A 62-year-old man with a past medical history of previous myocardial infarction, angina, hypertension, hyperlipidemia, diabetes mellitus, peripheral vascular disease, and a below-knee amputation has developed new chest pain. His medication includes insulin, hydrochlorothiazide, lisinopril, metoprolol, daily aspirin, atorvastatin, and nitroglycerin as needed. His blood pressure is 135/87 mm Hg, pulse 52/min, and his respirations are 17/min. Coronary arteriography shows a reduced ejection fraction, 65% stenosis of the left anterior descending artery, and 75% stenosis of the left circumflex artery. Which of the following is the recommended treatment for the patient?
A. Coronary artery bypass grafting (CABG)
B. Heparin
C. Increased beta blocker dosage
D. Extended release nitrate therapy
E. Angioplasty with stent placement
A 66-year-old female with hypertension and a recent history of acute ST-segment elevation myocardial infarction (STEMI) six days earlier, treated with percutaneous transluminal angioplasty (PTA), presents with sudden onset chest pain, shortness of breath, diaphoresis, and syncope. The patient’s temperature is 37℃ (98.6℉), blood pressure is 80/50 mm Hg, pulse is 125/min, respiratory rate is 12/min, and oxygen saturation is 92% on room air. On physical examination, the patient is pale and unresponsive. A cardiac exam reveals tachycardia and a pronounced holosystolic murmur loudest at the apex and radiates to the back. Lungs are clear to auscultation. Her chest X-ray shows cardiomegaly with clear lung fields. ECG is significant for ST elevations in the precordial leads (V2-V4) and low-voltage QRS complexes. An emergency transthoracic echocardiography shows a left ventricular wall motion abnormality along with a significant pericardial effusion. The patient is intubated, and aggressive fluid resuscitation is initiated. What is the next best step in management?
A. Intra-aortic balloon counterpulsation
B. Administer dobutamine 70 mcg/min IV
C. Emergency pericardiocentesis
D. Immediate transfer to the operating room
E. Immediate cardiac catheterization
A 3-year-old boy is brought to his pediatrician for a regular checkup by his mother. The patient’s mother is concerned about a slight deviation of his left eye and she also notes that her child’s left eye looks strange on the photos, especially if there is a flash. The patient is the first child in the family born to a 31-year-old woman. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. Family history is unremarkable. The eye examination shows left eye converging strabismus. The pupillary reflex cannot be elicited from an illumination of the left eye. Fundal examination reveals are shown in the picture. On testing, visual evoked potential cannot be elicited from the left retina but is normal from the right retina. MRI of the orbits shows a retina-derived tumor in the left eye with an initial spread along the intrabulbar part of the optic nerve and vitreous seeding. The other eye is completely intact. Which of the following methods of treatment is indicated for this patient?
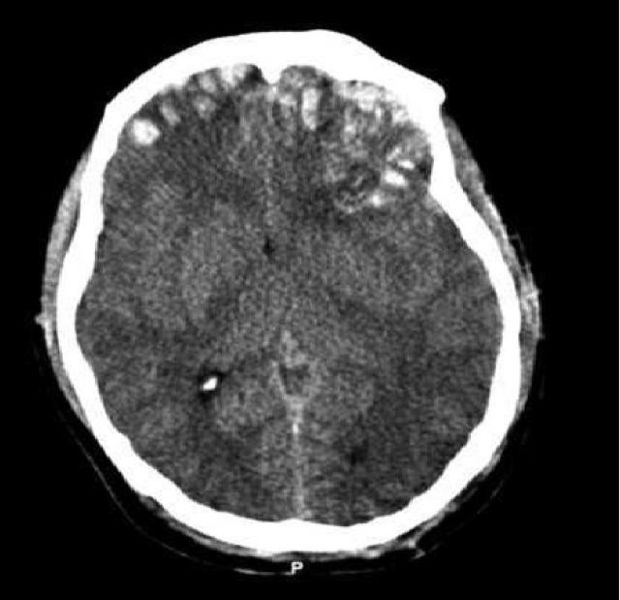
A 31-year-old unresponsive man is admitted to the emergency department after a single-vehicle roll-over accident. On primary assessment by paramedics, he was unresponsive. On admission, he opened his eyes to painful stimuli, was not responsive to verbal commands, his arms were flexed and the legs were straight with no reaction to pain. The patient was intubated and examined. His blood pressure is 150/90 mm Hg, heart rate is 56/min, respiratory rate is 14/min, temperature is 37.5℃ (99.5℉), and SpO2 is 94% on room air. The examination shows a depressed fracture of the left temporal bone and ecchymoses and scratches over his abdomen and extremities. His pupils are round, equal, and show a poor response to light. There is no disconjugate eye deviation. His lungs are clear to auscultation and the heart sounds are normal. Abdominal examination reveals normal bowel sounds and no fluid wave. There are no meningeal signs. Focused assessment with sonography for trauma is negative for blood in the abdominal cavity. Head CT scan is shown in the picture. Which procedure is required to guide further management?
A 60-year-old man presents with pain, swelling, and a purulent discharge from his left foot. He says that the symptoms began 7 days ago with mild pain and swelling on the medial side of his left foot, but have progressively worsened. He states that there has been a foul-smelling discharge for the past 2 days. The medical history is significant for type 2 diabetes mellitus that was diagnosed 10 years ago and is poorly managed, and refractory peripheral artery disease that failed revascularization 6 months ago. The current medications include aspirin (81 mg orally daily) and metformin (500 mg orally twice daily). He has a 20-pack-year smoking history but quit 6 months ago. The family history is significant for type 2 diabetes mellitus in both parents and his father died of a myocardial infarction at 50 years of age. His temperature is 38.9°C (102°F), blood pressure is 90/65 mm Hg, pulse is 102/min, respiratory rate is 22/min, and oxygen saturation is 99% on room air. On physical examination, he appears ill and diaphoretic. The skin is flushed and moist. There is 2+ pitting edema of the left foot with blistering and black discoloration (see picture). The lower legs are hairless and the lower extremity peripheral pulses are 1+ bilaterally. Laboratory tests are pending. Blood cultures are positive for Staphylococcus aureus. Which of the following findings is the strongest indication for amputation of the left lower extremity in this patient?
A. Diminished peripheral pulses
B. Positive blood cultures
C. Presence of wet gangrene
D. Smoking history
E. Poorly managed blood glucose

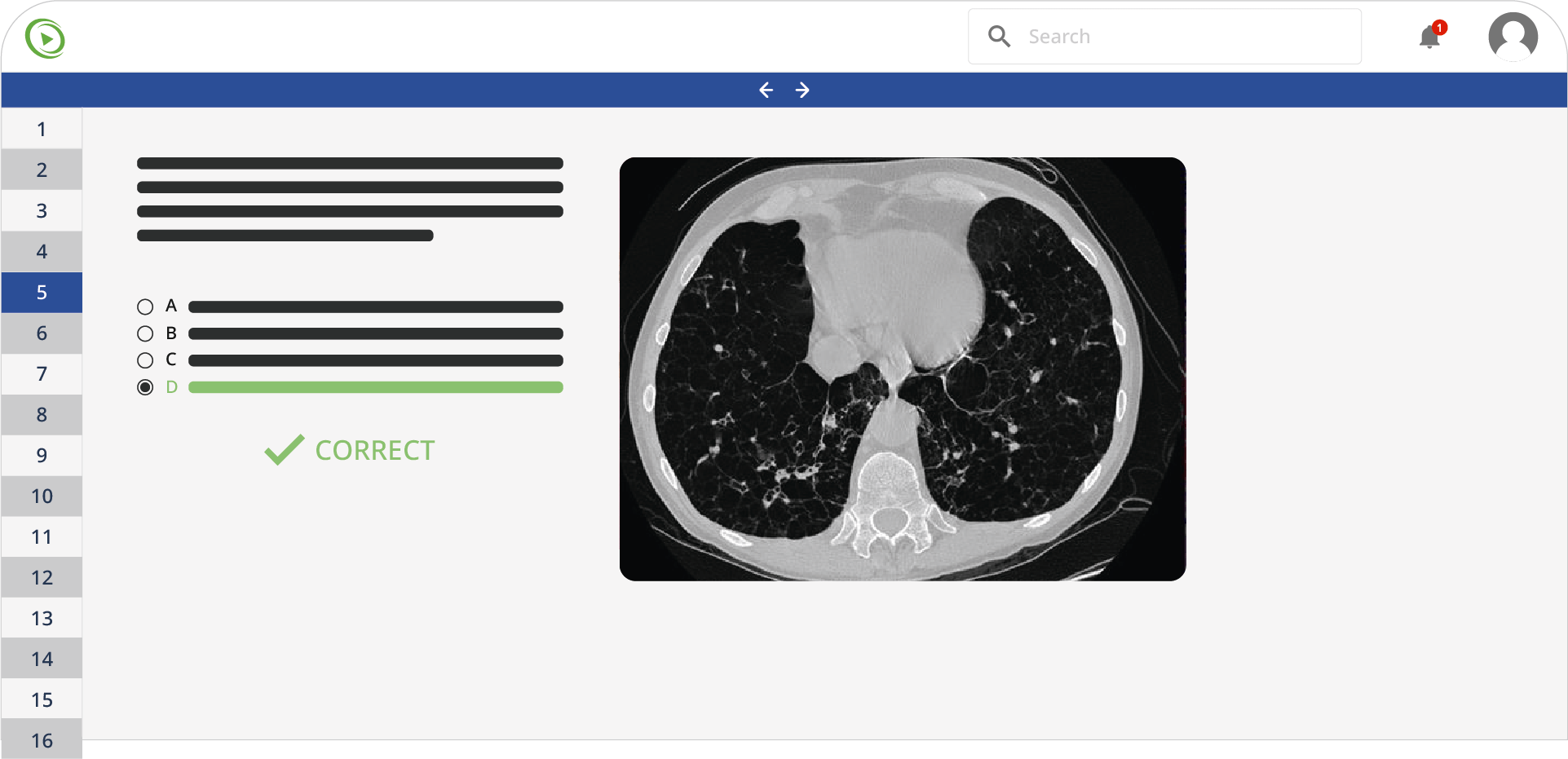
A 27-year-old man presents to the emergency department with severe dyspnea and sharp chest pain that suddenly started an hour ago after he finished exercising. He has a history of asthma as a child, and he achieves good control of his acute attacks with Ventolin. On examination, his right lung field is hyper-resonant along with diminished lung sounds. Chest wall motion during respiration is asymmetric. His blood pressure is 105/67 mm Hg, respirations are 22/min, pulse is 78/min, and temperature is 36.7°C (98.0°F). The patient is supported with oxygen, given corticosteroids, and has had analgesic medications via a nebulizer. Considering the likely condition affecting this patient, what is the best step in management?
A. Chest X-rays
B. ABG
C. Tube insertion
D. Sonogram
E. CT scan
A 6-year-old boy is brought to the pediatrician by his parents. He has been coughing extensively over the last 5 days, especially during the night. His mother is worried that he may have developed asthma, like his uncle, because he has been wheezing, too. The boy usually plays without supervision, and he likes to explore. He has choked a few times in the past. He was born at 38 weeks of gestation via a normal vaginal delivery. He has no known allergies. Considering the likely etiology, what is the best approach to manage the condition of this child?
A. Order a CT scan
B. Prescribe montelukast
C. Perform cricothyroidotomy
D. Perform bronchoscopy
E. Encourage the use of a salbutamol inhaler
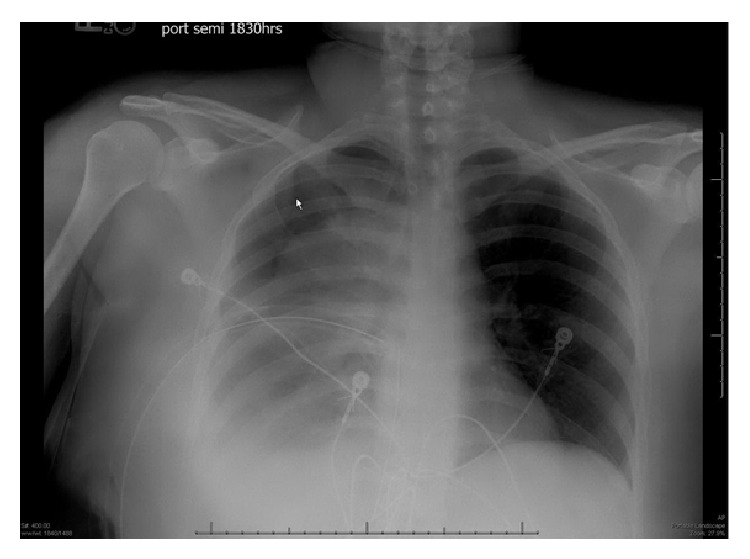
A 45-year-old man in respiratory distress presents to the emergency department. He sustained a stab to his right chest and was escorted to the nearest hospital. The patient appears pale and has moderate difficulty with breathing. His O2 saturation is 94%. The right lung is dull to percussion. CXRs are ordered and confirm the likely diagnosis. His blood pressure is 95/57 mm Hg, the respirations are 22/min, the pulse is 87/min, and the temperature is 36.7°C (98.0°F). His chest X-ray is shown. Which of the following is the next best step in management for this patient?
A 56-year-old man presents to his primary care provider because of a lack of flexibility in his right hand. He has noticed that his hand has become less flexible and more fixed over the past year and he now has trouble shaking other people’s hands comfortably. He has a history of chronic alcohol abuse, hepatitis C, and cirrhosis. His family history is insignificant. He has a 40 pack-year smoking history. At the physician’s office, his blood pressure is 118/67 mm Hg, the respirations are 18/min, the pulse is 77/min, and the temperature is 36.7°C (98.0°F). On physical examination, the 4th and 5th digits are mildly flexed with dense, rope-like cords extending down his palm. Additionally, small ulcerations are identified on his palm. Which of the following is considered the first-line therapy for this condition?
A. Surgery
B. Colchicine
C. Anti-TNF drugs
D. Steroid injections
E. Collagenase injections
A 53-year-old woman is referred to the physical medicine and rehabilitation center for pain in her right knee. She has felt an increasingly mild pain in her right knee after her morning walks for the past 5 months. She has no other medical comorbidities. Her family history is significant for degenerative joint diseases. Vital signs are normal. On physical examination, there is evidence of crepitations in her right knee joint. Passive movements of the knee joint are mildly limited. No joint malalignment is observed. The patient is scheduled for arthroscopic debridement and is prescribed a therapeutic exercise regimen. Which of the following is the most commonly associated complication of this procedure?
A. Effusions
B. Synovitis
C. Septic arthritis
D. Deep vein thrombosis
E. Post-procedure shock
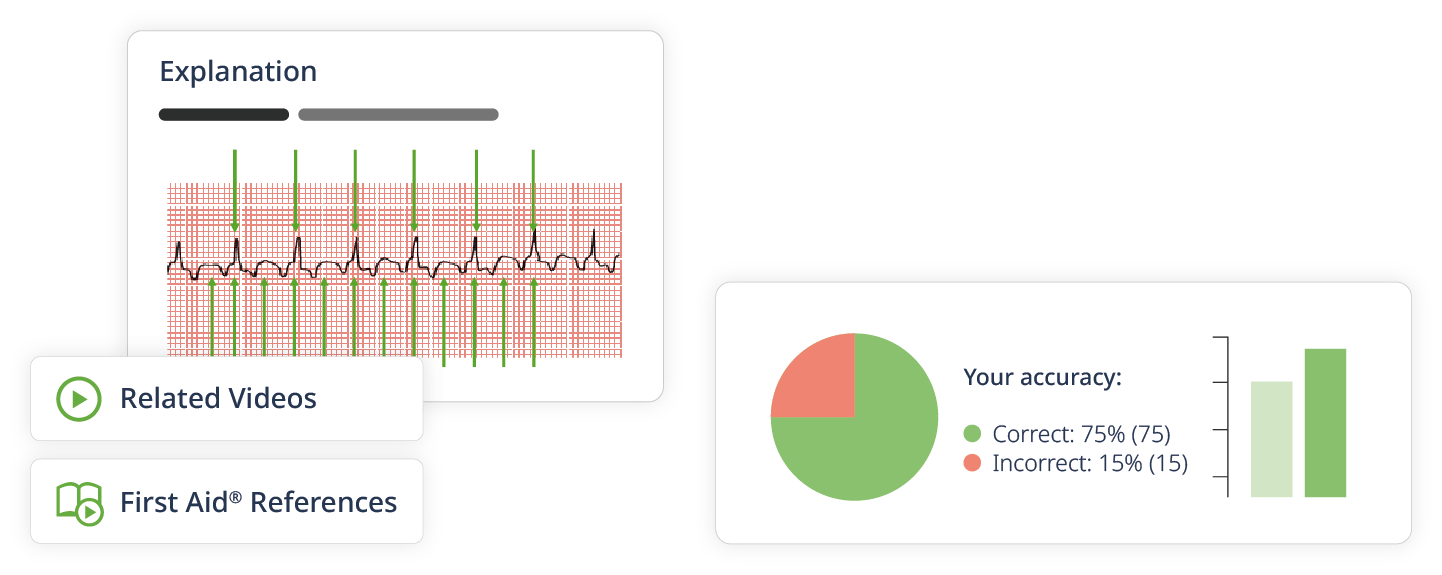
Do you want to practice more Surgery questions?
Create a free Lecturio account and you’ll have access to the Lecturio question bank with more than 1,200 USMLE Step 2 CK practice questions.