What are ethics?
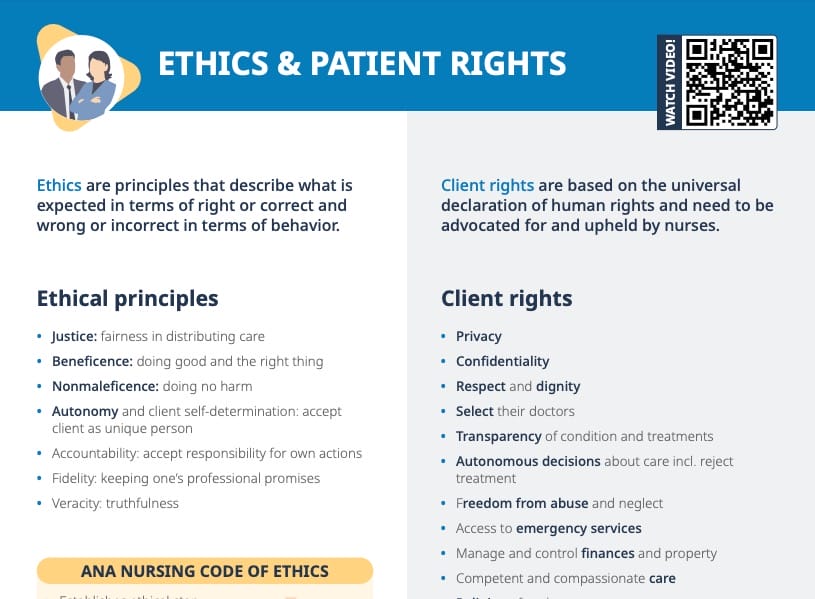
Ethics are principles that describe what is expected in terms of right or wrong in terms of behavior.
What is clinical ethics?
Clinical ethics is a subset of ethics that focuses on clinical medicine. It is essential to have an understanding of medical ethics in order to make clinical decisions.
Nurses must act on behalf of patients to promote and protect their rights and best interests, which includes speaking up and acting in favor of patient needs and what is ethically right.
Ethical principles in nursing
#1 Justice
Justice, or fairness, means nurses must be fair when they distribute care among their patients, and their attention and care must be equitably distributed.
#2 Beneficence
Beneficence means doing good and the right thing for the patient.
#3 Nonmaleficence
Nonmaleficence means doing no harm to the patients. This includes intentional as well as unintentional harm.
#4 Accountability
Accountability is accepting responsibility for one’s own actions. It means to accept the professional and personal consequences of your actions.
#5 Autonomy
Autonomy and patient self-determination mean to accept the patient as a unique person with an innate right to their own opinions and beliefs. Patients must be encouraged to make their own informed decisions without judgment or influence. This includes care aligning with a patient’s cultural beliefs and needs, as well as the patient’s right to refuse treatment.
#6 Fidelity
Fidelity stands for keeping one’s promises. A nurse must remain faithful and true to their professional responsibilities by providing high-quality, safe care.
#7 Veracity
Veracity means being truthful with patients at all times; including not withholding parts of the truth.
What are the 4 main ethical principles in nursing?
A lot of sources name as the 4 main principles:
- Autonomy
- Beneficence
- Nonmaleficence
- Justice
Ethical principles in organ donation
The Organ Procurement and Transplantation Network (OPTN) has defined the following major ethical principles to be applied in organ donation:
- Utility: goal is benefit of critically ill patients
- Justice: equitable access and equitable allocation of donated organs
- Respect: treating people as ends in themselves and not as some sort of means to an end
What is casuistry theory?
Casuistry theory is an ethical approach that focuses on case-based reasoning. Instead of applying broad ethical principles universally, casuistry examines individual situations and makes decisions based on the specifics of that case.
In nursing, this could mean evaluating a patient’s situation as a unique case and basing ethical decisions on the individual situation, rather than relying solely on broad ethical guidelines.
Potential ethical dilemmas in nursing
Situations that can lead to ethical dilemmas in nursing practice include:
- Staffing ratios
- Disagreements between patients and healthcare providers
- Disagreements between healthcare providers
- Limited resources
- End-of-life issues
- Waiting lists
- Medical errors
- Informed-consent issues
- Bioethics (stem cells, cloning, genetic engineering)
How to solve an ethical dilemma
As nurses, it is our obligation to recognize and identify ethical issues that affect staff and patients. Ethical committees within facilities can advise in the resolution of ethical concerns.
- Identify a concern: What is wrong?
- Identify the dilemma: What are the competing obligations? What values are at stake?
- Identify the stakeholders: Who is affected by this situation, decision, or action? Consider medical indications, patient preferences, quality of life, and context.
- Identify sources of guidance: (e.g., case law, code of ethics)
- Explore possible solutions
- Decide on a course of action
- Evaluate outcome
What is an ethical committee?
An ethics committee is a multidisciplinary group within a healthcare facility that provides guidance on ethical dilemmas and complex patient-care issues. A nurse might consult an ethics committee when faced with a challenging ethical decision where guidance, additional perspectives, or institutional input is needed.
What is moral distress in nursing?
Moral distress occurs when a nurse knows the ethically appropriate action to take but feels constrained or powerless to take that action, often leading to feelings of frustration, guilt, or anguish. It can arise from internal conflicts, organizational constraints, or conflicting duties and responsibilities.