Playlist
Show Playlist
Hide Playlist
Other Forms – Bleeding Disorders
-
Slides Bleeding disorders.pdf
-
Reference List Hematology.pdf
-
Download Lecture Overview
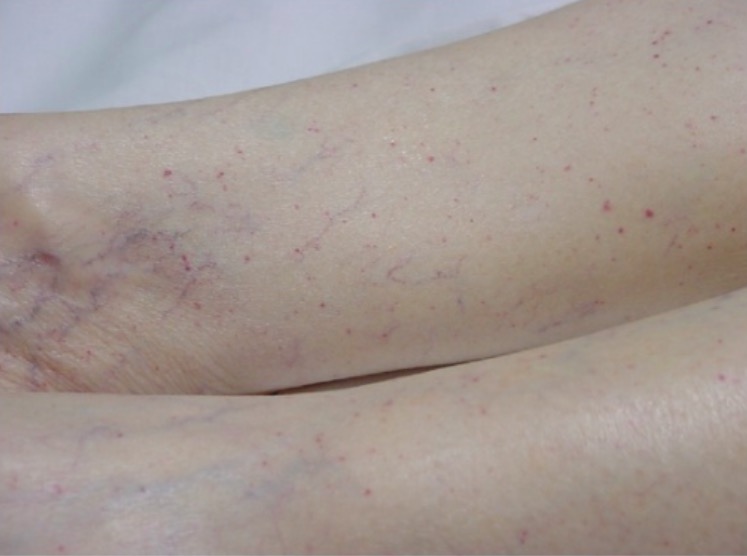
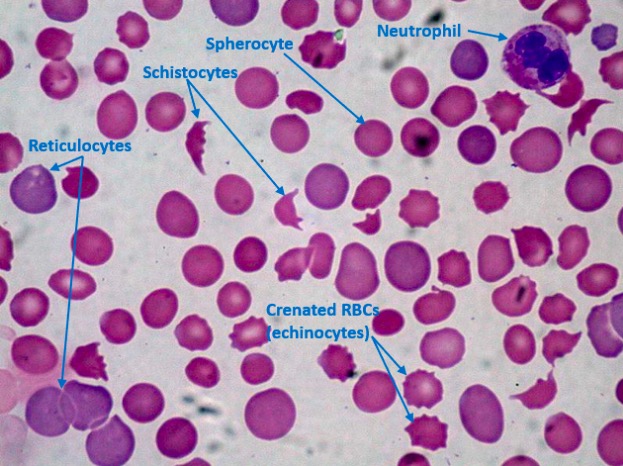
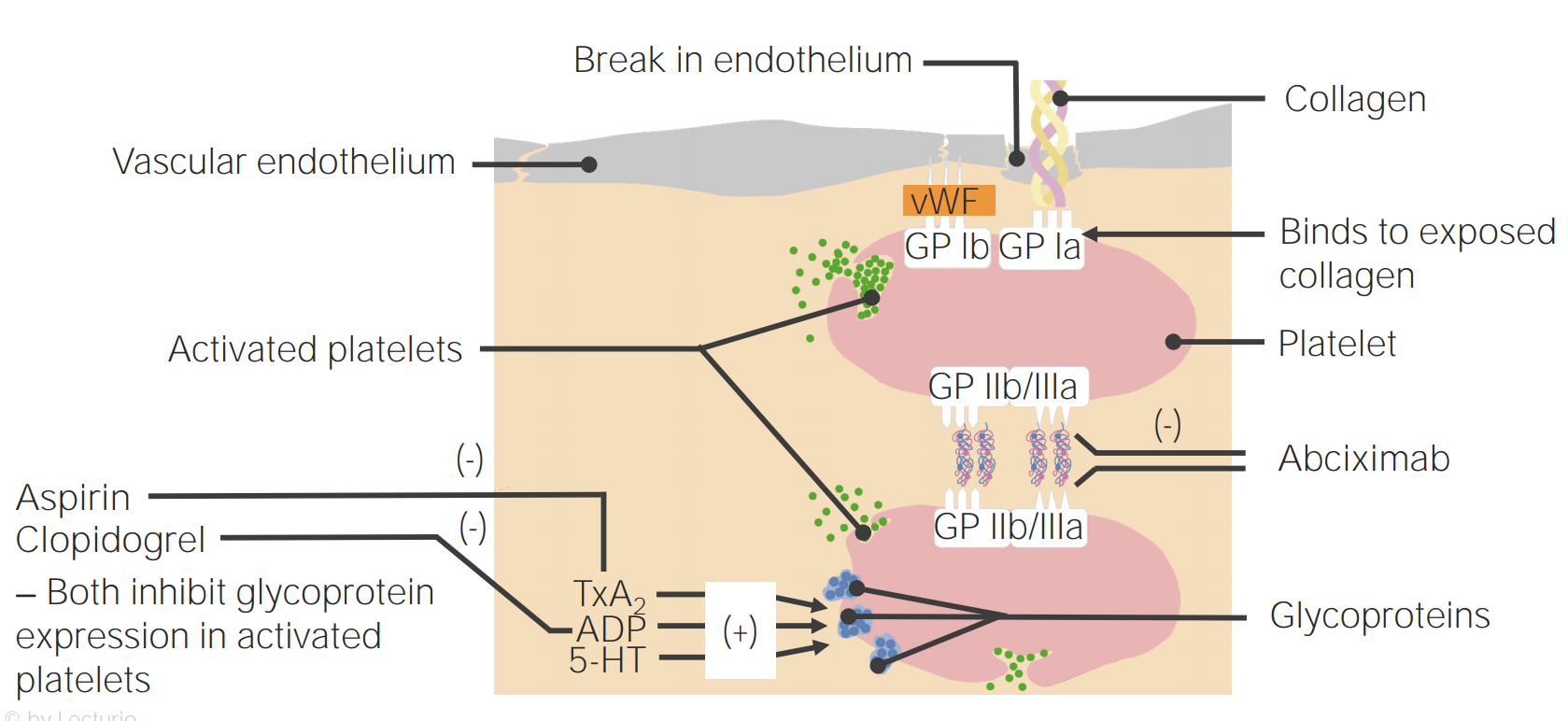
00:01 Now, let's look at some of the clinical disorders that can lead to bleeding problems, and I want to start with the vessel itself before we move on to consider the platelet and then the coagulation factors. 00:15 Now, let's look at the vessels, vascular disorders. 00:19 Now, sometimes these can be inherited, probably the most important one is represented with the clinical picture on the right. 00:28 This is called hereditary haemorrhagic telangiectasia. 00:33 It has an autosomal dominant inheritance and involves proteins which involved in collagen formation and strength. 00:42 Endoglin is one of these molecules that's often mutated. 00:47 And these telangiectasia develop in the skin, the mucous membranes and also in internal organs. 00:55 It can be a challenging condition to treat. 00:58 But we will use local factors, sometimes embolisation and perhaps even hormonal treatment. 01:07 There are also acquired disorders that can affect the ability of our vessels to stop blood clotting. 01:15 Probably the most common is aging. 01:18 As our skin gets older, it gets thinner and you often see bruises in older people. 01:24 Steroids as well thin skin and that's one reason you shouldn't keep putting high dose steroids onto areas of the skin. 01:33 On the right is the hand of an elderly person, you can see some of that bruising in the skin, which has become very thin. 01:45 But two of the conditions on that slide which are themselves of interest. 01:49 One is a relatively rare ondition, but very interesting, Henoch-Schonlein purpura. 01:56 This is often seen in young people after a recent infection. 02:01 And it's a vasculitis mediated through IgA and it leads to a purpura on the extensor parts of the limbs and on the buttocks. 02:12 And finally at the bottom, a classic disease, scurvy, which I'm sure you know, used to blight many sailors who went round the world on long trips and didn't get sufficient vitamin C. 02:25 Vitamin C is quite important for maintaining collagen in its most active form, and so bleeding was a major problem with scurvy. 02:36 We rarely see it now, but sometimes if people are on very poor diets, you may see perifollicular hemorrhages in vitamin C deficiency. 02:46 Now, let's look at some platelet disorders and we'll start in disorders where there are low numbers of platelets, so-called thrombocytopenia. 02:55 And as you'll see on the left, this can be due to increased destruction or at the bottom, decreased production. 03:04 Let's look at some of the ways by which platelets can be destroyed. 03:10 The most common is an immune disorder, immune mediated thrombocytopenia. 03:16 And here, the body produces IgG antibodies against the platelets and that leads to their destruction. 03:25 Sometimes it's triggered by a recent infection or sometimes it can occur out of the blue and it can be seen in young people or older people. 03:35 It can be treated in a number of ways, some of them are represented on the slide. 03:41 Steroids, we may remove the spleen perhaps, or we can use drugs which stimulate thrombopoietin-receptor activity. 03:53 Other disorders which reduce the platelet count - severe infections, there's a modest reduction in the platelet count during pregnancy, which is not clinically important, and sometimes drugs can cause this effect. 04:08 Another cause that I've put up there, thrombotic thrombocytopenic purpura, an important disorder that I want to discuss on the next slide. 04:18 Platelets can also be reduced because of decreased production. 04:21 The bone marrow is simply not making enough platelets and we see that in patients who have bone marrow failure due to aplastic anemia or chemotherapy. 04:32 Now, if your platelet count is reduced, you tend to get bruising or mucous membrane bleeds and you'll see on the right a patient with quite severe bruising and purpura on the skin due to thrombocytopenia. 04:49 Now, let me just talk a little bit more about that disorder with a very long name, thrombotic thrombocytopenic purpura, the name is quite interesting in itself because we're suggesting that there's low platelets here, it's thrombocytopenic, and you've got purpura - bruising, but thrombotic as well. 05:08 So we're getting blood clots. 05:10 So it's a paradox of clotting and bruising. 05:14 How can this happen? Well, fortunately, it's a rare disorder, but it's fascinating pathophysiology. 05:23 In this disorder, patients have a deficiency of the metalloprotease, an enzyme that's called ADAMTS13, as you can see on the slide. 05:34 Sometimes it's congenital and we see this disorder in children, but in adults, it's an autoimmune disorder and these patients developed an antibody against that protein. 05:47 Now, one of the important functions of that protein is to break down Von Willebrand factor into smaller components because vWF is made in very large aggregates and it needs to be broken down. 06:03 If you're deficient in this enzyme, you have very large circulating multimers, as we call them, of vWF and they adhere the platelets very strongly to your vessels. 06:16 That's why you get thrombocytopenic purpura, because the platelets stick to the vessel. 06:22 But those platelet plugs also damage red cells that are trying to get through. 06:27 And as you'll see on the right, that's a blood film in TTP and you'll see all those damaged and sheared red cells. 06:36 And that produces the, as you can see, hemolytic anemia and this can reduce blood flow to organs like the brain, the kidney, and also cause a fever producing that classic spectrum of symptoms that I've put there. 06:53 This can be a very serious disorder if it is not recognized, with a high fatality rate. 07:00 And so it's important that it's treated and the best way to treat it is with plasma exchange taking off the patient's plasma and infusing it from a donor. 07:14 As well as just abnormalities in platelet number, we can also get disorders of platelet function. 07:22 I've represented some here, there are rare inherited disorders that we see in children. 07:29 And there's two of the classic types: Glanzmann's disorder and Bernard-Soulier disease, and you can see that they affect two of the proteins we've learnt about in this lecture IIb/IIIa and Ib, and you now understand how that can lead to bleeding disorders. 07:47 But at the bottom, of course, acquired disorders of platelet function, with the most common of the use of antiplatelet drugs, very widely used by millions of people around the world - aspirin, clopidogrel and so forth. 08:04 On the right, we've got a nice example of platelet aggregometry platelet testing. 08:11 Here we take blood, we put platelets into a tube and we shine light through that tube. 08:17 Now, if you put in various molecules such as ADP, collagen, adrenaline, as you can see at the top, the agonists, that will cause the platelets to adhere and aggregate and more light can go through the system, as you'll see on the left, increasing light transmission. 08:37 And in green, you'll see what happens when you add the agonists. 08:41 the platelets adhere, more light can shine through. 08:45 But in the top, in pink, there are platelets from somebody with Glanzmann's disease, Glanzmann's thrombosthenia, and you'll see there's no platelet adhesion or aggregation at all. 08:57 That's a commonly used test to assess platelet function. 09:02 Now, let's finish by talking about the coagulation disorders. 09:06 And we'll start with the inherited types. 09:08 Hemophilia A is the classic condition in this area due to deficiency of factor VIII. 09:16 It's X-linked, and therefore it's only seen in boys. 09:20 With the frequency, you can see around 30-100 per million. 09:25 Now, the gene may run in families, passed on from the mother, or it may result from a new mutation. 09:33 So, sometimes it spontaneously arises in the family. 09:36 Now, if this is untreated, it's a very serious disease. 09:41 It tends to start with bruising in babies, but throughout life, you can get serious bleeds thickly into joints and muscles. 09:52 Very characteristic feature of this disease. 09:55 You'll see on the right, what can happen to the joints after frequent bleeds into them, and it used to lead to a lot of disabling arthropathy. 10:05 Fortunately, factor VIII concentrates are now available, and they can prevent this bleeding and also stop it once it started. 10:17 And what we've seen in the treatment of hemophilia, is a move away from waiting until a patient have a bleed and then treating them to giving factor VIII prophylactically stop the bleeding. 10:31 And that's because if you look on the right, at the top, there's a chart there showing that the amount of factor VIII in the blood determines the severity of the disease and you can see values there suggesting severe, moderate, or mild disease. And with prophylactic therapy, only a modest increase in factor VIII can dramatically reduce the number of bleeds that the patient gets. 10:59 And so, that's the approach that we need to aspire to in the management of hemophilia. 11:04 At the bottom is hemophilia B, a rarer subtype, and that's due to deficiency of factor IX. 11:12 Another inherited disorder of coagulation is Von Willebrand disease. 11:19 This is due to a deficiency or inactivity of that factor vWF that we've mentioned so much during this talk. 11:27 Now, the prevalence of this is actually not that low, one in 10,000 individuals. 11:33 And I've put it at the top right there, a reminder of the activity of vWF. 11:39 Linking the platelet through GP Ib to the damaged vessel on the collagen. 11:45 vWF also carries factor VIII. That's another a bit important function. 11:51 Now, at the bottom, I've shown you electrophoresis diagram which represents some of the subtypes of Von Willebrand disease, and you can see that there are several. 12:02 From type 1, where there's a modest reduction of vWF to type 3 when there's really none at all, and that's a very serious bleeding disorder. 12:11 We can treat this disorder by local factors. 12:15 Drugs such as DDAVP, which release vWF, and sometimes we need vWF infusions, which we can generate. 12:25 Finally, acquired disorders of the coagulation system. 12:30 On top here, I've put disseminated intravascular coagulation. 12:34 DIC most often presents with bleeding, manifesting with bruising, skin petechiae, or oozing from wounds or IV sites. It can also present with venous or arterial thrombosis due to clotting, and rarely, gangrene. 12:52 Now, this is a paradoxical disorder because in fact, there's excessive coagulation. 12:57 What that does is it depletes coagulation factors and leaves the patient very prone to bleeding. 13:04 It's usually triggered by extrinsic events, severe infections, perhaps severe problems in child birth, and the classic clinical feature of DIC is that patients bruise and bleed spontaneously. 13:24 They may have had blood taken a day or two ago and suddenly the venipuncture site start to ooze. 13:31 The whole blood system fails to clot. 13:34 And that needs to be treated by infusions of things like fresh frozen plasma, and platelets, perhaps fibrinogen through cryoprecipitate. 13:47 Second disorder, vitamin K deficiency. 13:51 Sometimes, you see it in the newborn and those with liver disease. 13:55 Vitamin K is needed to activate several of the clotting factors. 13:59 And again, that's why warfarin works as an antithrombotic agent by inhibiting vitamin K. 14:06 And finally, a rare disorder, acquired hemophilia, this is seen in adults and they have a clinical picture that resembles inherited hemophilia, but this is developed not due to congenital deficiency, but due to an autoimmune disease against the factor VIII. 14:25 And that can be very challenging to treat. 14:27 So, in summary. Hemostasis depends on the interaction of the blood vessel, the platelets, and the coagulation system. 14:37 Vessels and platelet disorders lead to bleeding into the skin and mucous membranes. 14:44 Immune thrombocytopenia is the most common cause of thrombocytopenia. 14:51 Hemophilia is the most important inherited coagulation disorder, but can now be managed by the use of prophylactic factor VIII. 15:00 I hope you've enjoyed this lecture on bleeding.
About the Lecture
The lecture Other Forms – Bleeding Disorders by Paul Moss, PhD, OBE, FMed, FRCPath is from the course Hematologic Disorders.
Included Quiz Questions
A 24-year-old woman notices bleeding from a venipuncture site during a difficult childbirth. Full blood count shows the platelet count has fallen from the normal value to 30 over 6 hours. Which of the following is the most likely diagnosis?
- Disseminated intravascular coagulation
- Immune thrombocytopenic purpura
- Acquired haemophilia
- Neonatal thrombocytopenia
- Scurvy
Which ONE of these is a primary disorder of the blood vessel?
- Hereditary haemorrhagic telangiectasia
- Haemophilia
- Warfarin overdose
- Immune thrombocytopenia
- Disseminated intravascular coagulation
Which of the following molecules is often mutated in patients with hereditary hemorrhagic telangiectasia?
- Endoglin
- Endostatin
- Tyrosine kinase
- Endothelin
- Endogenin
What type of antibodies are directed against platelets in immune-mediated thrombocytopenia?
- IgG
- IgM
- IgA
- IgD
- IgE
Which of the following is deficient in thrombotic thrombocytopenic purpura?
- ADAMTS13
- ADAMTS31
- ADAMTS15
- ADAMTS21
- ADAMTS11
Which of the following statements is FALSE regarding thrombotic thrombocytopenic purpura?
- It is treated with platelet transfusions
- It is associated with microangiopathic hemolytic anaemia
- The patient often presents with fever and renal failure
- It is caused by a deficiency of ADAMTS13
- It can present as congenital or autoimmune
Which of the following disorders is associated with abnormalities in IIb/IIIa?
- Glanzmann's
- Bernard Soulier syndrome
- Von Willibrand disease
- Hemophilia A
- Thrombotic thrombocytopenic purpura
Bernard-Soulier syndrome is caused by abnormalities in which of the following molecules?
- Ib
- IIb/IIIa
- IXb/IIIa
- IIIa
- IX/X
What levels of factor VIII are seen in severe haemophilia A?
- Less than 2 units / dl
- 5 to 45 units/dl
- 2 to 5 units/dl
- 45 to 90 units/ dl
- More than 90 units
Which of the following clotting factors is deficient in hemophilia B?
- Factor IX
- Factor XII
- Factor XI
- Factor VIII
- Factor VII
Which of the following types of Von Willebrand factor disease does not have vWF multimers?
- Type 3 Von Willebrand disease
- Type 1 Von Willebrand disease
- Type 2A Von Willebrand disease
- Type 2N Von Willebrand disease
- Type 2B Von Willebrand disease
With which of the following clotting factors is Von Willebrand disease associated?
- Factor VIII
- Factor XII
- Factor XI
- Factor IX
- Factor VII
Customer reviews
3,3 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
2 |
the lecture was very thorough explained in detail understood the lecture and saved me a lot of time
6 customer reviews without text
6 user review without text