What are corticosteroids?
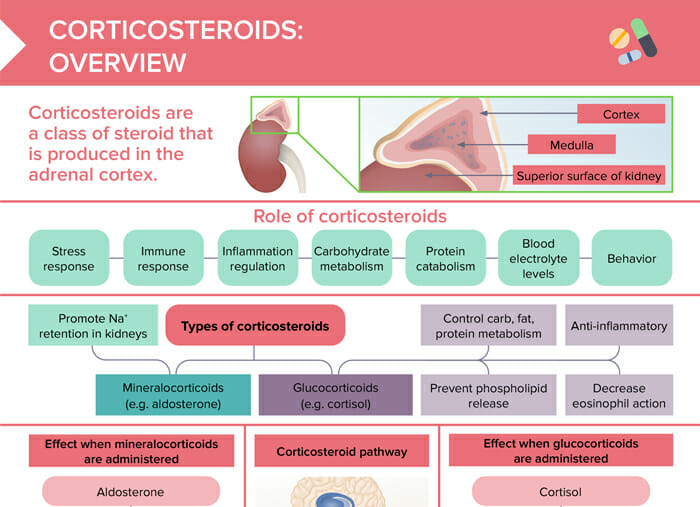
Corticosteroids are a class of steroids that are produced in the adrenal cortex. As a medication, corticosteroids mimic the hormone function and are used to treat a variety of conditions such as asthma, arthritis, allergies, lupus, multiple sclerosis, and certain skin conditions.
Related videos
What are the types of corticosteroids?
The two types of corticosteroids are mineralocorticoids (e.g., aldosterone, fludrocortisone) and glucocorticoids (e.g., cortisol, prednisone).
Mineralocorticoids
Mineralocorticoids impact electrolyte and water levels (impacting blood pressure). They are used to treat conditions such as Addison disease, where there is a deficiency of these hormones.
Glucocorticoids
Glucocorticoids are primarily used to manage conditions, such as asthma, arthritis, and autoimmune diseases. Their properties are:
- Anti-inflammatory and immunosuppressive effects
- Control carbohydrate, fat, protein metabolism
- Prevent phospholipid release
- Decrease eosinophil action
Effects of mineralocorticoids
Mineralocorticoids, such as fludrocortisone, primarily affect the body’s balance of sodium and water, leading to increased blood volume and blood pressure. They are often used to treat conditions like Addison disease for adrenal insufficiency.
However, they can also have side effects such as fluid retention, high blood pressure, heart failure, hypokalemia (low potassium levels), and in rare cases, it can lead to adrenal crisis if stopped suddenly. Therefore, they should be used carefully, monitored regularly, and never abruptly discontinued.
Aldosterone → Sodium/water retention, potassium excretion → Increased blood volume → Higher blood pressure
Effects of glucocorticoids
Glucocorticoids, such as prednisone, have anti-inflammatory and immunosuppressive effects. They are used for conditions such as asthma, allergies, autoimmune diseases, and inflammatory conditions.
However, their side effects can include increased blood glucose levels, weight gain, mood changes, insomnia, osteoporosis with long-term use, and increased susceptibility to infections due to suppressed immune response. Like mineralocorticoids, discontinuing glucocorticoids abruptly can lead to adrenal crisis, so should be tapered off under the direction of a healthcare provider.
Cortisol →
- Affects carbohydrate, fat, protein metabolism
- Anti-inflammatory
- Lowered eosinophil action
- Affects glucose metabolism
- Affects mood, behavior
- Higher bone reabsorption
What is the corticosteroid pathway?
The corticosteroid pathway, or the hypothalamic-pituitary-adrenal (HPA) axis, is the body’s major stress response system. Here’s how it works:
- Hypothalamus releases corticotropin-releasing hormone (CRH).
- Pituitary gland secretes adrenocorticotropic hormone (ACTH).
- ACTH stimulates the adrenal glands to produce and release corticosteroids (cortisol/aldosterone).
What is the therapeutic goal of corticosteroid treatment?
The therapeutic goal of corticosteroid treatment is to have an anti-inflammatory effect and decrease immune reaction. They also can be used to replace hormones in adrenal insufficiency.
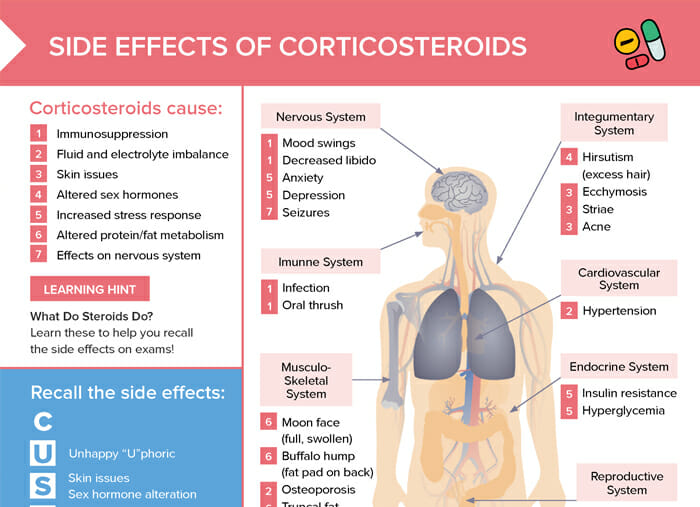
What is the role of corticosteroids in the body?
- Stress response
- Immune response
- Inflammation regulation
- Carbohydrate metabolism
- Protein metabolism
- Blood electrolyte levels
- Chemical changes
These functions are essential for maintaining homeostasis in the body. When corticosteroid levels are too high or too low, it can lead to health problems.
How do corticosteroids interact with other medications?
Corticosteroids can interact with many other medications, altering their effects. For example, they can increase the blood glucose in clients with diabetes or increase the risk of gastrointestinal bleeding with NSAIDs. Always check for potential interactions in your client’s medication plans.
What are signs of corticosteroid overdose?
Signs can include hyperglycemia, hypertension, fluid retention, insomnia, and mood changes. In severe cases, corticosteroid overdose can cause Cushing syndrome.
Client education regarding corticosteroids
Instruct clients to:
- Take medication as prescribed
- Report adverse effects
- Not stop taking the medication abruptly
- Monitor signs of side effects (e.g., weight gain, mood changes, increased thirst or hunger, signs of infection)
- Stick to regular follow-ups (for long-term users)