A síndrome do ovário poliquístico (SOP) é a patologia endócrina mais comum nas mulheres em idade reprodutiva, afetando cerca de 5% a 10% das mulheres nesta faixa etária. Tendo em conta que se caracteriza por hiperandrogenismo, anovulação crónica associada a oligomenorreia (ou amenorreia) e disfunção metabólica, a SOP aumenta o risco de infertilidade, hiperplasia ou carcinoma endometrial e de doenças cardiovasculares. A fisiopatologia não é totalmente compreendida, mas acredita-se que tenha uma base genética multifatorial com alteração na liberatção pulsátil da hormona libertadora de gonadotrofinas (GnRH, pela sigla em inglês), bem como aumento da hormona luteinizante (LH, pela sigla em inglês), androgénios, estrogénio e insulina: o que resulta em anovulação crónica e hirsutismo, definidores desta patologia. O diagnóstico é de exclusão; portanto, devem ser descartadas outras causas de hemorragia uterina anormal e hirsutismo. O tratamento inclui a tentativa de restauração da ovulação normal através da perda de peso, pílulas anticoncecionais orais (ACOs) e assistência à fertilidade.
Última atualização: Feb 9, 2023
Os mecanismos exatos são desconhecidos, mas considerados complexos e incluem fatores genéticos e ambientais. A síndrome metabólica e a obesidade estão frequentemente, mas nem sempre, presentes e provavelmente contribuem para a fisiopatologia em alguns indivíduos.
A síndrome do ovário policístico (SOP) deve ser suspeitada em qualquer mulher em idade reprodutiva com menstruação irregular e/ou sintomas de hiperandrogenismo, especialmente se obesa ou apresentando infertilidade.

Hirsutism in PCOS:
Hair is noted along the side burns, chin, and upper lip; signs of hyperandrogenism.

Male-pattern alopecia in PCOS:
The patient has frontal hair thinning, which is a sign of hyperandrogenism.

Acantose nigricans na SOP:
A pele espessada e escurecida pode aparecer na nuca, axilas ou dobras cutâneas como um sinal de altos níveis de insulina devido à resistência à insulina.
A síndrome do ovário policístico (SOP) é um diagnóstico de exclusão, portanto, outras causas de oligo ou amenorreia e hiperandrogenismo devem ser descartadas. Os critérios de Rotterdam são comumente usados para fazer o diagnóstico, uma vez que outras causas são excluídas.
O diagnóstico requer 2 dos 3 critérios a seguir:
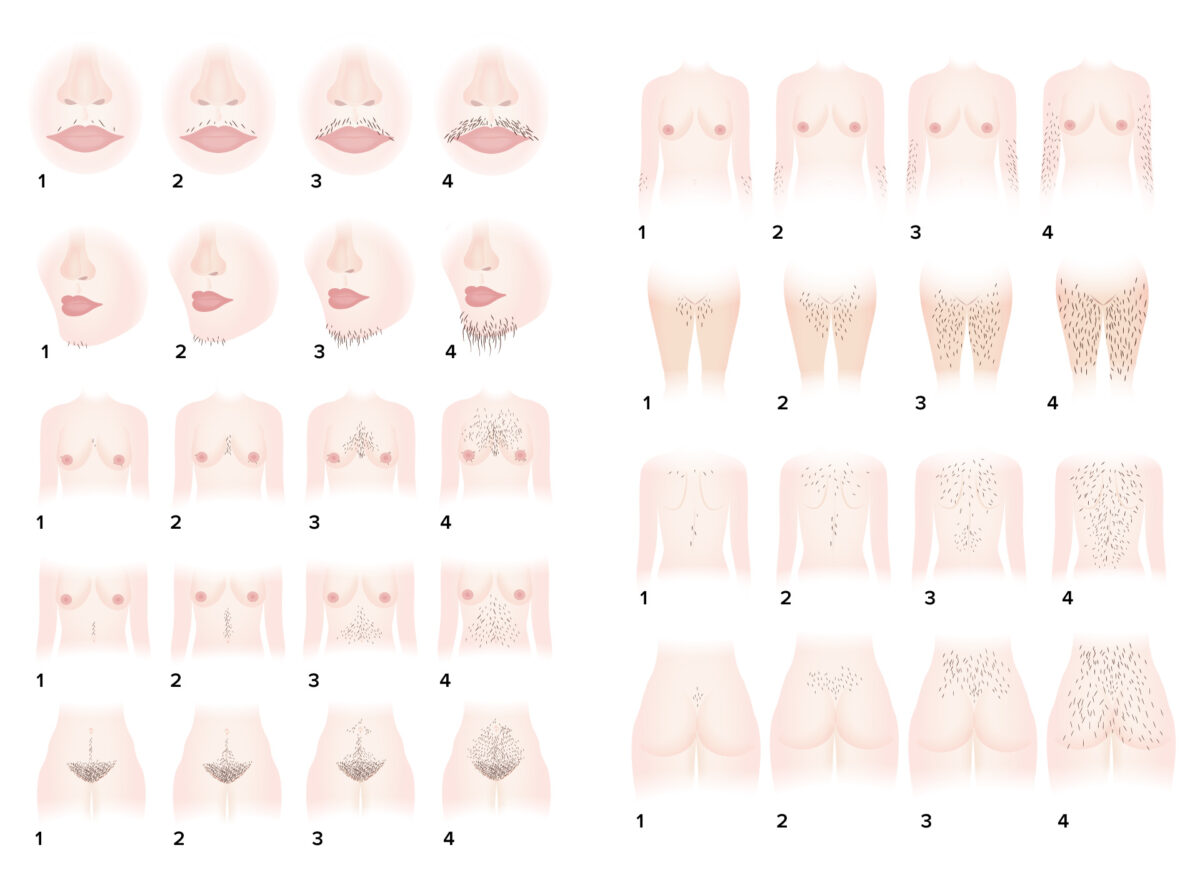
Sistema de pontuação de hirsutismo de Ferriman-Gallwey: um sistema para avaliação objetiva do grau de hirsutismo
Imagem por Lecturio.| Hormones ↑ in PCOS | Hormones ↓ in PCOS |
|---|---|
|
|
FSH: follicle-stimulating hormone
HDL: high-density lipoproteins
LDL: low-density lipoproteins
LH: luteinizing hormone
PCOS: polycystic ovarian syndrome
SHBG: sex hormone-binding globulin

Ultrassonografia de um ovário de aparência policística:
Observe as clássicas “pérolas em uma corda” ao redor da periferia do ovário, identificando os folículos em desenvolvimento anormal vistos na SOP. Ovários com aparência policística são vistos em aproximadamente ⅔ dos pacientes com SOP e é 1 dos 3 critérios diagnósticos de Rotterdam.
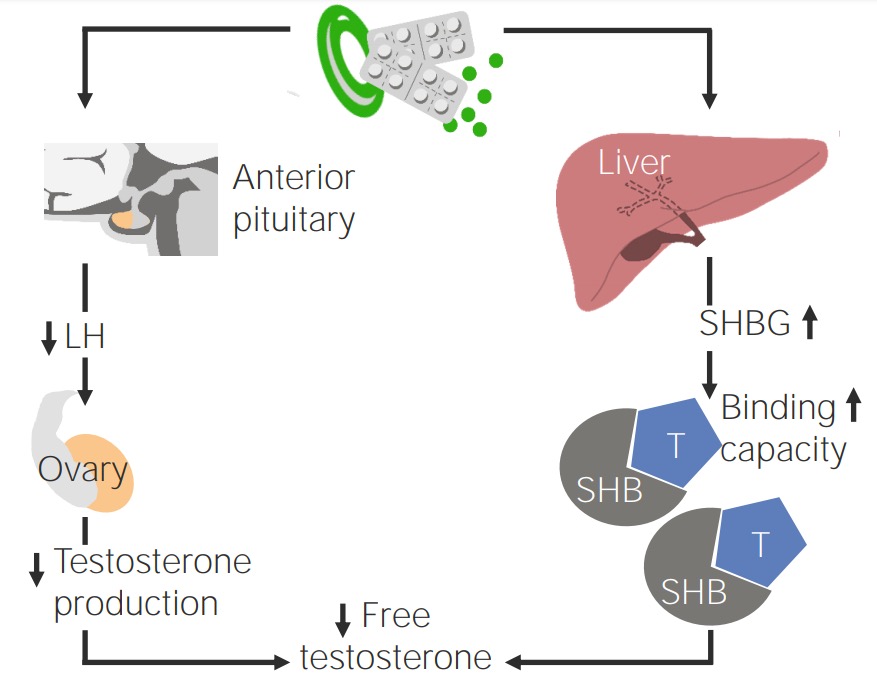
Efeito da contracepção oral em pacientes com SOP
Imagem por Lecturio.