Playlist
Show Playlist
Hide Playlist
STEMI and NSTEMI: Signs and Symptoms
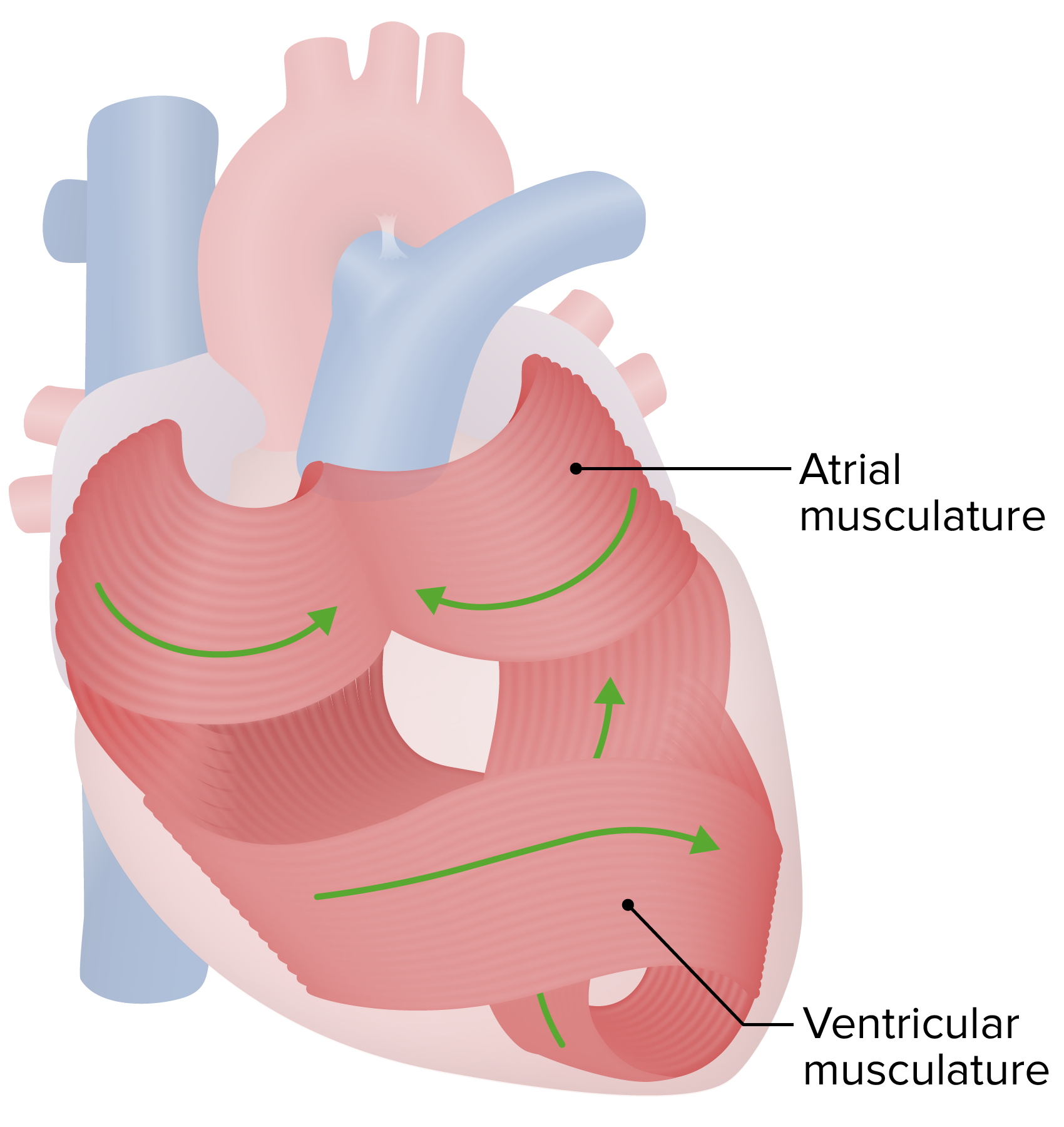
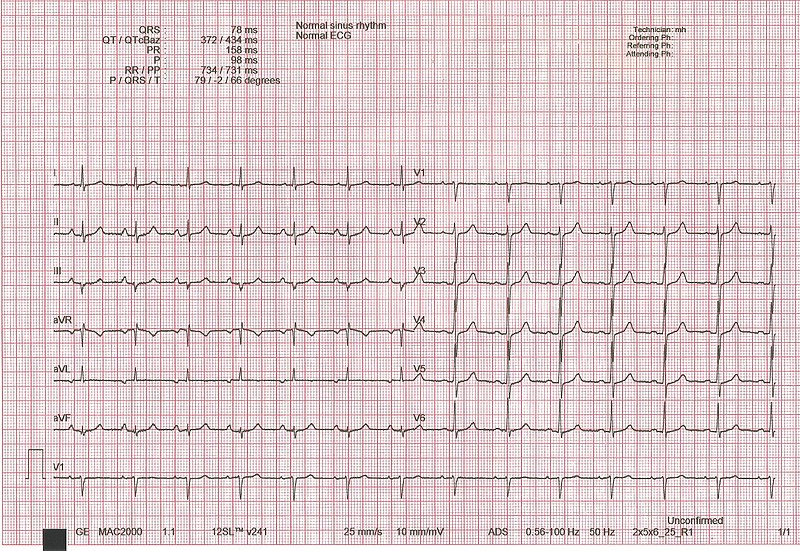
00:01 The patient with pain here would be once again substernal, may be pressure sensation. That is how they would describe it if they were to feel the pain. Why do we say if? Because can you have a patient who has a silent MI? Of course, what may happen then? Well how did that occur? It is the fact that the nerves has been shot, maybe there was diabetes mellitus resulting in diabetic neuropathy. And so at that point, the nerves are not able to properly feel the pain and that is very scary and you know for a fact the patient with diabetes has what? Increased VLDL, which contains triglyceride and this may then accumulate in your blood vessels. The pain, how long does it last? Approximately 20 minutes to hours, but it is not a fleeting pain. Versus what? Versus your anginas. Remember in exertional. It was exactly that exertional, stable. Unstable, maybe about 30 minutes, even at rest. But eventually, remember that is not an MI. This is, so we will find cardiac enzymes. It radiates to the neck, jaw and arm and associated with diaphoresis, right. 01:12 Physical examination, your sympathetic activity has kicked in once again. If your heart is beginning to die, it decreases your cardiac output because it's refers to as being what? Cardiogenic shock. If it is a cardiogenic shock, then what branch of the autonomic nervous system is going to be stimulated? The sympathetic nervous system. If it is the sympathetic nervous system, it is doing everything in its power to restore heart function, isn't it? It may then function on your beta-1 receptors excessively resulting in tachycardia. Now if there is enough damage taking place with the heart, at some point, the left ventricle becomes large. Pay attention here, please. So now, the left ventricle becomes enlarged, association with CHF, congestive heart failure from AMI, acute myocardial infarction. Whenever there is congestive heart failure, I want you to think about the heart sounds that we will discuss. And when we do in great detail, then you know that S1 is the closure of what? Mitral and tricuspid in that order. S2 is the closure of what? Closure of aortic, pulmonic in that order. And when does your aortic valve close? I want you to pay attention to aortic valve right now, specifically. It closes doing diastole, doesn't it? Yes, it does. If it closes during diastole, then what then opens? Mitral valve. Are you with me? If you don't, make sure that your physio is strong here. See the only way that you are able to properly understand this and this information will never leave you because it is a permanent part of your heart and brain and soul. So now the mitral valve opens and this left ventricle is rather large and I will say this blood is rushing into the left ventricle, are you here? Stay with me. The blood is rushing into the left ventricle. Are you going to create a heart sound? Of course, you are. What is this called? S3 gallop. You’re with me? And that's why S3 comes after S2. S2 is a diastolic type of heart sound because that is the only time that you have aortic, pulmonic valve closure. Subsequently thereafter, the mitral valve is then going to open during diastole and if you have a large ventricle, you are going to create an S3. Pulmonary rales may be present, why is that? While let us go backwards, mean to say that earlier we just talked about S3 and if the heart is not able to move forward because of acute myocardial infarction, then perhaps there might be congestion. If there's congestion is taking place from the left ventricle, then you are going to back up into where? Good, left atrium. After that what are you going to back up into? The pulmonary veins. 03:58 And then where are we going to back up into? Increased hydrostatic pressure in the pulmonary capillaries may result in pulmonary rales. A new systolic murmur due to papillary muscle rupture, is that a complication that could occur? Of course. Worse case scenario, what if there is a ventricular septal rupture? May result in something like a VSD perhaps and when you have that type of rupture, my goodness, you are worried about things like cardiac tamponade especially if it is a ventricular wall rupture. So that rupture be careful, please. This is ventricular septum and here we are looking at physical findings of new systolic murmurs. You should know already that VSD is the systolic murmur. On EKG. Now here let put things together I have repeated this. I have introduced this already to you. Let's just make sure that we are clear about what kind of EKG changes you are expected to see, please focus upon transmural MI. We have a peaked, a hyperacute T-wave. Next, ST elevation. That by far is the most important point. The ST elevation is found with transmural. Once again you tell me what kind of coronary blood vessel, an artery or an arteriole? You answer that question. Artery, right. And if you have that picture anatomically once again you will remember that as soon as the artery has been occluded, there is complete draping of infarction over the entire transmural tissue. 05:31 There is something called Q-waves and I am not going to focus upon that so much, but it if the fact that normally the Q-wave, at least, tell me this. What is a Q-wave? Is it a negative or positive deflection? It is a negative deflection. It is the first negative deflection that you would find in normal EKG. If you find that Q-wave to be exaggerated in terms of its negativity, that is referred to as being your Q-wave. Just keep that in mind. It doesn't mean that it is absent. It just means that it might be exaggerated especially if it is a chronic type of MI. Let us continue. ST segment elevation is the classic infarction pattern and this is what you have to pay attention to. If it is greater than 1mm, which is one box, remember dissecting an EKG and what a box means to you? So that one box whether 1 mm in 2 or more contiguous leads, by definition an ST elevation. What about an EKG and its T-wave? Now it could be peaked or it could be inverted. The development of new Q-waves then indicates a transmural MI. What that means is that they are usually part of late finding in AMI. Your focus right now, should be on ST elevation. Once you have understood that and if you have got that firmly embedded, then you move on to take a look at these other waves that are relevant when dealing with acute myocardial infarction, transmural type. MI here new conduction system abnormalities and that we have already known. Whenever there is a myocardial infarction, my goodness you are now compromising the conduction systems. 07:09 So, therefore, you are introducing what? New types of arrhythmia. There might be a new left bundle-branch block and how do you know that on your example? What would they give you? A left bundle-branch block. Now close your eyes and think of the following. We have bundle branches. So you have just moved from your AV node through the bundle of His and you are moving through your interventricular septum, are you not? Are you there? Good. Now you have a left bundle branch and a right bundle branch normally. Now you tell me what is it that permits the aortic valve to close? Don't you need a depolarization event? And so, therefore, the left bundle branch is going to depolarize first, always physiologically, so that the aortic valve closes and then followed by the right bundle branch and the pulmonic valve. Is that clear? We have A2, P2, collectively what heart sound please? The second heart sound, good. Now, what if there is a left bundle-branch block, what happens? It means that you have decreased conduction through the left bundle branch, yes. So does that mean that you have conduction passing the right bundle branch? That is exactly right. So that results in what kind of split? Paradoxical split, excellent okay. EKG changes maybe there is a left bundle-branch block resulting in a paradoxical split of your second heart sound.
About the Lecture
The lecture STEMI and NSTEMI: Signs and Symptoms by Carlo Raj, MD is from the course Ischemic Heart Disease: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following is the most likely explanation for pulmonary rales following a myocardial infarction?
- Backup up of blood into the pulmonary veins from the left atrium resulting from a weakened left ventricle
- Backup of blood into the pulmonary arteries from the right atrium resulting from a weakened left ventricle
- Backup of blood into the pulmonary arteries from the left atrium resulting from a weakened left ventricle
- Backup of blood into the pulmonary veins from the right atrium resulting from a weakened right ventricle
- Backup of blood into the pulmonary veins from the right atrium resulting from a weakened left ventricle
ST-elevation myocardial infarction is characterized by which of the following ECG findings?
- New ST-segment elevations with a magnitude of greater than 1 mm in two or more contiguous leads.
- New ST-segment elevations with a magnitude of greater than 16 mm in all leads.
- New ST depressions in all leads.
- New ST segment elevations with a magnitude of less than 1 mm in three leads.
- Diffuse ST depressions and Q waves.
Which physiological heart sound occurs at the start of diastole and what does it represent?
- S2, indicating closure of the aortic and pulmonic valves
- S1, indicating closure of the mitral and tricuspid valves
- S3, indicating closure of the aortic and pulmonic valves
- S2, indicating closure of the mitral and tricuspid valves
- S1, indicating closure of the aortic and pulmonic valves
Which of the following heart sounds most likely indicates a dilated left ventricle?
- S3
- S1
- S2
- S4
- Opening snap
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |