Advertisement
Advertisement
Advertisement
Advertisement
El síndrome de ovario poliquístico (SOP) es el trastorno endocrino más común de las mujeres en edad reproductiva y afecta a casi 5‒10% de las mujeres en ese grupo de edad. Caracterizado por el hiperandrogenismo, la anovulación crónica que conduce a la oligomenorrea (o amenorrea) y la disfunción metabólica, el SOP aumenta el riesgo de infertilidad, hiperplasia o carcinoma endometrial y enfermedades cardiovasculares. La fisiopatología no se conoce del todo, pero se cree que tiene una base genética multifactorial que provoca una alteración en la liberación pulsátil de la hormona liberadora de gonadotropina (GnRH), así como un aumento de la hormona luteinizante (LH), los andrógenos, los estrógenos y la insulina. El resultado es la anovulación crónica y el hirsutismo, los cuales definen la enfermedad. El diagnóstico es de exclusión, por lo que hay que descartar otras causas de hemorragia uterina anormal e hirsutismo. El tratamiento incluye el intento de restablecer la ovulación normal mediante la pérdida de peso, los anticonceptivos orales (ACO) y el apoyo a la fertilidad.
Última actualización: Feb 9, 2023
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Se desconocen los mecanismos exactos, pero se cree que son complejos e incluyen tanto factores genéticos como ambientales. El síndrome metabólico y la obesidad están presentes a menudo, pero no siempre, y probablemente contribuyen a la fisiopatología en algunos individuos.
El síndrome de ovario poliquístico (SOP) debe sospecharse en cualquier mujer en edad reproductiva con menstruaciones irregulares y/o síntomas de hiperandrogenismo, especialmente si es obesa o presenta infertilidad.

Hirsutism in PCOS:
Hair is noted along the side burns, chin, and upper lip; signs of hyperandrogenism.

Male-pattern alopecia in PCOS:
The patient has frontal hair thinning, which is a sign of hyperandrogenism.

Acantosis nigricans en el SOP:
La piel engrosada y oscurecida puede aparecer en la nuca, las axilas o los pliegues de la piel como signo de niveles elevados de insulina por la resistencia a la misma.
El síndrome de ovario poliquístico (SOP) es un diagnóstico de exclusión, por lo que deben descartarse otras causas de oligo o amenorrea e hiperandrogenismo. Los criterios de Rotterdam se utilizan habitualmente para hacer el diagnóstico una vez que se han excluido otras causas.
El diagnóstico requiere 2 de los 3 criterios siguientes:
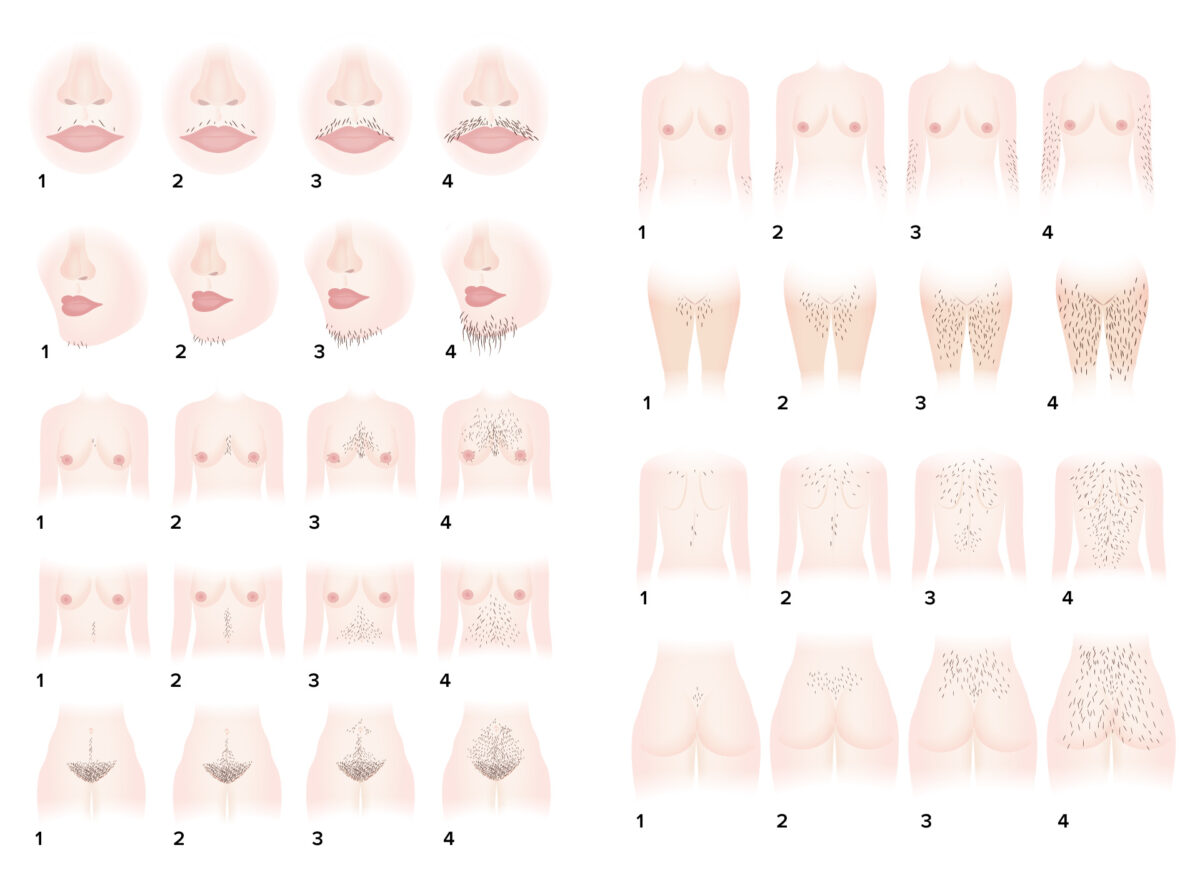
Sistema de puntuación del hirsutismo de Ferriman-Gallwey: un sistema de evaluación objetiva del grado de hirsutismo
Imagen por Lecturio.| Hormones ↑ in PCOS | Hormones ↓ in PCOS |
|---|---|
|
|
FSH: follicle-stimulating hormone
HDL: high-density lipoproteins
LDL: low-density lipoproteins
LH: luteinizing hormone
PCOS: polycystic ovarian syndrome
SHBG: sex hormone-binding globulin

Ecografía de un ovario de apariencia poliquística:
Observe el clasico «collar de perlas» alrededor de la periferia del ovario que identifican los folículos de desarrollo anormal que se observan en el SOP. Los ovarios de apariencia poliquística se observan en aproximadamente ⅔ de las pacientes con SOP y es uno de los 3 criterios diagnósticos de Rotterdam.
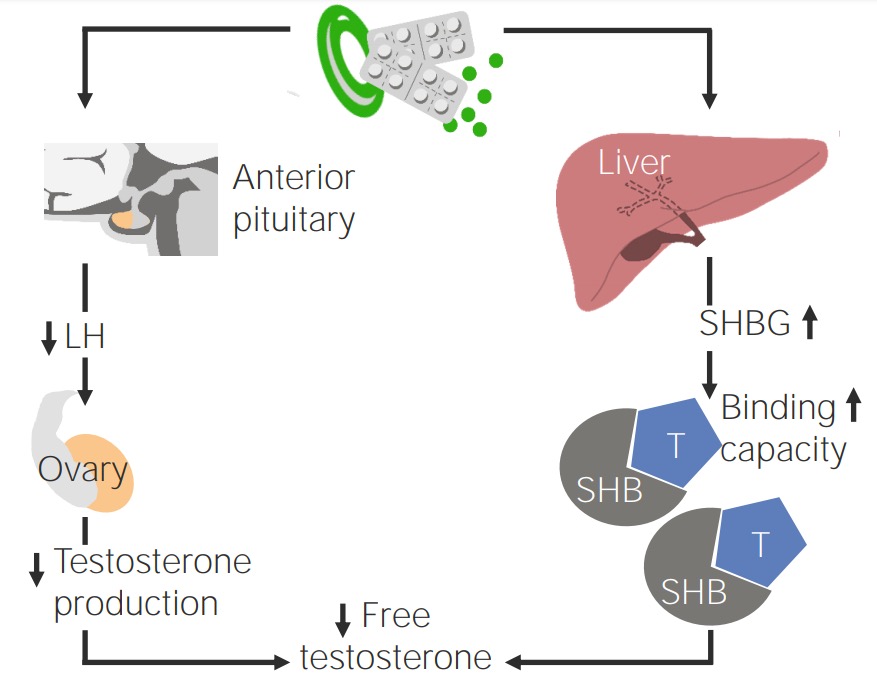
Efecto de los anticonceptivos orales en pacientes con SOP
Imagen por Lecturio.