Playlist
Show Playlist
Hide Playlist
Coronary Steal Syndrome
-
Slides IschemicHeartDisease CardiovascularPathology.pdf
-
Download Lecture Overview
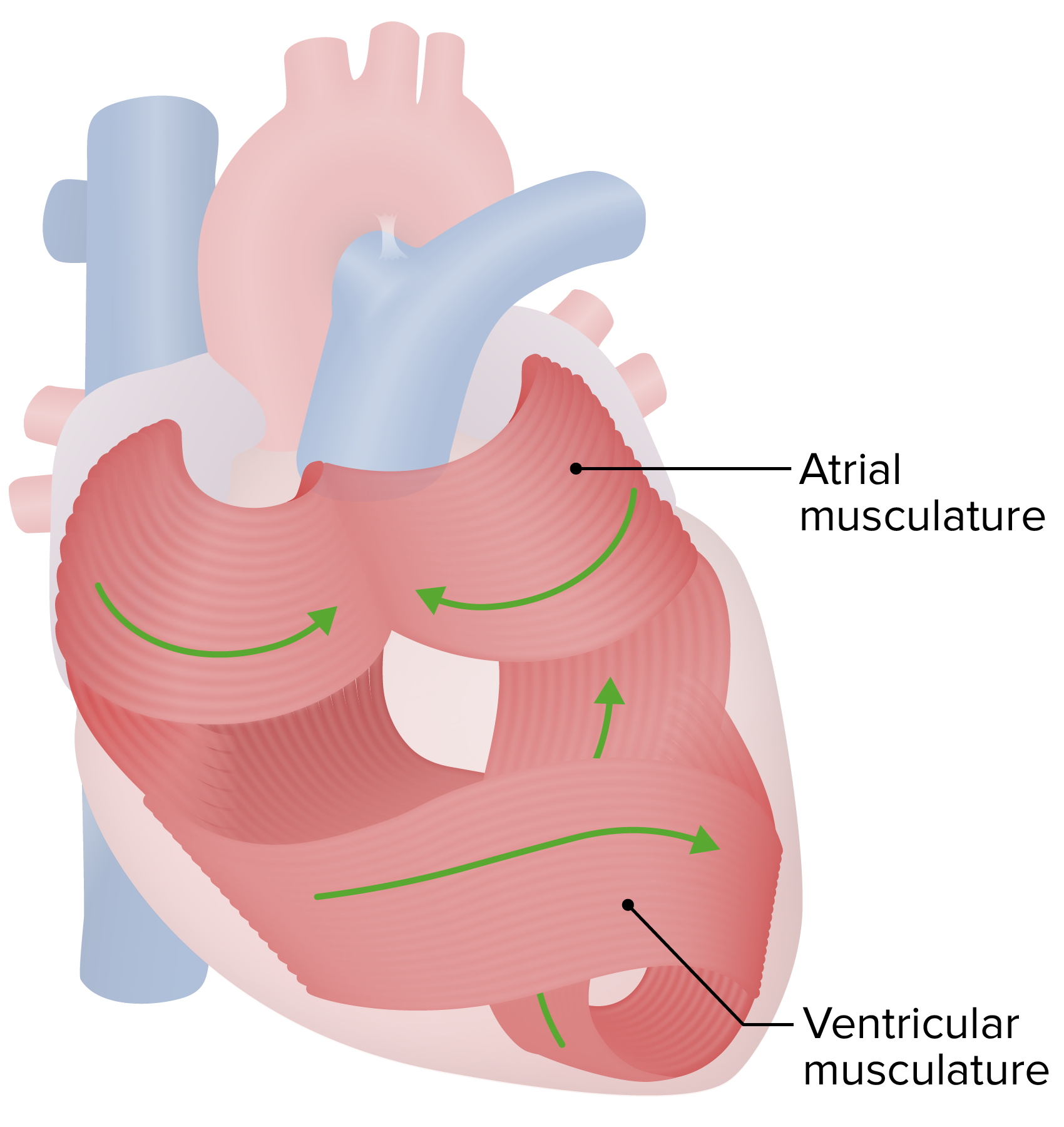
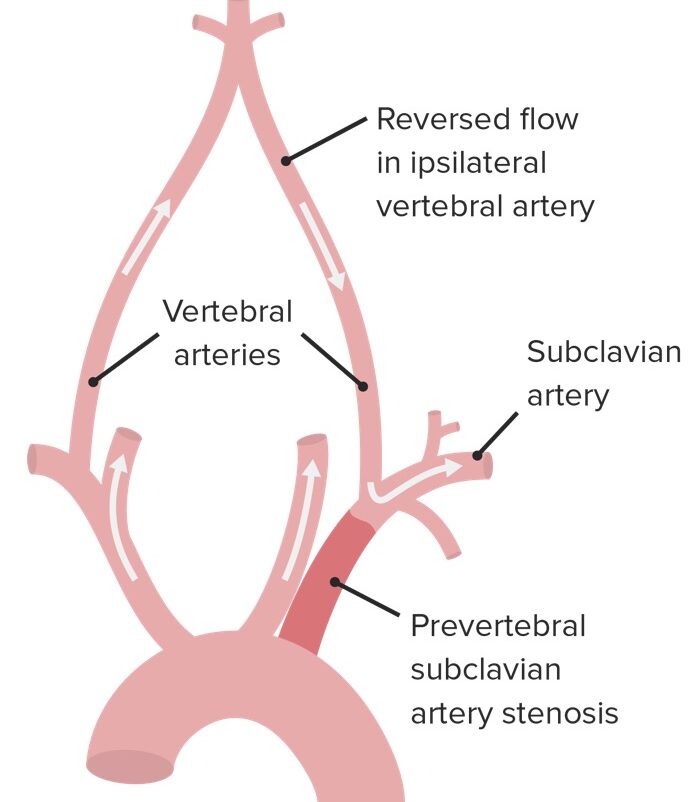
00:00 You pay attention to these tables. You are in fantastic shape. 00:00 Take a look at coronary steal syndrome now. In order for you to understand this, once again comes back to functional anatomy of the heart. Let me set this up for you. First and foremost, I want to you to come down and take a look where is this coronary vasculature. You see that. Now that is the lumen and I want you to guide and call this the left ventricular wall. Are you with me so far? Okay. So that is the left ventricular wall and where is this coronary vasculature. I need you to think of that as being a lumen of your left ventricle. 00:27 That is a chamber. So that would be the endocardium right. Now as we move superficial, we are moving towards the surface. So we are moving through the myocardium, you see where is the myocardium and then we are getting to pericardium right now. Is this picture perfectly clear to you? It should be. Next, you see where's the pericardial cavity, what is it called again? When you had sudden rupture of that ventricular wall especially when you had a macrophage degradation? It is called a left ventricle pseudoaneurysm. And what are you worried about? You are worried about rupture. 01:00 And what is that called when you have rapid accumulation of fluid in your pericardial cavity? It is called pericardial tamponade. I said that fast because we already covered that. 01:08 Okay now. In order for you to understand further, there're a couple of things that are ridiculously important. 01:14 Take a look at that coronary artery. You see that coronary artery and that is then supplying your surface of the heart. In other words, closer to the pericardium. As we move deeper down through the myocardium and then eventually to the subendocardium, understand that you are now branching into your arterioles. Okay. And the reason that this is all important to you clinically, is the fact that say that you had a coronary artery massive occlusion in which you had a MI. Okay. There is a myocardial infarction taking place at the coronary artery. 01:49 I am purposely emphasizing artery. You tell me, is that entire wall underneath the coronary artery being draped and undergoing infarction or is it only the subendocardial portion? Now, the coronary arteries supplying blood down through the branches and tributaries. 02:11 So it only makes sense that if there is coronary artery occlusion completely and a patient had myocardial infarction, then entire wall trans, what does wall mean? Mural. Transmural type of myocardium infarction would be a myocardium infarction or occlusion taking place in your coronary artery. Why is that so important to you? Because you are expected to know, on your EKG the type of ST change that you would find with the transmural type of myocardial infarction and you will tell me what kind. ST elevation or non-ST elevation. ST elevation with transmural type of infarction. Good. Take a look at arterials. You see that. Say that you had a myocardial infarction of an arteriole and it is way down by the where is this coronary vasculature and see if you had an arteriole type of occlusion, are you going to suffer from myocardial infarction? Of course you are. But then why would you call this? Not transmural but subendocardial myocardial infarction. Are we clear? How can you tell the difference. Well first and foremost, in both MIs are you going to find cardiac enzymes? Do not let that question fool you. 03:27 Of course you are. It is a myocardial infarction. What is the gold standard? One more time. 03:33 I am the most amazing medical student because you know it is troponin I. Right. So in both instances you will find a gold standard cardiac enzyme being elevated, granted. But then how can you tell the difference between transmural coronary artery occlusion versus your arteriole type of subendocardial myocardial infarction? Non-STEMI, which is an ST depression type of issue would be with your subendocardium. Coronary artery, transmural would be STEMI. We will talk about this again, but I need you to visualize the anatomy here so that you're clearly seeing as to when you are having a drape type of infarction versus subendocardial. 04:17 Next when we get into coronary steal syndrome, there are times when you might want to use certain drugs in which you might then cause coronary arteries to dilate. Okay. Now, what is that going to do? I will quickly walk you through this and then we are good to go. And then in the next couple of slides, then the information is all here. I need you to listen to me right now. Listen first, then see. Now you give a drug that is going to cause immediate vasodilation and why would you want to do this in a patient? Well your patient has something like stable angina, and what is stable angina? What do you know about the atherosclerotic plaque? Rather minimal and the pain occurred when? During exertion. Now you tell me, when you exercise from physiology, what kind of factors then have on your blood vessels when you have exercise? Obviously when you exercise, all of your muscles require greater amounts of oxygen. So just by sheer common sense, what then happens to your blood vessels? They are going to dilate. They have to. Why in the world would you want your blood vessels to constrict when your exercising? That wouldn't mean that you are supplying more oxygen. Is that clear? "But Dr. Raj, I thought exercise meant sympathetic?" Of course it does. I'm not saying that it doesn't. But when you exercise, you … that it cannot be strictly sympathetic activity on your blood vessels because that would cause vasoconstriction and it would defeat the purpose of supplying oxygen to a skeletal muscle or your heart muscle. 05:47 So then you have certain metabolites. What are those metabolites called? ATP stand for adenosine triphosphate. What kind of effect does adenosine have on your blood vessels? Vasodilate. What about lactic acid? Vasodilate. What about carbon dioxide? Where is carbon dioxide coming from? What happens to amount of carbon dioxide production with exercise? Increase, doesn't it? Of course it does. You have more glycolysis, more TCA cycle from biochemistry, releasing more carbon dioxide. All those are vasodilatory metabolites on your blood vessels. Is that clear? So my point is this when you induce stress, let us say that it is going to be physical stress with the patient with stable angina, you are trying to then create an area where you have increased coronary artery dilation, so that that area where it's undergoing your occlusion feels the pain. Are you feeling the pain right now? I hope not. If not, go to the doctor right now, but point is this. If the patient is feeling pain doing exercise, then you know you can find ST depression and such. You know your patient has stable angina. Can you mimic this medically? Of course again exactly what we just did. Instead of exercise, why not replace it with a vasodilator such as adenosine or its analog that exactly what you want to do. And when you do so, you cause your coronary artery to then dilate, it will then steal the blood from the area where it is stenosed, to your coronary artery, which is now open and what is your patient is going to feel? Pain. Clear? Now other drugs that you might want to use including dobutamine as well in which it's a chemical stress test. But understand the concept of coronary steal syndrome please. Here you will find your two different types of myocardial infarction. You will find your subendocardium, which will be arteriolar type of MI versus transmural. What kind of coronary artery or arteriole? It will be a coronary artery, transmural.
About the Lecture
The lecture Coronary Steal Syndrome by Carlo Raj, MD is from the course Ischemic Heart Disease: Basic Principles with Carlo Raj.
Included Quiz Questions
What is the typical ECG finding in a patient with an acute transmural infarction?
- ST segment elevation
- ST segment depression
- Prolonged PR interval
- J wave
- Left bundle branch block
What is the usual ECG finding during an acute subendocardial infarction?
- ST segment depression
- ST segment elevation
- Prolonged PR interval
- Left bundle branch block
- Pathologic Q waves
Which lab value is the gold standard in the diagnosis of myocardial infarction?
- Troponin I
- AST
- LDH
- Myoglobin
- Creatine kinase-MB (CK-MB)
Which of the following types of medications can pharmacologically induce coronary steal syndrome?
- Vasodilators
- Calcium channel blockers
- Beta blockers
- Epinephrine
- Amiodarone
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
He's just brilliant, and I'm so engaged and interested. He's making me love Cardiology!