Nursing Knowledge
An individual’s blood type (the molecules on the surface of red blood cells) is determined by the presence or absence of A or B antigens and the Rhesus (Rh) factor. When Rh factor proteins are present on the red blood cells, the individual is Rh-positive, while Rh-negative individuals have no Rh factor proteins.
The discovery of the Rh factor had significant and far-reaching impacts on society, particularly in the fields of medicine and public health, for example:
Rh incompatibility is the discordant pairing of a pregnant person with Rh-negative blood type and a Rh-positive fetus.
This difference in Rh status can lead to complications due to the mother’s immune system reacting against the Rh factor, a protein on the surface of the baby’s red blood cells.
Fetomaternal hemorrhage is when fetal blood enters the pregnant client’s blood stream due to a breach of the placental membrane, such as:
Rh alloimmunization, also known as Rh sensitization, occurs when a person with Rh-negative blood is exposed to Rh-positive blood and develops an immune response to the Rh factor, a protein on the surface of red blood cells.
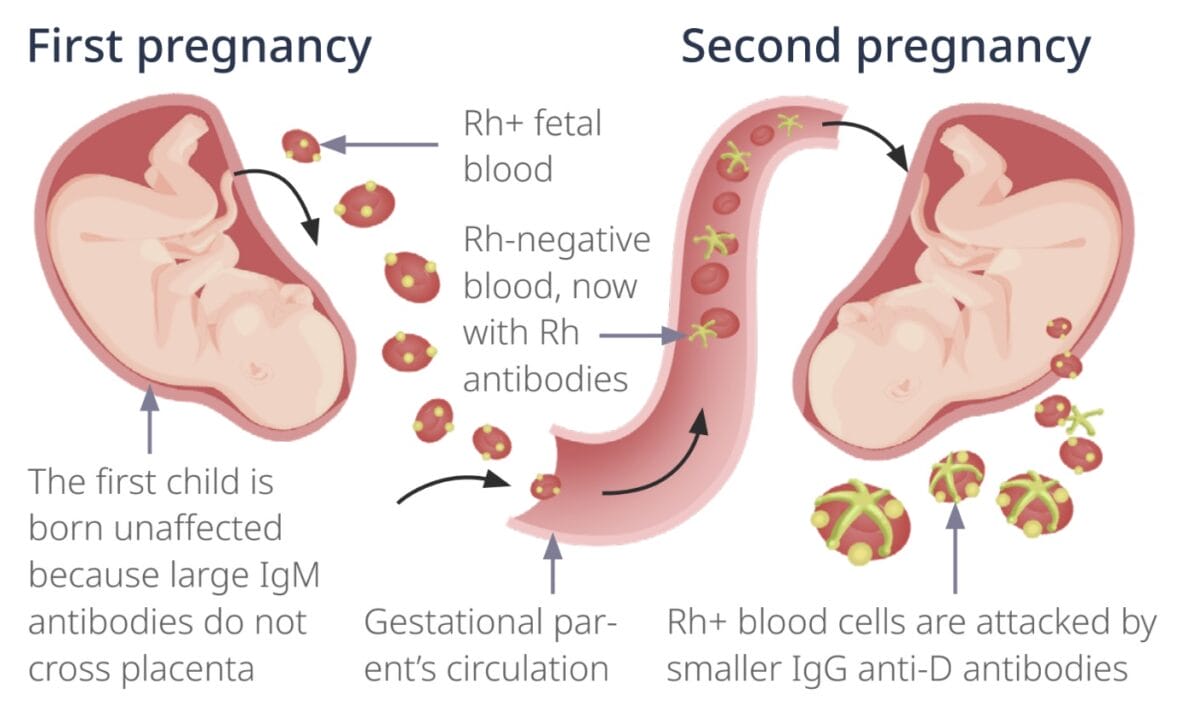
If an Rh-negative person carries an Rh-positive fetus, they can become sensitized if fetal blood cells cross into their circulation, usually during childbirth, miscarriage, abortion, or some medical procedures. Once exposed to Rh-positive blood, the immune system may produce antibodies against the Rh factor (anti-D antibodies).
In a potential subsequent pregnancy with another Rh-positive baby, when fetomaternal hemorrhage occurs, the Rh D antigen on fetal blood cells is perceived as a threat and prompts the pregnant client’s immune system to produce anti-D antibodies. These antibodies can cross the placenta and attack the fetus’s red blood cells, leading to hemolytic disease of the newborn.
The fetus triggering alloimmunization is protected from large IgM antibodies by the placenta and remains unaffected. But, if the sensitized client has another Rh+ fetus in a subsequent pregnancy, fetal red blood cells are targeted by IgG antibodies, causing hemolytic disease of the neonate.
Subsequent pregnancies with Rh-positive babies are typically more dangerous since the immune response gets stronger with the mother’s immune system already being primed and reacting more robustly and rapidly, producing more antibodies.
Hemolytic disease of the neonate (HDN) is a consequence of Rh incompatibility because the mother’s immune system produces antibodies against the baby’s red blood cells.
Symptoms of HDN range from mild to severe, including:
It is typically diagnosed through prenatal screening and blood tests, including antibody titers and blood type testing.
Alloimmunization in the context of Rh incompatibility is primarily prevented using RhD immunoglobulin (RhIg).
RhD immunoglobulin (RhIg) mimics the body’s innate antibodies. If the pregnant client is exposed to Rh-positive fetal blood, their body does not react as it perceives that the needed antibodies are already present. This prevents alloimmunization.
RhIg is routinely administered via IM injection:
This intervention significantly reduces the risk of Rh alloimmunization in future pregnancies.
ABO incompatibility and Rh incompatibility are the types of blood group incompatibilities that can occur between a pregnant patient and the fetus, leading to hemolytic disease of the newborn.
RELATED TOPIC:
Free Download
Master the topic with a unique study combination of a concise summary paired with video lectures.
Your free account gives you access to:
or