Playlist
Show Playlist
Hide Playlist
Blunt Cardiac Injury, Esophageal Injury, Diaphragmatic Injury
-
Slides ThoracicInjuries Surgery.pdf
-
Download Lecture Overview
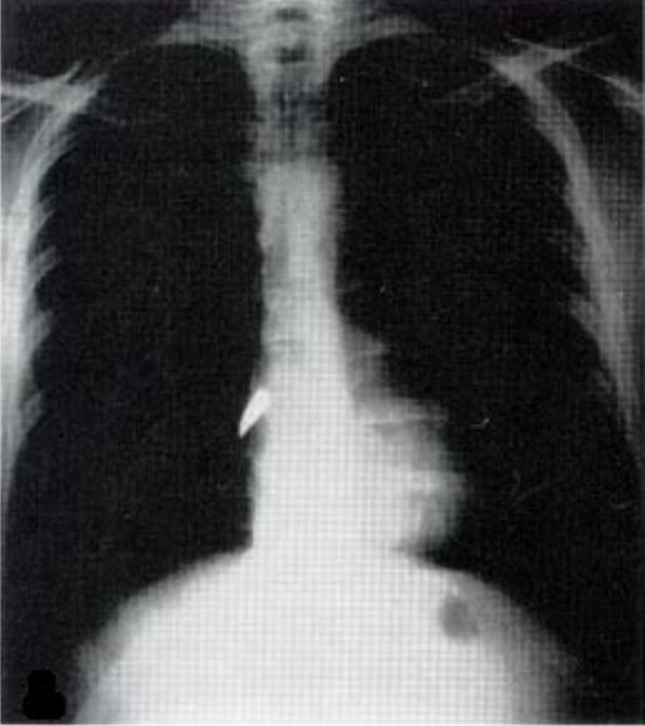
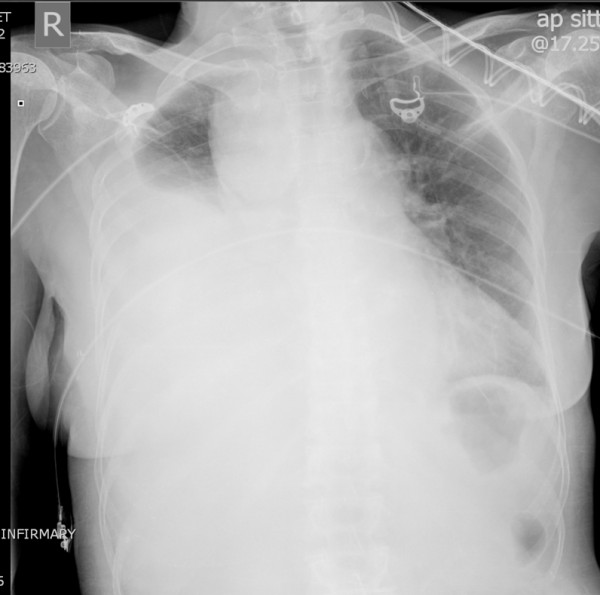
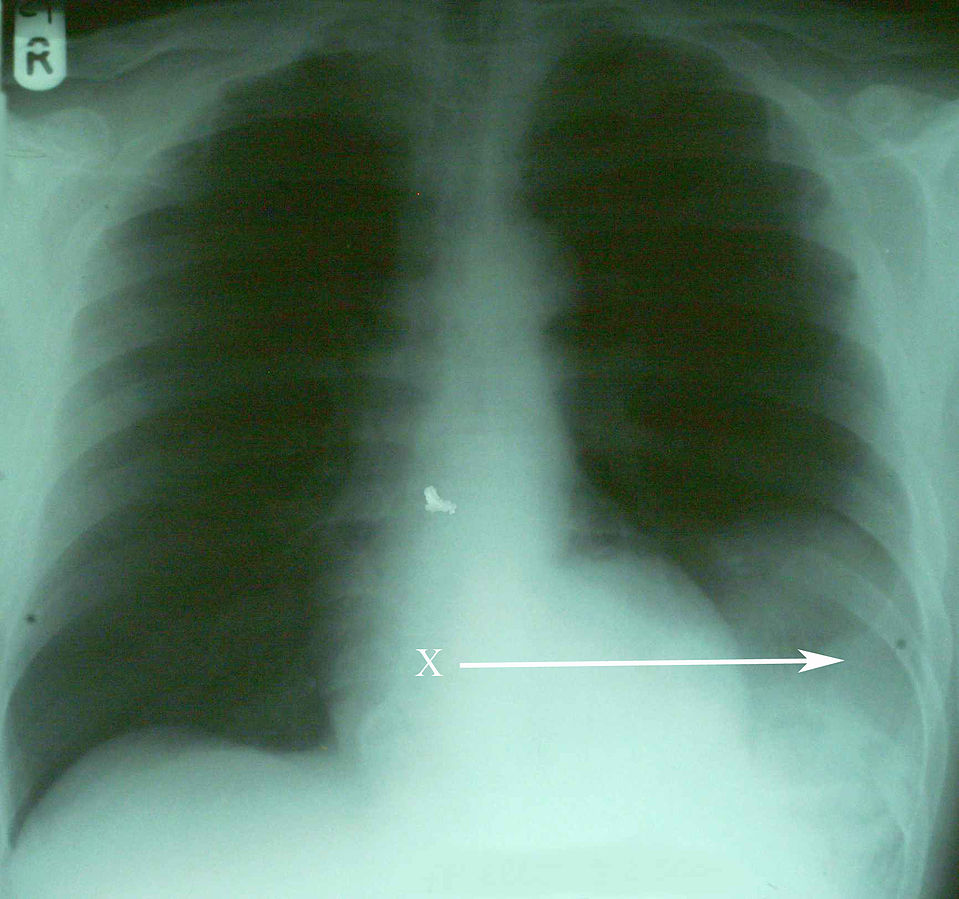
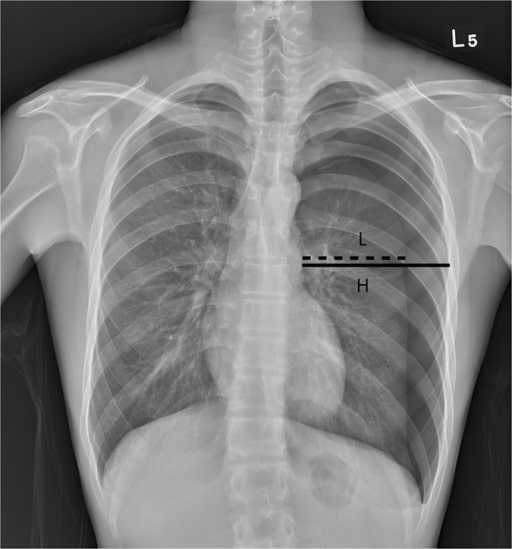
00:01 Now, let's move on to a different clinical scenario. 00:05 Let's say the patient now is a 60-year-old man who sustains a head-on collision and there's deformity of the steering wheel and there was airbag deployment. 00:14 The patient is conversant and is orientated at the scene with a normal blood pressure, but he complains of severe breastplate pain. 00:23 What injuries are you suspecting at this time having received this report? I'll give you a second to think about it. 00:32 Your differential diagnosis should include a sternal fracture, sure. 00:36 As the airbags are so important savings lives, however, the force at which it deploys can often cause sternal fractures. 00:46 And of course, myocardial injury, also known as blunt cardiac injury. 00:52 We used to call this cardiac contusion, but we don't call it that anymore because it's clearly a spectrum of diseases. 01:00 Let's start with sternal fractures. 01:02 Here on this cross-sectional CT chest, you notice that the sternum is fractured. 01:07 Again, sternal fractures in and of themselves are not so important. 01:10 They cause pain and the patient can splint. 01:12 So you want to make sure the patient has adequate pain control. 01:16 I remember, sternal fractures can be difficult to diagnose and appreciate on plain x-rays particularly if they have had previous cardiac surgery like our patient and has sternal wires. 01:26 Now, let's discuss blunt cardiac injury. 01:29 It's similar to patients who develop multiple rib fractures and underlying pulmonary contusion. 01:35 The right ventricle is particularly susceptible injury because it's so close to the sternum and the surface that is exposed to injury is far bigger than any other chamber. 01:49 Here, we get an EKG or 12-lead EKG on our patient suspected of blunt cardiac injury. 01:54 It's important to remember, however, the severity of the sternal fracture or even the presence of the sternal fracture does not actually indicate that the patient is more likely to have a blunt cardiac injury. 02:06 Here on this EKG, take a look at it. 02:09 You can pause the video, and see that there are 1 millimeter ST segment elevations in the lateral leads with associated right bundle branch block. 02:17 All concerning for blunt cardiac injury. 02:21 If you decide that the patient in fact is at risk or has blunt cardiac injury, either diagnose with EKG abnormalities or a rise in the troponin level, the patient should be admitted and watch by telemetry. 02:34 However, if the EKG is completely normal and the troponins are negative, usually the patient can be sent home as long as they don't have any other injuries. 02:44 Should we get any additional studies for blunt cardiac injury? Well, like I said if there's any hemodynamic instability, go ahead and get an echo, take a look at whether or not the right ventricular function is normal. 02:55 In the absence of hemodynamic instability, it's usually not very helpful. 03:02 Now, quiz time. 03:04 Take a look at this image. 03:05 What's wrong with that? The hints are in the white arrows. 03:09 I'll give you a second to take a look at this. 03:15 That's right, the patient has a widened mediastinum and anytime you see a widened mediastinum in a trauma patient, you should have concern for aortic injury. 03:27 In this 3D reconstruction of the aortic anatomy, you see the results of an endovascular repair of a traumatic pseudoaneurysm. 03:34 Nowadays, endovascular repair of the Type B dissection involve the descending aorta is very popular and supplanting left thoracotomies and open procedures. 03:42 However for Type A dissection sternotomy and open repair is the standard. 03:50 Let's pose a question. 03:52 In the scenario where a patient presents to the trauma bay is hypotensive and demonstrates a widened mediastinum, what's your next step in management? I'll give you a second to think about it. 04:04 Of course, ABCs. 04:05 I know it seems silly, but you get the point. 04:08 We always start with airway, breathing, circulation, but very importantly, the take-home message here is this. 04:14 For circulation, it is very unlikely that a widened mediastinum is actually the cause of hypotension. 04:20 Therefore, you have to go look for other sources of bleeding. 04:26 And the answer is an eFAST. 04:28 We'll get to that in a little bit. 04:31 Remember, any time you have a hypotensive patient statistically speaking, it's bleeding until proven otherwise. 04:41 Let's move on a little bit. 04:43 Here, also in the thorax of course is the esophagus. 04:46 Esophageal injury is demonstrated by CT scans is usually indirect findings and the most common indirect finding is a mediastinum that has air or called a pneumomediastinum. 04:58 By the time you have dysphagia or pleural effusion, it's usually a late finding. 05:03 High index of suspicion is very important. 05:05 And of course, if you have a knife or a sword stab wound to the chest, you have to consider esophageal injury as a possibility. 05:12 Given pneumomediastinum and a mechanism that suggests that there may be either a tracheal or esophageal injury, patients undergo what's called a triple scope. 05:22 They include bronchoscopy to look at the major airways, esophagoscopy to look at the esophagus. 05:31 This is typically done in a rigid fashion as opposed to an EGD, which is a flexible scope that goes into the stomach and duodenum. 05:39 And lastly, a laryngoscopy to evaluate the upper airway. 05:43 Here, you see an image of the vocal cords. 05:47 Now, some important esophageal injury principles. 05:50 Remember, esophageal injuries are associated with other mediastinal structures. 05:55 That's where we get 3 scopes. 05:57 If you have an esophageal injury, you may also have a tracheal injury. 06:01 Early repair is preferred if you identify it. 06:04 That's because if it's delayed in terms of diagnosis, the patient may become septic. 06:09 Review the septic lecture module for more information. 06:16 Now, let's move on to our favorite test topic which is the diaphragmatic hernia. 06:22 Diaphragmatic hernias are difficult to diagnose. 06:25 And once again, it's one of those entities where you need to have a high index of suspicion. 06:29 Clearly, our patient has a risk of diaphragmatic injury. 06:33 In this chest x-ray that includes the upper cuts of the abdomen, this is as clear as it gets. 06:38 You see an air bubble within the left thorax, that's likely the stomach. 06:42 Clearly, the stomach doesn't belong in the left thorax. 06:45 There's only one way that happened. 06:47 There's a diaphragmatic hernia. 06:51 Now, in practice, it's rarely this clear. 06:53 Usually even with cross-sectional imaging that is high definition, it's still very, very hard to detect. 06:58 Therefore, you have to have a high index of suspicion. 07:01 And also, diaphragmatic hernia may cause respiratory distress because of the possibility of phrenic nerve paralysis. 07:10 All diaphragmatic injuries need to be repaired particularly on the left side as they're unlikely to fix themselves. 07:16 And again, to remind you, they are difficult to diagnose on x-ray or cross-sectional imaging. 07:23 Now, it's time to review some important clinical pearls and high-yield information. 07:28 Recall that any stab wound to the chest may also involve the abdomen and diaphragm. 07:33 Therefore, a high index of suspicion is necessary. 07:37 Additionally, remember the very important concept of tension pneumothorax. 07:41 It's a clinical diagnosis, hypotension, distended neck veins, and of course a clinical picture that's consistent with the possibility of a pneumothorax. 07:51 Thank you very much for joining me on this discussion of thoracic trauma.
About the Lecture
The lecture Blunt Cardiac Injury, Esophageal Injury, Diaphragmatic Injury by Kevin Pei, MD is from the course Surgery: Trauma. It contains the following chapters:
- Differential Diagnosis
- Blunt Cardiac Injury
- Esophageal Injury
- Diaphragmatic Injury
Included Quiz Questions
Which of the following conditions is most difficult to diagnose on plain radiographs and CT scans?
- Diaphragmatic injury
- Atelectasis
- Hemothorax
- Pneumothorax
- Emphysema
A trauma patient presents with a widened mediastinum seen on a chest x-ray. What are you concerned about?
- Aortic injury
- Pericardial effusion
- Cardiac tamponade
- Esophageal rupture
- Mediastinitis
In cases of esophageal injury, which of the following diagnostic methods are NOT utilized?
- Rhinoscopy
- Esophagoscopy
- Cross-sectional imaging
- Bronchoscopy
- Laryngoscopy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |