube to the xiphoid process, which is the pointy lower end of the sternum (breastbone) that’s located in the middle of the upper abdomen.
How to insert an NG tube, step-by-step
Steps:
- Gather supplies: NG tube, lubricant, pH test strips, stethoscope, gloves, tissues, tape, water, straw, syringe.
- Perform hand hygiene, don gloves.
- Explain the procedure and position the client upright or in semi-Fowler’s.
- Measure tube.
- Lubricate tube.
- Insert the tube with the client’s head tilted slightly forward. Advance within the nasal cavity floor towards the ear. When the tube reaches the nasopharynx, have the client tilt their head back and start to swallow (support by giving sips of water). Continue until premeasured length is reached.
- Verify placement.
- Secure tube.
What should you do if a client experiences difficulty breathing or starts choking during NGT insertion?
If a client experiences difficulty breathing or choking noises during NGT insertion, remove the tube and reattempt. Take care to reassure the client and call for help if needed.
A common reason for respiratory distress during NGT insertion is the tube was inserted into the trachea instead of the esophagus.
How to check NG tube placement
Verifying the placement of a nasogastric (NG) tube is a critical step in ensuring client safety. Misplaced NG tubes can lead to serious complications, such as aspiration pneumonia. There are several methods to verify placement:
- Radiographic confirmation:
- Preferred: confirmation by chest X-ray
- Typically done when the tube is first inserted, when there are difficulties placing the tube, or limited drainage.
- Aspiration of gastric contents:
- Aspirate fluid from the tube with a syringe.
- Gastric fluid is typically greenish, yellow, or clear with a slightly acidic pH (usually below 5.5): can be influenced by medications, food, disease → not a foolproof method.
- pH Testing:
- After aspirating, you can use pH paper to test the fluid.
- Stomach content typically has a pH below 5.5.
- Fluid from the lungs (if the tube is mistakenly in the lungs) or the intestine will typically have a higher pH.
- External measurement, visual inspection and auscultation:
- Tube should appear to follow the nasal cavity down into the throat.
- Keeping track of the external portion of the tube can give a rough estimate if the tube might have moved. Any significant changes should prompt a reevaluation of the tube’s position.
- When listening to the client’s stomach while injecting air into the tube, you should hear a distinct “whoosh” sound (not recommended or used often).
How to remove an NG tube
Steps:
- Explain procedure and gather supplies.
- Perform hand hygiene and don gloves.
- Position client upright or in semi-Fowler’s.
- Clamp tube if it is connected to a suction device and disconnect it.
- Ask client to take a deep breath and hold it to minimize discomfort. Remove the tube in one gentle, smooth, continuous motion. Avoid pulling too forcefully.
- Dispose of tube according to regulations.
- Clean client’s face as needed and monitor for complications.
- Document the procedure.
What to expect after NG tube removal
- Many clients feel relieved as soon as the NG tube is removed.
- Clients may experience mild throat irritation, increased mucus production, or hoarseness (should resolve quickly).
- Nausea can occur.
It is vital to closely observe the client after NG tube removal. Next to signs of respiratory distress or other complications, clients should be monitored for emotional reactions to their changed situation, or difficulties when gradually returning to oral nutrition intake.