Playlist
Show Playlist
Hide Playlist
Scrotal Masses in Adolescent Males: Testicular Torsion, Epididymitis, Hydrocele & Varicocele
-
Slides ScrotalProblems Pediatrics.pdf
-
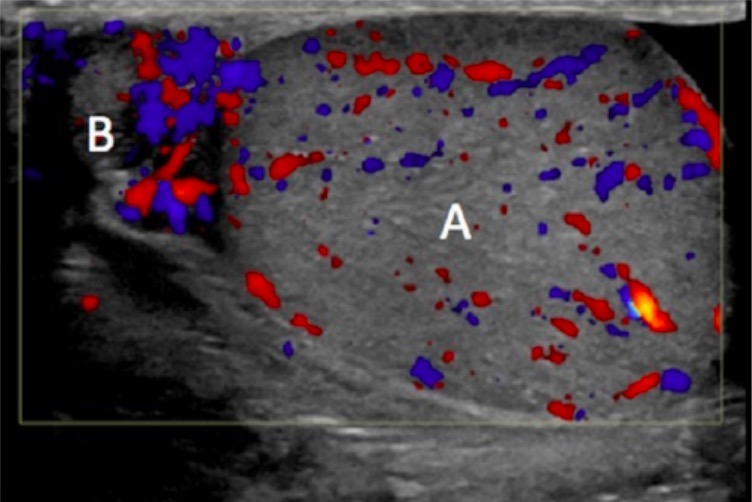
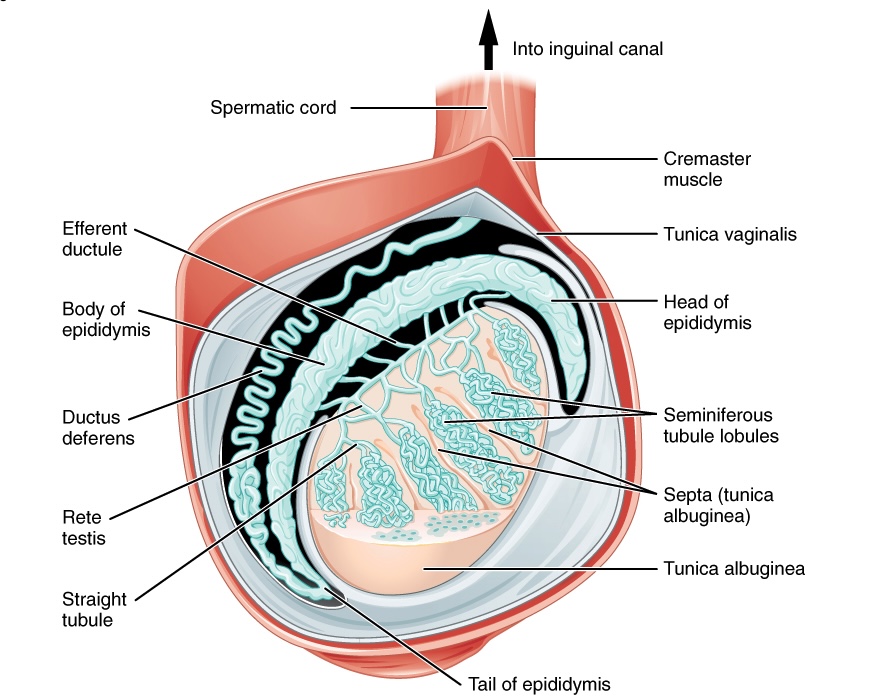
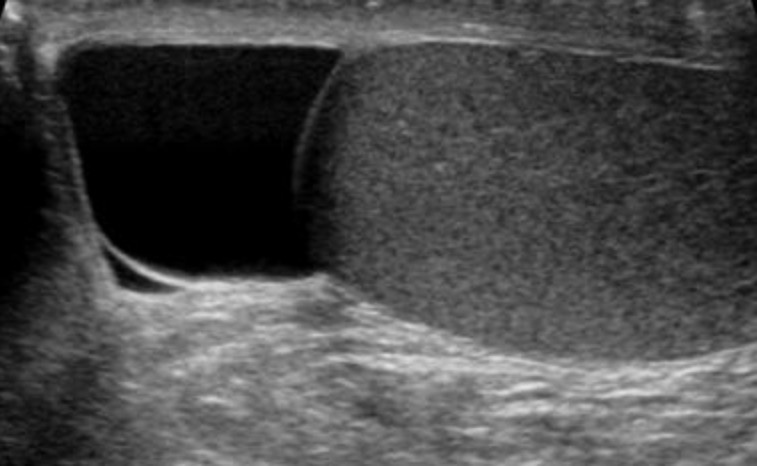
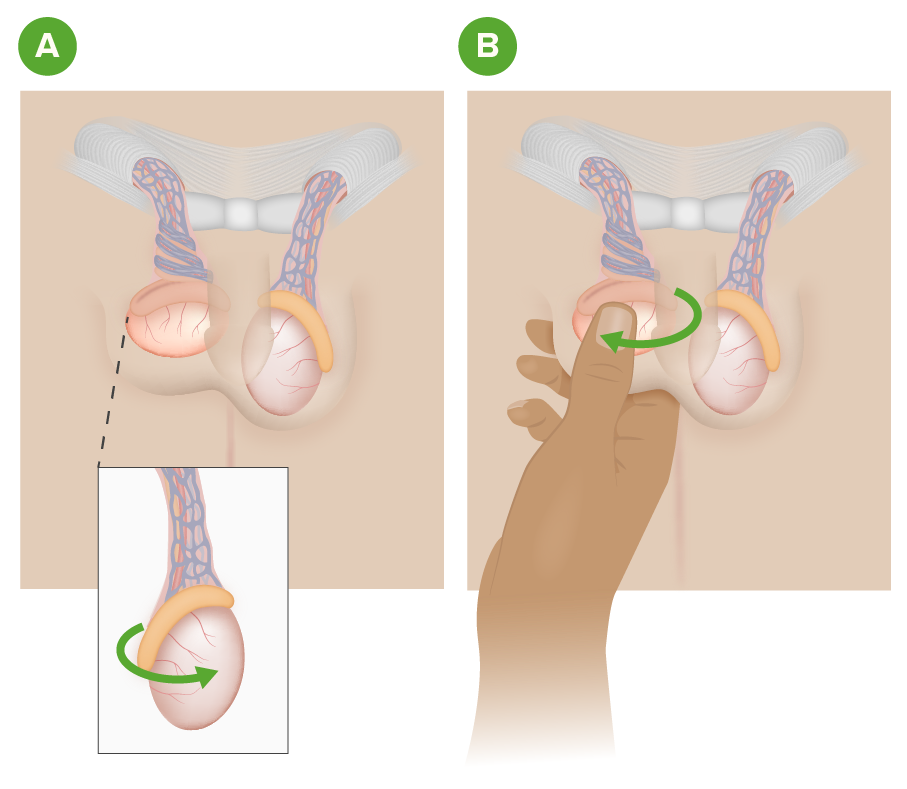
Download Lecture Overview
00:01 In this lecture, we will discuss scrotal masses in adolescent males. Masses can be palpated in any scrotal structure. They may be painful or non-painful. One of the reasons we worry about these masses is because testicular cancer in particular can happen early on in adolescent male life. 00:22 So, let’s review this. Testicular cancer is most common in 15-35 year old males. It has an excellent prognosis if it’s picked up early. But let’s go through what could be a scrotal mass. 00:39 Testicular torsion, epididymitis, hydroceles, spermatoceles, and varicoceles are all potentially palpable scrotal masses in adolescent males. So, let’s talk about testicular torsion first. 00:53 Testicular torsion is a twisting of the spermatic cord. It causes an obstruction of blood flow which can then lead to ischemia. If you see a patient with a testicular torsion, they generally have a painful, blue unilateral testis that’s elevated and has a sideways lie. It can occur bilaterally in some patients and may recur after treatment. Also, if painful testes are present and there’s a blue dot on the scrotum, this might be a torsion of the appendix testis which is less concerning in that you just provide pain relief and it gradually resolves. Epididymitis on the other hand is an inflammation of the epididymis. This can cause a palpable mass. Toddlers get epididymitis from urinary tract infection organisms but adolescents typically get it from ascending sexually transmitted diseases classically gonorrhea and chlamydia. So, another mass is the hydrocele. We see this more commonly in toddlers. This is a fluid collection in the tunica vaginalis surrounding the testis. 02:04 A spermatocele is a little bit higher up and it’s a retention cyst which is filled with sperm and is located in the epididymis. Another problem that can arise in adolescents is a varicocele. 02:21 This is a dilatation of veins in the pampiniform plexus of the scrotum. This results in a pressure in the left testicular vein more so often than the right testicular vein. This higher pressure plus an incompetent venous valve results in a pooling of blood in the plexus. If you see a patient who has a scrotal mass, it’s important to take a detailed history. Ask about the history of onset, whether it’s severe or very painful and the location. Ask about a history of trauma, certainly sexual activity is important. Ask about urethral symptoms. Does the patient have a urethritis or signs of infections such as dysuria. Ask about whether they’ve received the mumps vaccine. 03:08 Very rarely, mumps can cause an orchitis. Ask about undescended testis or malignancies in the past. 03:15 Of course, ask about any associated symptoms. When we examine the mass, it’s important to do it carefully and slowly. Sometimes the patient may feel awkward but take your time. 03:27 You examine the mass. You localize where any swelling or tenderness is in the testicle or in the epididymis or higher up. Notice the position of the testicle and the epididymis. 03:40 Examine the patient both lying down and standing up. Assess the cremasteric reflex. 03:47 That’s important because any entrapment of that cremaster muscle will result in a reduced cremasteric reflex. And especially for hydroceles or varicoceles, trans-illumination is helpful. 03:59 We’ll talk about that in a bit. So, when you examine the mass, there are some things that you may see that may be consistent with certain diagnoses. So, if you feel a mass within the body of the testicle, the testicle itself feels normal but then there’s a side mass. That’s probably cancer especially if it’s non-tender. 04:19 If you feel a knot in the spermatic cord, that’s torsion. Torsion is hard to miss because those patients are in incredible pain. There’s a sideways lie. There may be discoloration of the testicle. 04:32 If you feel a mass above and posterior to the testicle, that’s probably an inflamed epididymis. 04:39 If you feel something anterior to the testicle, that’s a hydrocele. Trans-illumination should really light up that entire testicle. Trans-illumination really works in hydrocele. If you feel a mass within the epididymis, that may be a spermatocele. So, if you’re feeling along that epididymis and then there’s a mass, that’s probably a spermatocele. If you feel a baggy, sort of almost wormy bag of masses, that’s probably a varicocele. That’s usually felt within the cord. So, key things are determining whether it’s painful or non-painful. That will help you narrow down your differential diagnosis. 05:18 So, painful masses include testicular torsion, a torsed appendix testis - that’s the blue dot, epididymitis, orchitis, a hematoma such as a traumatic hematoma, or an incarcerated hernia. Non-painful would be a hydrocele, a spermatocele, a varicocele, a testicular tumor, or a non-incarcerated hernia. 05:40 A non-incarcerated hernia generally should be reducible when pushed back up the spermatic cord. 05:46 Testing the cremasteric reflex is important part of the testicular exam. For a normal reflex, we notice an elevation of the testis after stroking the ipsilateral or inner thigh, the same side. 05:58 Sometimes people like to use something cold. If it’s abnormal, you should suspect testicular torsion. 06:05 A twisting of the cord can interfere with the contraction of the cremasteric muscle. So, let’s talk a little bit about trans-illumination. We see this really well in patients with a hydrocele. So, here’s a picture of somebody trans-illuminating a hydrocele in a child. Basically, you’ll hold the light up against the scrotum and the whole area should really shine right through. It will do that if there’s a block in the drainage of that fluid. This indicates a cystic structure such as a hydrocele or a spermatocele. 06:35 A mass that does not illuminate, you should be concerned about the possibility of a tumor. 06:41 We do sometimes get labs. Certainly, if a patient has evidence of a urethritis, we might suspect epididymitis. 06:49 In an adolescent, that means getting a nucleic acid amplification test or a test for chlamydia or gonorrhea. Also, if a patient has a mass, it’s important to do some tumor markers to try and identify what type of mass that is. So alpha fetoprotein, hCG, or lactate dehydrogenase are all fairly useful. 07:12 What radiologic studies do we do? Well, the best test for imaging the scrotum and the testicles is an ultrasound. 07:21 This visualizes tumors, notices hydroceles, can assess for dilatation of the pampiniform plexus in the case of a varicocele. So, we’ll do a Doppler ultrasound. Doppler is also useful because it assesses blood flow. In the case of a torsed testis, it should show an area of decreased blood flow because the whole point is that that testicle is having a decreased arterial flow from the torsion and the twisting of the root of that testicle. Then in epididymitis, you may see also either an increased flow or a normal flow. Sometimes the increased flow is just from the hyperemia and the infection causing vascular dilatation. Surgical therapy is indicated certainly for torsion and it’s an emergency. Generally before surgical therapy, if you wish to try to reduce it, you can try and open the book or twist outward and that will allow a reduction, although often these patients go on to surgery. If the testicle is no longer viable which is unfortunately reasonably common, they simply remove it. Then they may do a testicular implant afterwards for cosmesis purposes. 08:30 Let’s talk about treatment. For an asymptomatic individual who has a hydrocele, a spermatocele, or a varicocele, there’s really no intervention needed. For epididymitis, we’ll generally give antibiotics. 08:44 For a torsed appendix testis which has a normal prognosis, it’s really just pain control until the pain resolves. NSAIDs usually do the trick. Of course for tumor, we’re going to refer that patient to a pediatric oncologist for a complete workup but usually excision is needed. 09:00 So, that’s my review of testicular masses in adolescent males. Thanks for your time.
About the Lecture
The lecture Scrotal Masses in Adolescent Males: Testicular Torsion, Epididymitis, Hydrocele & Varicocele by Brian Alverson, MD is from the course Adolescent Medicine. It contains the following chapters:
- Scrotal Masses
- Physical Exam Features
- Lab Studies
Included Quiz Questions
What is the next best step for a patient with torsion of the appendix testis?
- Ibuprofen and bed rest
- Manipulation
- Surgery
- Broad-spectrum antibiotics
- Steroids
Which of the following is most accurate regarding testicular cancer?
- It commonly affects men 15-35 years old.
- The majority are painful.
- The majority have a poor prognosis.
- Gynecomastia is commonly a presenting manifestation.
- Surgery is less often curative.
Which of the following is NOT a scrotal mass in adolescent males?
- Inguinal hernia
- Testicular torsion
- Hydrocele
- Varicocele
- Epididymitis
A 10-year-old boy is brought to the physician with acute-onset pain in the scrotum. On physical examination, the "blue dot sign" is observed. The testicle is non-tender. Which of the following is the most likely diagnosis?
- Torsion of appendix testis
- Testicular torsion
- Hydrocele
- Varicocele
- Epididymitis
Which of the following disorders refers to the dilatation of the pampiniform plexus of spermatic veins?
- Varicocele
- Testicular torsion
- Hydrocele
- Epididymitis
- Torsion of appendix testis
Which of the following is most often painful?
- Epididymitis
- Varicocele
- Hydrocele
- Spermatocele
- Testicular tumor
Which of the following disorders is most likely to transilluminate during physical examination?
- Hydrocele
- Varicocele
- Testicular tumor
- Epididymitis
- Testicular torsion
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Very clear differential physiopathology and differential diagnosis. Thank you very much!