What does “hemodynamically stable” mean?
“Hemodynamically stable” means that the patient’s vital signs—like heart rate, blood pressure, and oxygen saturation—are within normal ranges. In a stable condition, the patient is generally at a lower immediate risk of life-threatening complications.
What does “hemodynamically unstable” mean?
“Hemodynamically unstable” indicates that vital signs are not within normal limits, and there’s a risk of inadequate blood flow to organs. This is a medical emergency requiring immediate intervention.
Why is hemodynamic stability important?
Hemodynamic stability is a requirement for any treatment plan, especially surgical procedures.
Stable vital signs—such as blood pressure, heart rate, and oxygen saturation—are generally a sign of adequate perfusion. When a patient is hemodynamically unstable, there’s a higher risk of inadequate perfusion leading to organ failure, tissue damage, and potentially life-threatening complications.
Arrhythmia vs dysrhythmia: what is the difference?
In many clinical settings, the terms “arrhythmia” and “dysrhythmia” are used interchangeably to describe irregularities in the heart rate or rhythm.
Both can involve deviations from normal sinus rhythm, such as tachycardia (fast heart rate), bradycardia (slow heart rate), or atrial fibrillation (irregular rhythm).
Some professionals use “dysrhythmia” as a term for any deviation from a normal rhythm, even if it’s not harmful, while using “arrhythmia” for clinically significant or harmful conditions.
Types of ventricular dysrhythmias
Ventricular tachycardia:
- Rapid heart beat arising from ectopic foci in the ventricles
- May occur with or without a pulse
Torsade de Pointes:
- A polymorphic form of ventricular tachycardia
- May occur with or without a pulse
Ventricular fibrillation:
- Irregular electrical activity originating from multiple sites within the ventricles
- The ventricles quiver instead of pumping blood.
- Client presents without a palpable pulse.
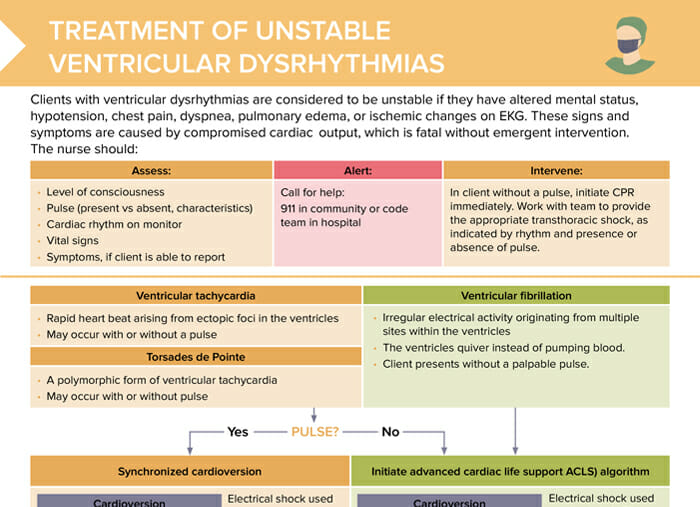
Treatment of unstable ventricular dysrhythmias
Clients with ventricular dysrhythmias are considered to be unstable if they have altered mental status, hypotension, chest pain, dyspnea, pulmonary edema, or ischemic changes on EKG. These signs and symptoms are caused by compromised cardiac output, which is fatal without emergent intervention.
The nurse should:
- Assess:
- Level of consciousness
- Pulse
- Cardiac rhythm on monitor
- Vital signs
- Symptoms, if client able to report
- Alert: Call for help (911 or code team).
- Intervene: In a client without a pulse, initiate CPR immediately. Work with team to provide the appropriate transthoracic shock, as indicated by rhythm and presence or absence of pulse.
Treatment steps
Does the client have a palpable pulse?
YES: synchronized cardioversion
- Electrical shock used to terminate a life-threatening cardiac rhythm in clients with a pulse
- Lower energy than defibrillation and shock is synchronized to occur on the R wave.
- May allow heart to resume normal sinus rhythm
NO: initiate ACLS algorithm
- Electrical shock used on clients in V-Fib or pulseless V-Tach
- Depolarizes cardiac cells, temporarily stopping all cardiac activity
- May allow the heart’s natural pacemaker to regain control and restart in normal sinus rhythm
Measures: defibrillate; epinephrine + amiodarone (if unresponsive to defibrillation after 3 shocks)
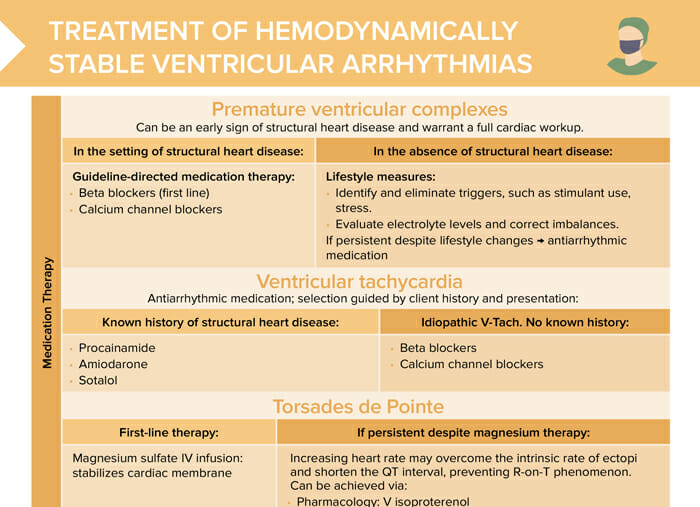
Treatment of hemodynamically stable ventricular arrhythmias
Premature ventricular complexes can be an early sign of structural heart disease and warrant a full cardiac workup.
Bonus download:
Treatment of hemodynamically stable ventricular arrhythmias
Treatment options for hemodynamically stable ventricular dysrhythmias
Pharmacological treatment
Depending on history:
- In the setting of structural heart disease: guideline-directed medication therapy (beta blockers, calcium channel blockers)
- In the absence of structural heart disease: lifestyle measures (identify/eliminate triggers, correct any electrolyte imbalances); antiarrhythmic medications
Ventricular tachycardia:
- If known history of structural heart disease: procainamide, amiodarone, sotalol
- If idiopathic: beta blockers, calcium channel blockers
Torsades de Pointes:
- First-line: magnesium sulfate IV infusion
- If persistent despite magnesium therapy: Increasing heart rate may overcome the intrinsic rate of ectopic and shorten the QT interval, preventing R-on-T phenomenon. Can be achieved via:
- Pharmacology: IV isoproterenol
- Electricity: override pacing
Procedural treatment
- Catheter ablation therapy:
- Uses heat or cold energy to create tiny scars in the heart tissue
- Can block faulty signals arising from these areas, which cause rapid and erratic heartbeat
- Implantable cardioverter-defibrillator:
- Device implantable in chest wall, monitors cardiac rhythm
- Can perform defibrillation, cardioversion or pacing as needed