Nursing Knowledge
Electronic fetal monitoring is the use of instruments to monitor fetal heart rate and uterine contractions to assess fetal health and response to the intrauterine environment.
The types of electronic fetal monitoring are:
External monitoring:
Internal monitoring:
| Type of monitoring | Pros | Cons |
| External; continuous auscultation | Allows continuous visual depiction of fetal heart rate (FHR)and uterine contractions (required when certain medications are given) | Restricts maternal movement (belts can be uncomfortable); can be affected by movement and body habitus; displays contraction frequency but not strength |
| External; intermittent auscultation | Allows freedom of maternal movement and can be used underwater and in multiple positions | Usually only for low-risk mothers; not for use with epidurals or labor-stimulating medications; does not assess contractions |
| Internal (continuous auscultation) | Most accurate! Provides continuous visual depiction of FHR and uterine contractions; only method that can objectively assess contraction strength; unaffected by maternal habitus/movement; can be used to provide amnioinfusion | Placed by provider; requires cervix to be dilated and ruptured membranes; increases risk of infection; possibility of injury; contraindicated with some maternal conditions/infections; restricts maternal movements |
The components of fetal monitoring assessment include:
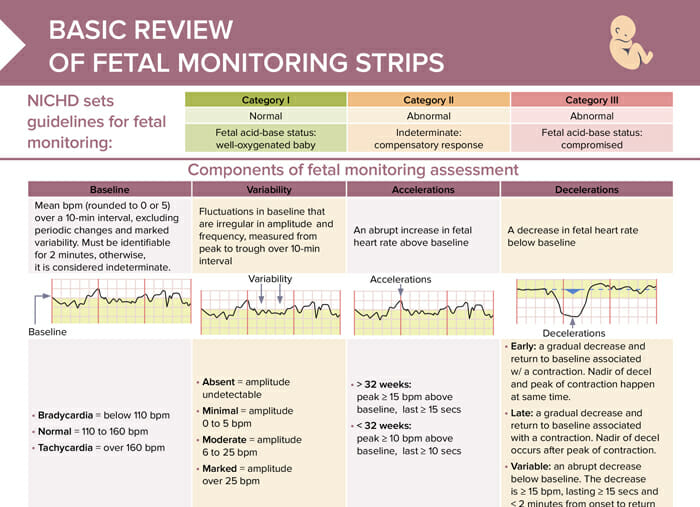
The National Institute of Child Health and Human Development (NICHD) has developed a three-tiered system for the interpretation of FHR patterns through electronic fetal monitoring:
| Category I | Category II | Category III |
| Normal | Abnormal | Abnormal |
| Fetal acid-base status: well-oxygenated baby | Indeterminate: compensatory response | Fetal acid-base status: compromised |
The baseline fetal heart rate is the average FHR during a 10-minute window, excluding periods of marked variability, decelerations, and tachycardia.
Variability refers to the fluctuations in the baseline FHR. Moderate variability (6 to 25 beats per minute) is usually a reassuring sign, indicating a well-oxygenated fetus with a functioning autonomic nervous system. Minimal or absent variability can be concerning and may suggest hypoxia or acidemia, but can also be seen in a sleeping fetus or with certain medications.
Accelerations are temporary increases in the FHR of at least 15 beats per minute, lasting for at least 15 seconds. They’re generally a reassuring sign, indicating a well-oxygenated fetus responding to movement or stimulation.
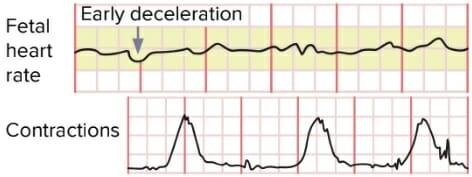
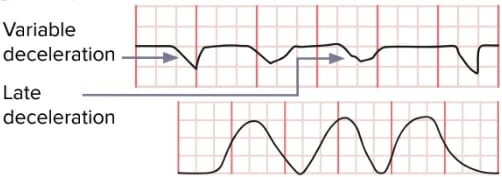
Early decelerations are dips in FHR that coincide with contractions, usually due to head compression and are generally not concerning. Late decelerations are dips in FHR that occur after the peak of a contraction and may indicate placental insufficiency, necessitating close monitoring or intervention. Variable decelerations are abrupt drops in FHR due to umbilical cord compression. Depending on their frequency, depth, and duration, they may require intervention.
Overview of fetal monitoring strip assessment, review of category 1–3 strips, and basic interventions
Variable and late decelerations require immediate intervention:
The first nursing intervention for an abnormal fetal heart tracing is to reposition the client to their left side to maximize blood flow and oxygen to the fetus.
RELATED TOPIC:
FREE CHEAT SHEET
Free Download
Master the topic with a unique study combination of a concise summary paired with video lectures.
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
Your free account gives you access to:
or
Have a holly, jolly study session 🎁 Save 50% on all plans now >>