Playlist
Show Playlist
Hide Playlist
Hepatitis: Diagnosis and Management
-
Slides Hepatitis.pdf
-
Reference List Infectious Diseases.pdf
-
Download Lecture Overview
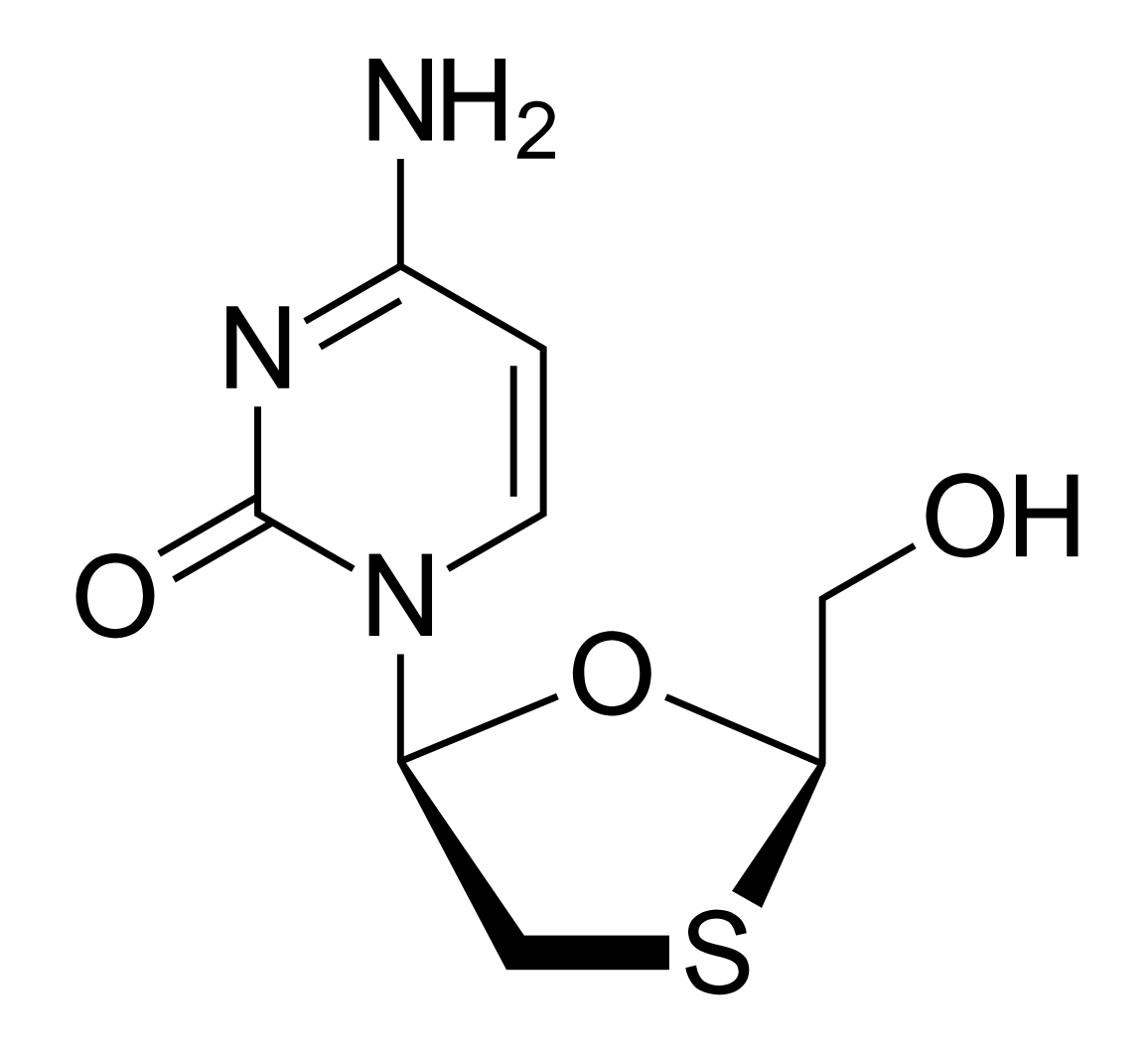
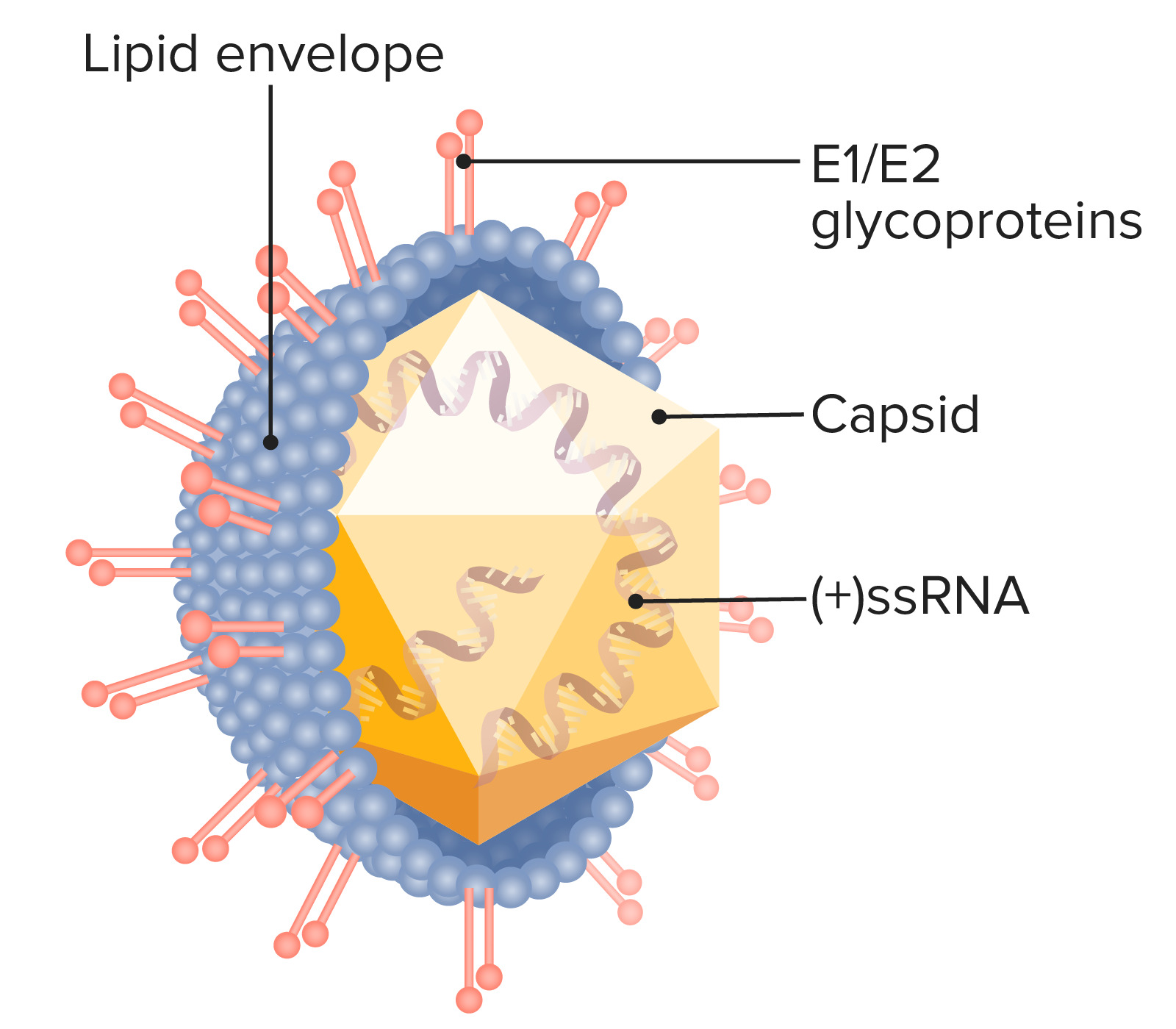
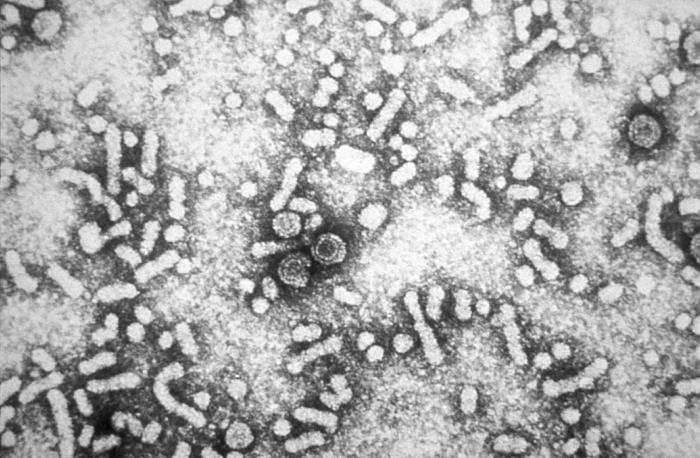
00:01 Let's now see if we can summarize the serology of hepatitis A, B and C. 00:07 First of all, let's take a look at acute hepatitis B. 00:12 In that situation, you would expect the patient to have hepatitis B surface antigenemia and have IgM antibodies to hepatitis B. 00:23 In chronic hepatitis B virus infection, you would expect positive surface antigen but negative for all of the rest. 00:36 Let's say you have acute hepatitis A on top of chronic hepatitis B, well, there is the surface antigen again, you would have antibodies to hepatitis A, you would not have IgM antibodies to hepatitis C and the anti-hepatitis C obviously will be negative. 01:00 So, if a person were to have both acute hepatitis A and B, they would have surface antigenemia, they would have IgM antibodies to hepatitis A and they would have antibodies to hepatitis B of the IgM sort. 01:19 If all they have is acute hepatitis A, their surface antigen would certainly be negative but they would have IgM antibodies to hepatitis A and nothing else. 01:34 Well, let's say a patient has both acute hepatitis A and B but that their surface antigen is below the level of detection, well, naturally their surface antigen would be negative but their antibodies to hepatitis A and hepatitis B of the IgM type would be positive. 01:54 Let's say the patient has acute hepatitis B, but the surface antigen levels are below the level of detection. 02:03 Well, the surface antigen would be negative, the IgM antibodies to hepatitis A and to hepatitis C would be negative but the IgM antibodies to hepatitis B would be positive. 02:19 Let's say all they've got is acute hepatitis C. 02:24 Then the surface antigen, the IgM antibodies to A and B are going to be negative. 02:32 The only one that will be positive are the antibodies to hepatitis C. 02:38 So this may help you solve the problem of what kind of hepatitis does the patient have and those would be the 3 most common that you would encounter. 02:48 So hopefully that helps. 02:51 So if it isn't viral hepatitis, what is it? Well, it could be drug-induced liver injury and we use a lot of drugs that are potentially hepatotoxic in patients so reviewing the drug list of a patient is extremely important. 03:11 In an older person, we have to think about ischemic hepatitis. 03:15 There are conditions of autoimmune hepatitis and a real feared one is this Budd-Chiari syndrome which is thrombosis of the hepatic venous system and of course that produces back-up and destruction of hepatic cells. 03:35 Wilson's disease is a problem of copper retention. 03:41 The metabolism of copper is abnormal and patients with Wilson's disease have high levels of copper in their blood and sometimes precipitates of that copper will appear in the iris of the eye known as Kayser-Fleischer rings. 04:01 And then pregnant women have a variety of problems with the liver that are non-infectious. 04:09 Furthermore, we have to consider Epstein-Barr virus, the cause of infectious mono, and I had the privilege of taking care of a nurse in her 50s who came in with a picture of hepatitis and it wasn't clear for several days into the work-up that what she had was infectious mononucleosis manifesting primarily as hepatitis. 04:36 Cytomegalovirus can do it especially in immunocompromised individuals. 04:41 Herpes simplex is a rare cause of hepatitis and some of the Flaviviruses, arthropod-borne, can cause a hepatitis. 04:54 Now, let's discuss an overview for the management of viral hepatitis. 04:57 It's generally accepted that acute viral hepatitis does not require specific treatment in most cases. 05:03 Acute hepatitis A, has an excellent prognosis. This is also true for acute hepatitis B. 05:08 As most patient will clearly infection on their own. 05:11 The story changes when we discuss chronic hepatitis B, where treatment is almost always recommended. 05:16 Medications can include pegylated interferon as well as nucleoside and nucleotide analogues such as entecavir and tenofovir. 05:24 The treatment is complex and is usually handled by a specialist. 05:28 Now, for acute hepatitis C, the story changes slightly, as patients much more frequently progress to chronic infections and require treatment. 05:36 The combination recommended by the Infectious Diseases Society of America (IDSA) and the American Association for the Study of Liver Diseases (AASLD) is glecaprevir (a protease inhibitor that targets the NS3/4A protein) and pibrentasvir (a protein inhibitor that targets the NS5A protein). The efficacy of this combination across all Hepatitis C virus (HCV) genotypes is greater than 95%. The cost of 8 weeks of therapy is approximately $26,000, though this can vary. In specific clinical scenarios, such as decompensated cirrhosis, though this requires careful monitoring due to potential side effects like anemia. Ribavirin is contraindicated in pregnancy. 06:26 The choice of medication is complex, and it depends on factor such as viral genotype, presence of cirrhosis, and prior treatment history. 06:33 For these reasons, it's also usually handled by a specialist. 06:37 Finally, regarding hepatitis E, while anti-HEV IgM testing is commonly used as an initial screen, it requires confirmatory testing due to high variability in commercial assays. HEV RNA detection in serum or stool is essential for diagnosis confirmation, especially in chronic cases and immunocompromised patients where antibody tests often give false negatives. Most cases are self-limited, but for severe cases, ribavirin can be used if the patient is not pregnant. Treatment cases are referred to specialists. So, one of the things that worries physicians certainly because of the high incidence of cirrhosis is hepatitis C. 07:23 So, how do we approach a patient? Well, we first check for hepatitis C antibodies. 07:29 If they don't have hepatitis C antibodies, they're negative or non-reactive. 07:34 There's no infection with hepatitis C and that's it, we don't do anything more. 07:41 On the other hand, if their hepatitis C antibodies are positive, reactive, then we need to do an analysis of the amount of hepatitis C that's present in the bloodstream, so-called hepatitis C viral RNA, a viral load if you will. 08:02 If there's none detected, then there's no current hepatitis C infection, they were one of the lucky ones who got over the infection themselves and you would do additional testing as appropriate but it's not hepatitis C causing the problem. 08:20 If on the other hand the viral load for hepatitis C, the HCV RNA is detected, then they need treatment. 08:32 They have a current infection and you need to link them to a specialist in hepatitis C.
About the Lecture
The lecture Hepatitis: Diagnosis and Management by John Fisher, MD is from the course Gastrointestinal Infections.
Included Quiz Questions
A patient has a positive HCV antibody test. What is the most appropriate next step in diagnosis?
- HCV RNA testing
- Liver biopsy
- Repeat the HCV antibody test
- Genetic testing
- Liver imaging studies
Which of the following tests is most indicative of acute hepatitis B infection?
- Positive HBsAg and IgM anti-HBc
- Positive HBsAg, negative anti-HBc
- Positive HBsA and HBsAb
- Positive HBsAb, negative HBsAg
- Positive HBeAg, HBsAg, and HBsAb
A patient has positive HBsAg, IgG ant-HBc, and IgM anti-HAV. What is the most likely diagnosis?
- Acute hepatitis A and chronic hepatitis B infections
- Acute hepatitis A and B infections
- Chronic hepatitis B and A infections
- Chronic hepatitis A and acute hepatitis B infections
- Acute hepatitis A infection and chronic hepatitis B and C infections
What is the treatment for acute hepatitis A infection?
- Supportive
- Ribavirin
- Corticosteroids
- Pegylated interferon
- Interferon-alpha and lamivudine combination therapy
Tenofovir or entecavir are commonly used as the initial regimen to treat which kind of hepatitis?
- Chronic hepatitis B infection
- Acute hepatitis B infection
- Chronic hepatitis C infection
- Acute hepatitis C infection
- Acute hepatitis E infection
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
1 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Your lectures are excellent because you have a great diction! Thanks.
Very comprehensive discussion. It would have been worthwhile to talk about criteria for starting treatment for chronic Hep B (e.g DNA count vs symptoms and livers functions). Also unclear if treatment of HepB is curative. The hepatitis talks did not mention genotypes of Hep C at all which is important for treating the condition, particularly in countries where access to direct acting antivirals is not available. Finally the talks didn't mention what percentage of patients with chronic Hep B and C go on to develop cirrhosis and hepatocellular carcinoma.