Excellent
By Blaze B. on 04. April 2024 for Ischemic Heart Disease: Development
Excellent lecture on the pathological timeline of MI and IHD.
Lack of depth.
By Ali J. on 24. April 2023 for Management of Angina and Myocardial Infarction: NSTEMI and STEMI Treatment
The treatment options, steps, and the overall approach to STEMI and NSTEMI patients was absolutely insufficient in this video compared to the information we must know for exams. So vague. Most of us are medical students, we know we have to use beta blockers, the real questions are when and how much? He should've gone over a systemic approach to such patients. The initial management and etc.
Very useful
By Nas A. on 13. November 2021 for Ischemic Heart Disease: Basic Principles with Carlo Raj
Very useful content with a good basis to understand the more serious presentations of IHD. It is also very well presented
Cardio Pathology
By Jenny A. on 08. October 2021 for Ischemic Heart Disease: Basic Principles with Carlo Raj
Dr. Raj makes the lecture more interesting with how he delivers the topic and the explanations behind it. His constant repetition of the topic makes one retain the information by heart. He is very smart and knows the topic very well the way he says it. I like all of his discussions…
Awesome
By Büşra Nur A. on 03. August 2021 for Ischemic Heart Disease: Basic Principles with Carlo Raj
Mr. Raj is awesome, I like his lecturing style a lot. Thanks!
Great Presentation
By Adewale K. on 21. January 2021 for Coronary Steal Syndrome
He's just brilliant, and I'm so engaged and interested. He's making me love Cardiology!
Amazing lectures by Dr. Raj
By Kevin Wilfredo A. on 30. November 2020 for Management of Angina and Myocardial Infarction: Treatment and Complications after (N)STEMI
Great overview! I personally loved to picture the concepts and pathophysiology in my mind.
Repeating concepts
By Laura N. on 25. November 2020 for Ischemic Heart Disease: Basic Principles with Carlo Raj
Mr. Carlo Raj has a particulary way of teaching that makes me get involved and really understand the content. He repeats the key concepts so many times so when the lesson finishes i have achieve the most important knowledge of such mater.
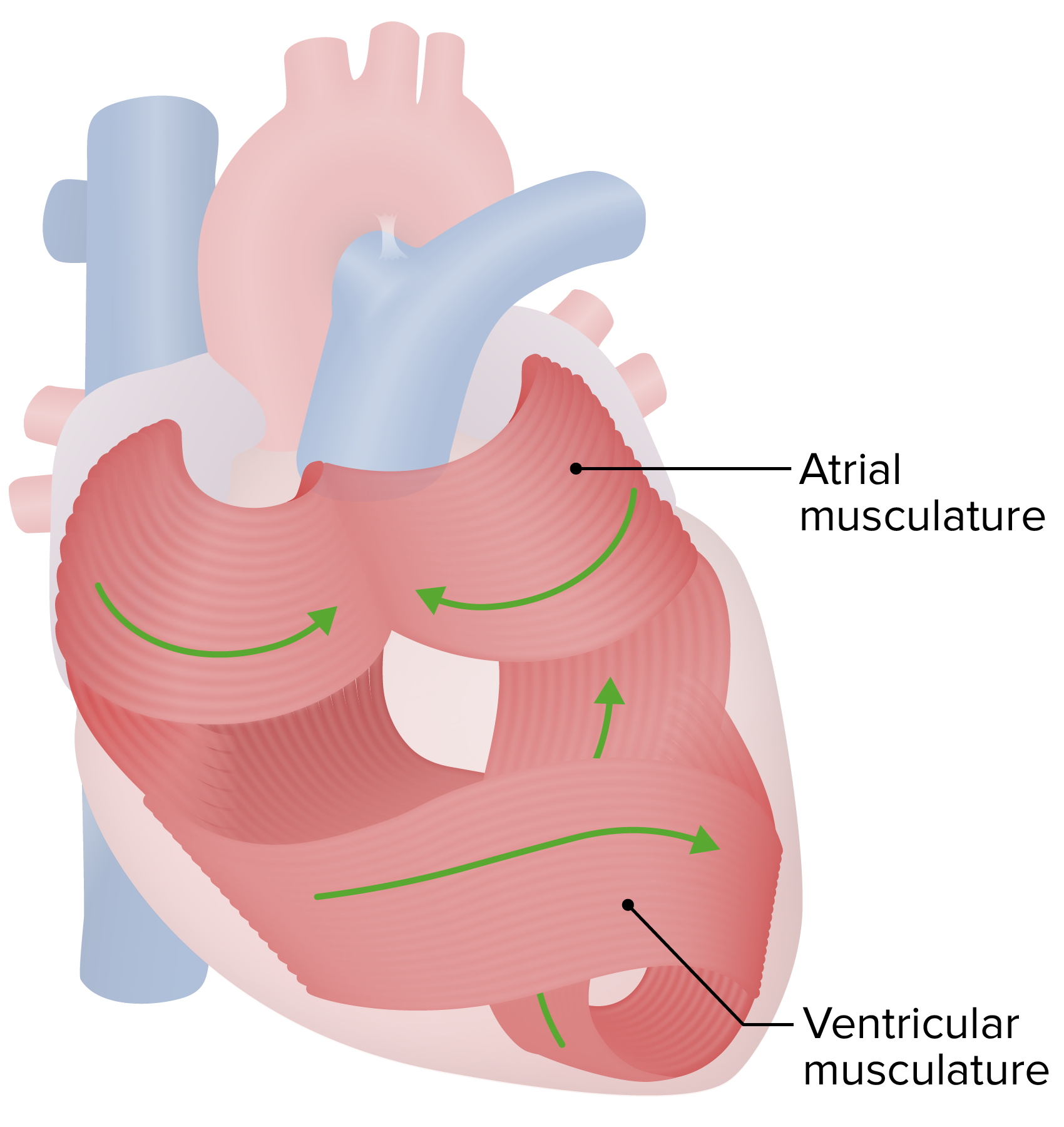
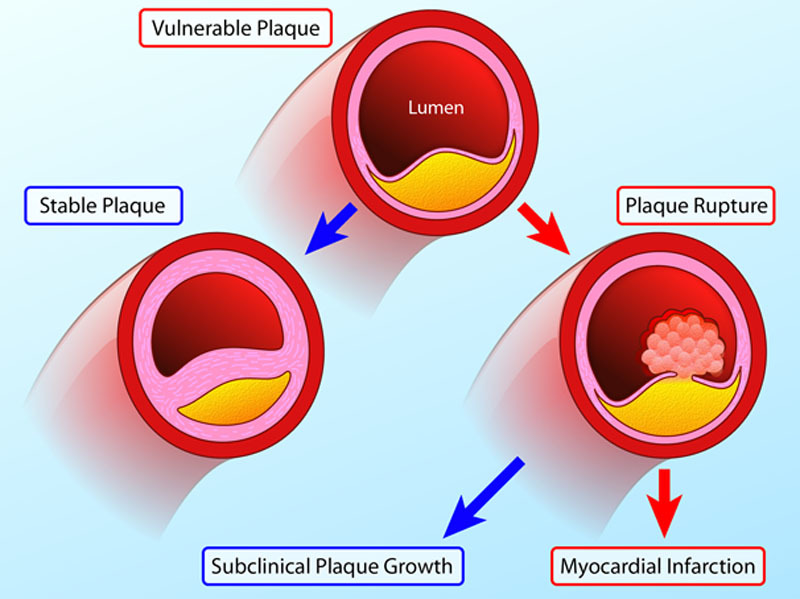
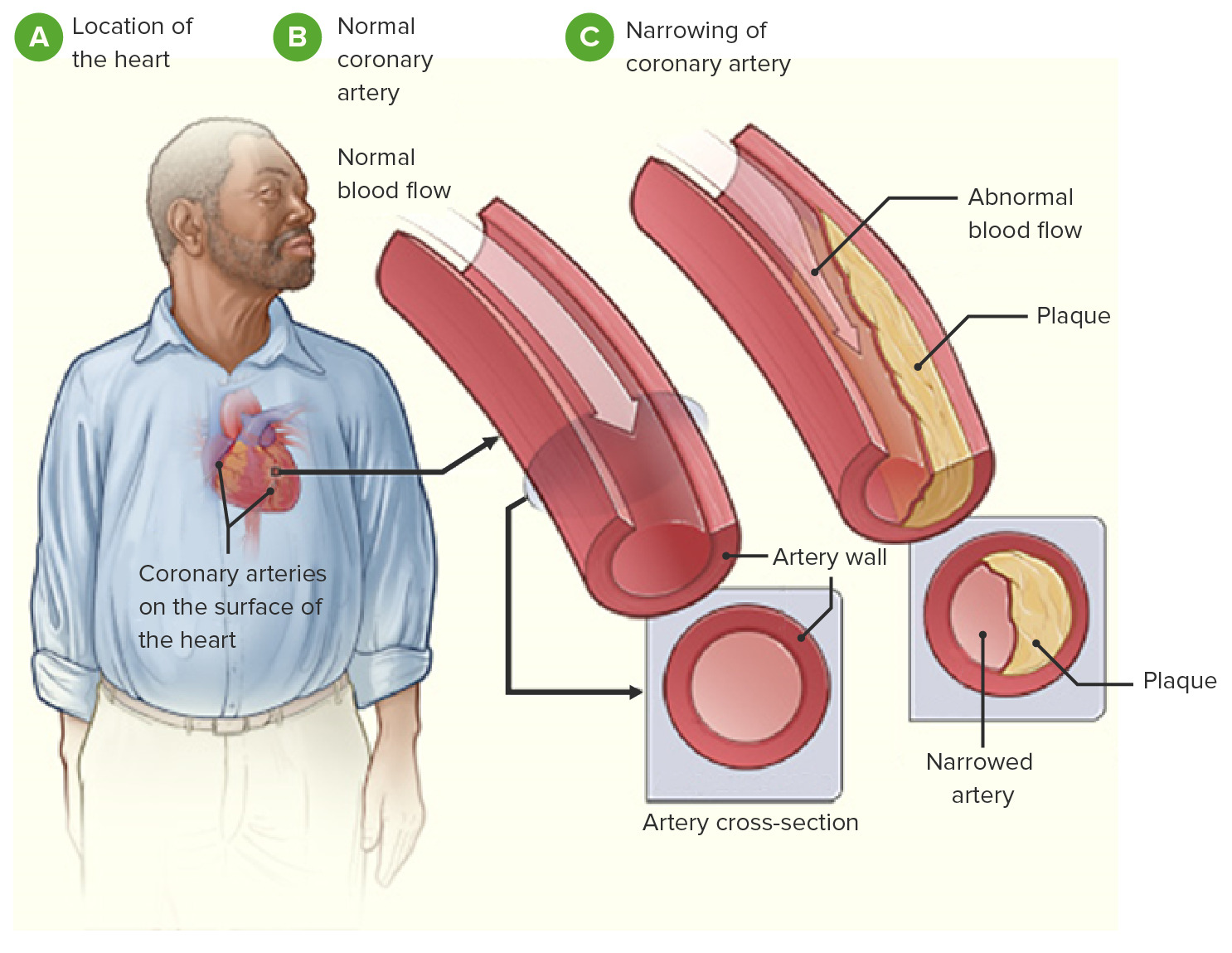
picture for heart patho
By flora g. on 21. October 2020 for Management of Angina and Myocardial Infarction: Treatment and Complications after (N)STEMI
having more pictures when explaining the heart will be better to understand.
excellent
By rosemarie m. on 29. May 2020 for Ischemic Heart Disease: Basic Principles with Carlo Raj
Carlo is an excellent teacher- he is thorough and ensures we get the concept.
Best lecturer on here
By Jack B. on 24. February 2020 for Management of Angina and Myocardial Infarction: Overview
His mannerisms and power-speaking sometimes detract from his lectures, but Dr Raj is by far the best lecturer on Lecturio.
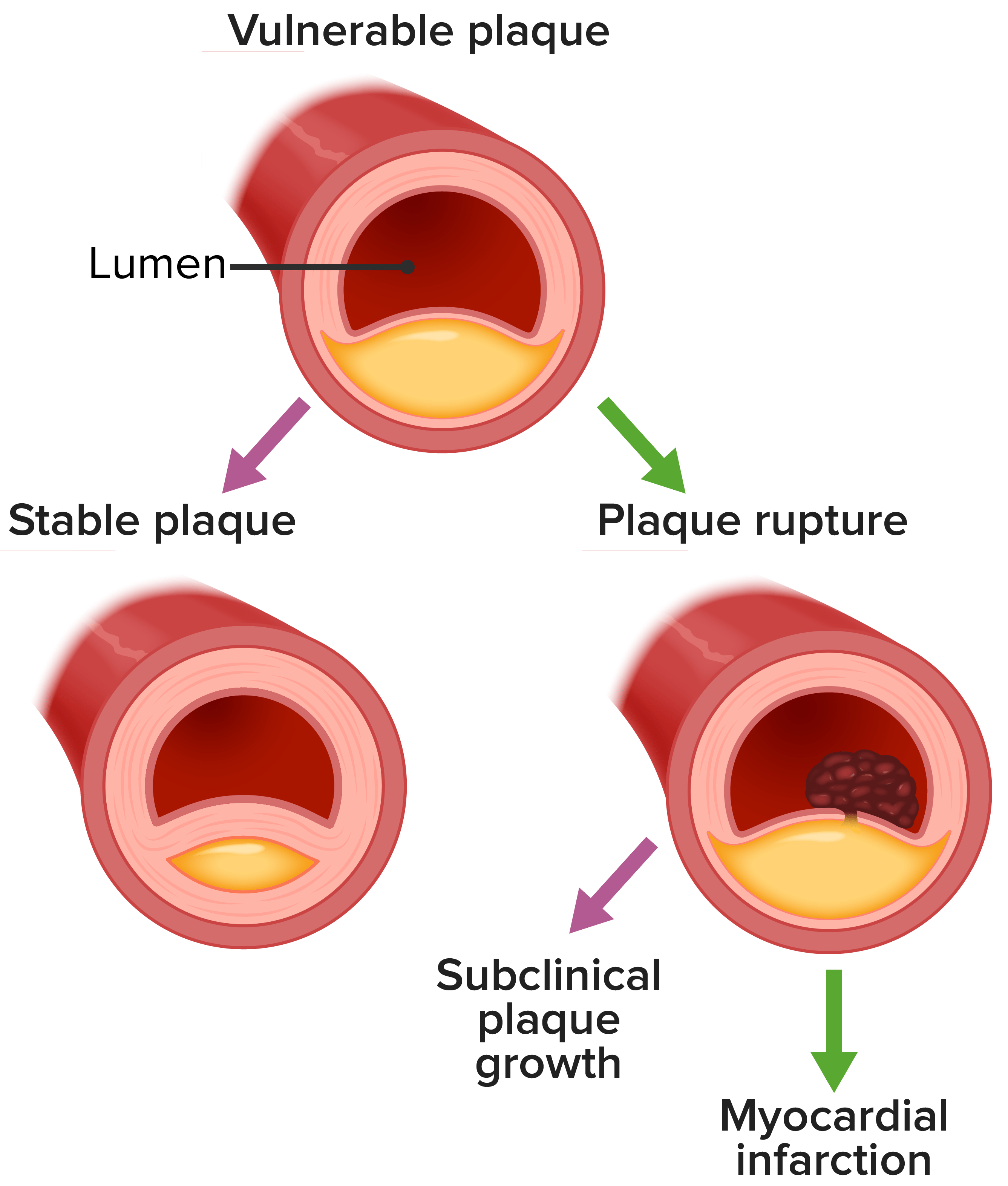
Best ACS diagram ever!
By Jack B. on 20. February 2020 for Acute Coronary Syndrome
Best ACS diagram ever! Clear, concise, and delivered with enthusiasm.
Too much
By Zeiad H. on 14. June 2019 for STEMI and NSTEMI: Special Inferior Wall Myocardial Infarction
too many information that is too advanced
slides were read not explained
thank you so mush it was helpful
By gumaa a. on 07. April 2019 for Ischemic Heart Disease: Basic Principles with Carlo Raj
thank you so mush it was helpful thank you so mush it was helpful
i like it so much . thank you
By gumaa a. on 04. April 2019 for Ischemic Heart Disease: Development
i like it so much . thank you i like it so much . thank you i like it so much . thank you
very clear and effective lessons
By samantha r. on 02. February 2019 for Ischemic Heart Disease: Basic Principles with Carlo Raj
one of the best lecturer that i have seen. thank you very much,the way he is doing easy to remember all the facts.
i am really thankful
By Yazan K. on 09. December 2018 for Ischemic Heart Disease: Basic Principles with Carlo Raj
very clear explanation that will be very beneficial in our future career . Thank you dr carlo
Great Great !!!!!!
By James A. on 19. June 2018 for Ischemic Heart Disease: Basic Principles with Carlo Raj
Much good information that will help you in your clinical practice and your board perfect combination
Best explanation & easy to understand
By Nimesh D. on 20. May 2018 for Ischemic Heart Disease: Basic Principles with Carlo Raj
Excellent explanation by dr carlo raj. I have completely understand the topic. Thanks so much to carlo raj
awesome style of teaching
By Neelam M. on 15. February 2018 for Ischemic Heart Disease: Basic Principles with Carlo Raj
fantastic teaching method, love the practical examples and slight humor, wakes you up.
Suitable for MBBS
By Alaa Q. on 13. February 2018 for Ischemic Heart Disease: Basic Principles with Carlo Raj
I would like lectures with more informations suitable for post graduate study
Great lecture, First Aid explained!
By Sandra F. on 15. January 2018 for Ischemic Heart Disease: Development
Very good lecture about the MI chronology. The Professor explains very well what we can read in "First Aid".
Very inciteful
By Tosin I. on 24. December 2017 for Ischemic Heart Disease: Basic Principles with Carlo Raj
Always inciteful with the eminent Dr Carlo Raj. It brought very much understanding of the topic
Good and clear presentation
By omar A. on 10. December 2017 for Ischemic Heart Disease: Basic Principles with Carlo Raj
Good and clear and Quick presentation. After d’avancement on futur vidéos i can beter express
The highest yield and largest amount of information But
By Hany S. on 19. August 2017 for Ischemic Heart Disease: Basic Principles with Carlo Raj
In general, great deal of high yield information with god connection to other pathologies or other specialities of the same pathology.
The problem is that sometimes those connections are not going smooth but like jumps leading to distraction and may be difficult to follow.Using techniques like light pointer or shading ,.... could be helpful .
Thanks a lot Lecturio.Thanks a lot dr Carol Raj
cool.
By Mino K. on 22. July 2017 for Ischemic Heart Disease: Basic Principles with Carlo Raj
great lecture.
repearting important thing again and again.
lecture looks like static but it is not.
He actively ask something and waiting your thought to help you understand.
Interesting!
By Yunior M. on 27. June 2017 for Ischemic Heart Disease: Basic Principles with Carlo Raj
Excellent video! I like how Dr Raj explains every detail. Perfect source to learn!
Good review of IHD
By Sterling H. on 18. May 2017 for Ischemic Heart Disease: Basic Principles with Carlo Raj
Clear and concise. Dr Raj has an engaging and interactive method of lecture that helps make this topic much easier to understand.
Easy to understand
By Lê N. on 03. May 2017 for Ischemic Heart Disease: Basic Principles with Carlo Raj
He repeats stuff a lot (in a good and memorable way) which makes me remember and understand the lesson easily. Plus he has good sense of humor!
Not helpful and makes even the most comprehensible topic difficult to understand
By Emanuele D. on 02. March 2017 for Ischemic Heart Disease: Basic Principles with Carlo Raj
"Now once this patient is giving you such a history, what would you want to give that patient automatically? You give this patient something in which there is going to be relief from the chest pain. Correct? What does that mean to you? It means underneath the tongue anytime that there's chest pain, you place nitroglycerin correct? Sublingual."
I'm sorry, and i really don't want to sound rude, but this is not how a professional teacher should speak. When i hear this i just get very confused, and i already have my teachertoconfuse me. Dr. Raj use this rethorical questions all the time and they're very annoying. What i like about lecturio's lessons is the fact that almost all the teachers use very easy sentences when they speak, and they use a lot schemes and pictures to be more clear.
Excellent source to study and preparation for USMLE
By Ashwani B. on 17. February 2017 for Ischemic Heart Disease: Basic Principles with Carlo Raj
Like it very much for education purpose very good.thanls for lecturio and the whole group for this
incredible
By Derek H. on 03. February 2017 for Ischemic Heart Disease: Basic Principles with Carlo Raj
That was incredible! This just solidified everything from 2 weeks of cardio