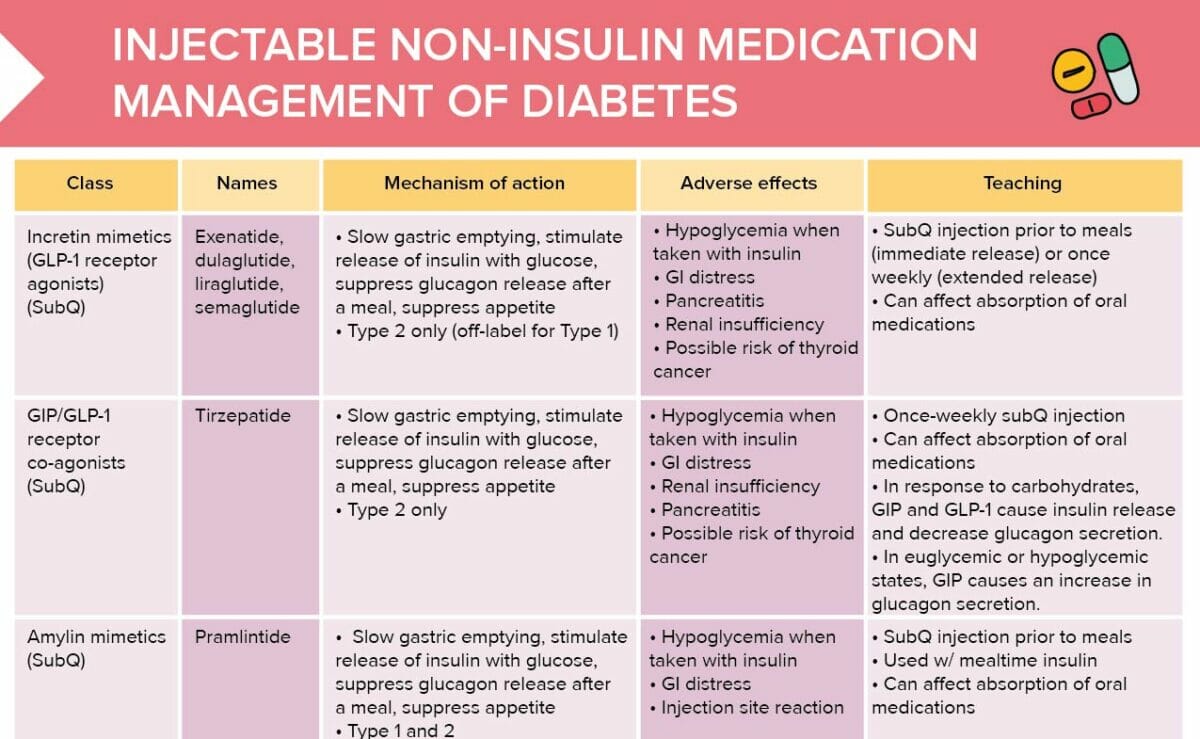
What are incretin mimetics?
Incretin mimetics, or GLP-1 receptor agonists, are a class of medications used to treat type 2 diabetes (off-label for type 1). They mimic the action of incretins, which are natural hormones in the body. Examples of incretin mimetics include liraglutide, exenatide, semaglutide, and dulaglutide.
Adverse effects of incretin mimetics
Potential adverse effects of incretin mimetics include:
- Hypoglycemia when taken with insulin
- GI distress
- Pancreatitis
- Renal insufficiency
- Possible risk of thyroid cancer
Other non-insulin, injectable diabetes medications
GIP/GLP-1 receptor co-agonists
GIP/GLP-1 receptor co-agonists are used to treat type 2 diabetes only. They can have adverse effects including:
- Hypoglycemia when taken with insulin
- GI distress
- Renal insufficiency
- Pancreatitis
- Possible risk of thyroid cancer
Amylin mimetics
Amylin mimetics are a group of medications used to treat type 1 and type 2 diabetes.
Potential adverse effects of these drugs include hypoglycemia (when taken with insulin), GI distress, and injection site reactions.
Mechanism of action
All non-insulin, injectable diabetes medications work by
- Slowing gastric emptying/decreasing gastric motility
- Stimulating the release of insulin with glucose
- Suppressing glucagon release after a meal
- Suppressing appetite/increasing satiety
Client education points
General teachings
- Do not inject into the same site as insulin.
- Immediate-release medications must be taken 60 minutes prior to a meal, not after.
- Educate clients how to use their specific device to avoid incorrect dosing.
- Do not double dose if missed.
- These medications may interfere with oral contraceptives.
- Educate the client on risks of hypoglycemia if using insulin.
Client teachings about incretin mimetics
- SubQ injection prior to meals (immediate release) or once weekly (extended release)
- Can affect absorption of oral medications
Client teachings about GIP/GLP-1 receptor co-agonists
- Once-weekly subQ injection
- Can affect absorption of oral medications
- In response to carbohydrates, GIP and GLP-1 cause insulin release and decrease glucagon secretion.
- In euglycemic or hypoglycemic states, GIP causes an increase in glucagon secretion.
Client teachings about amylin mimetics
- SubQ injection prior to meals
- Used w/ mealtime insulin
- Can affect absorption of oral medications