its hard to follow him, due to his disorganization
By birehan e. on 21. March 2024 for Pneumothorax, Pleural Effusion & Obstructive Sleep Apnea
it's hard to follow him due to his disorganization. he jumps here and there, that makes it hard to follow
MY ASSESSMENT
By michael o. on 01. February 2023 for Disorders of the Pulmonary Circulation and the Respiratory Regulation
The videos are of short duration. The videos need to be longer, and some videos that I search for are not on file to be watched.
Good job by Doctor Raj------I wish I know as much pathology as him!!!!!!
Good
By deleted u. on 27. July 2022 for Disorders of the Pulmonary Circulation and the Respiratory Regulation
I like the way Dr Raj explains everything with accuracy and with so much dedication.
DR.CARLO RAJ THEEEEEEEE BESSSST
By Vishnu K. on 14. May 2021 for Neonatal Respiratory Distress Syndrome: TTN, RDS and PPHN
DR.CARLO RAJ MAKES CONCEPTS EASIER THROUGH HIS ACTION AND WAY OF TEACHING
An excellent lecture
By Luis Ángel Z. on 12. May 2021 for Acute Respiratory Distress Syndrome (ARDS): Pathogenesis
Dr. Carlo Raj, i like a lot the way you expose the lectures. You explain everything in very understandable way
Best explanation
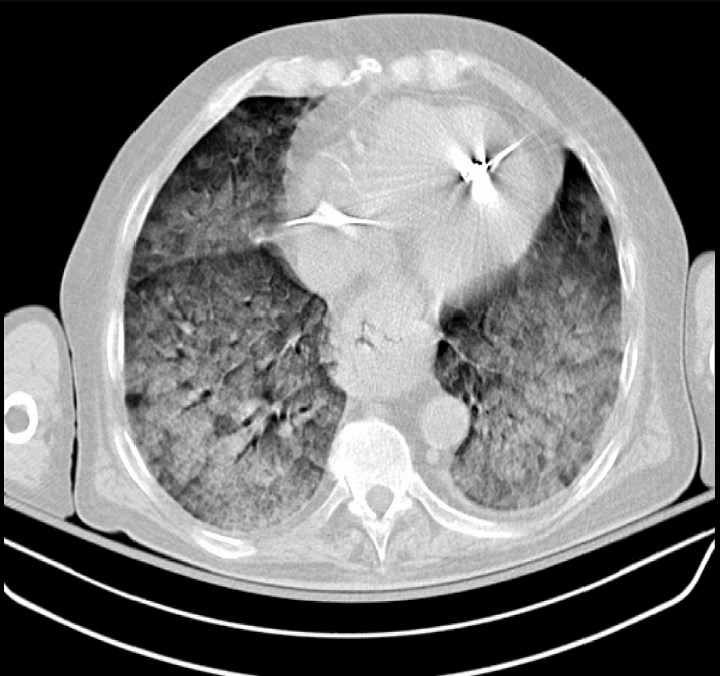
By BIHARA R. on 26. December 2020 for Acute Respiratory Distress Syndrome (ARDS): Signs, Symptoms, Definition, Treatment
He explains it well without any stress just like a pro
Superb explanation
By Rajath R. on 25. May 2020 for Acute Respiratory Distress Syndrome (ARDS): Pathogenesis
Thank u so much Dr Raj. It was a very good lecture.
Amazing teacher
By Saradha P. on 06. January 2020 for Disorders of the Pulmonary Circulation and the Respiratory Regulation
Dr Raj is just amazing , he simplifies the concept and makes it funny
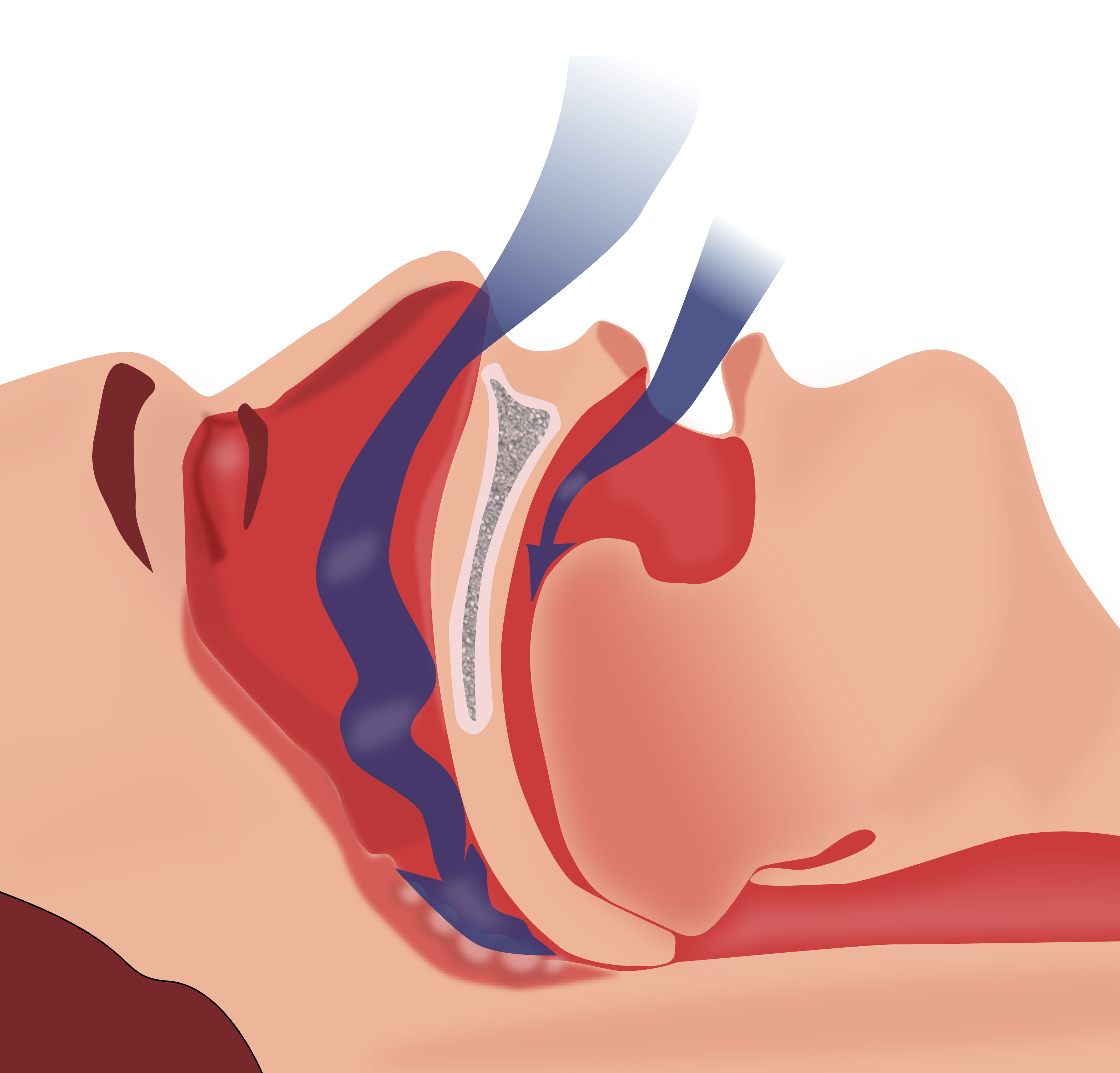
Sleep apnea
By La melma C. on 09. July 2019 for Sleep Apnea: Definition
Holy moly, you are awesome. I understood the topic ASSAP. I love the way you explain, keep up the good job
Great!
By olawale o. on 05. February 2018 for Acute Respiratory Distress Syndrome (ARDS): Differential Diagnosis
Once again, Dr. Raj is blowing my mind with the way he teach medicine. Connecting everything from here on out to eternity. I have a question about that second quiz question about sepsis before ARDS. The answer was that ARDS following sepsis will decrease the cardiac output, and that was according to what Dr. Raj said in the lectures. Is it possible that we could also have a situation with respiratory rate increasing?