Playlist
Show Playlist
Hide Playlist
Bleeding Disorders: Platelet Count, Defects, and Factor Deficiencies
-
Slides Bleeding Disorders and Thrombotic Disorders.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
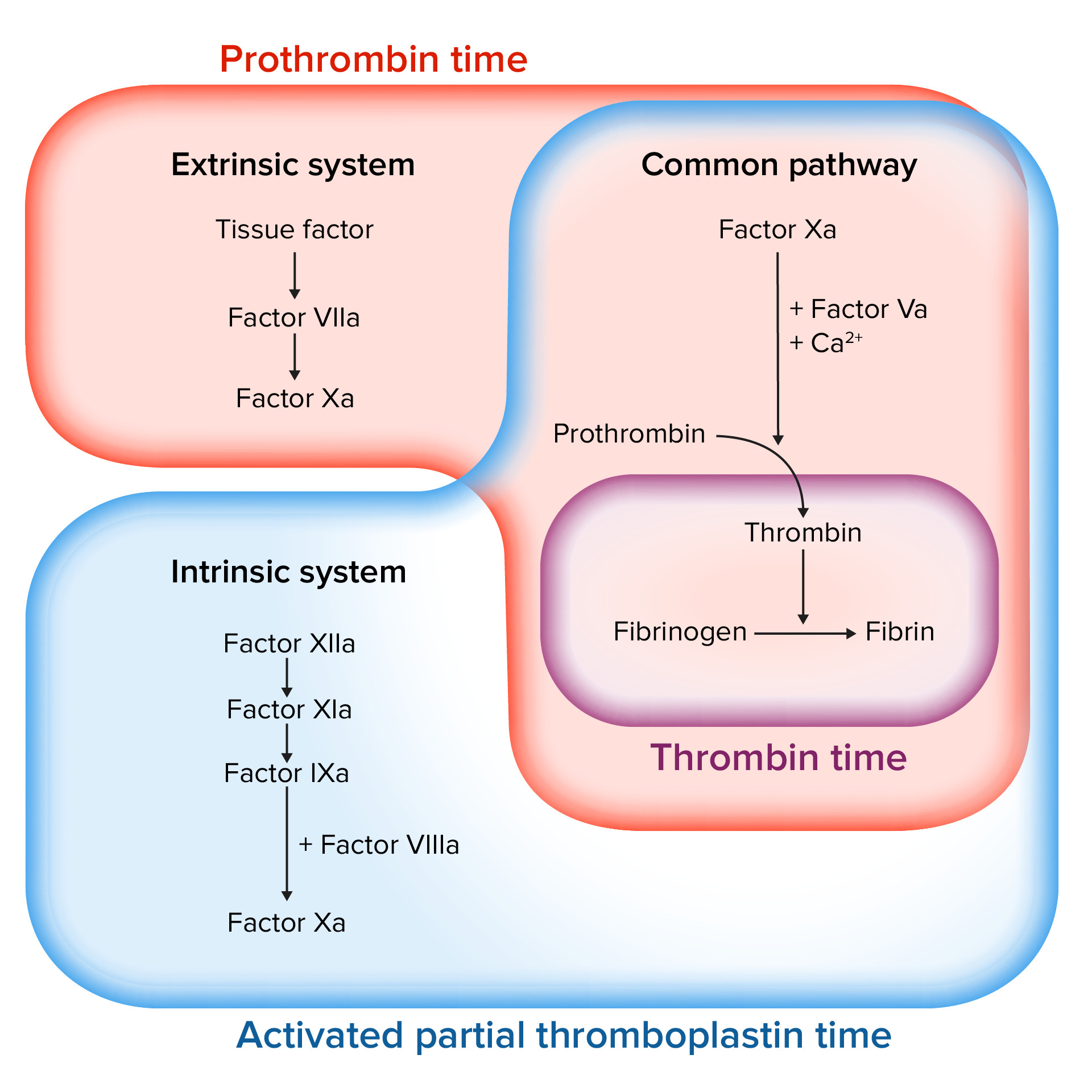
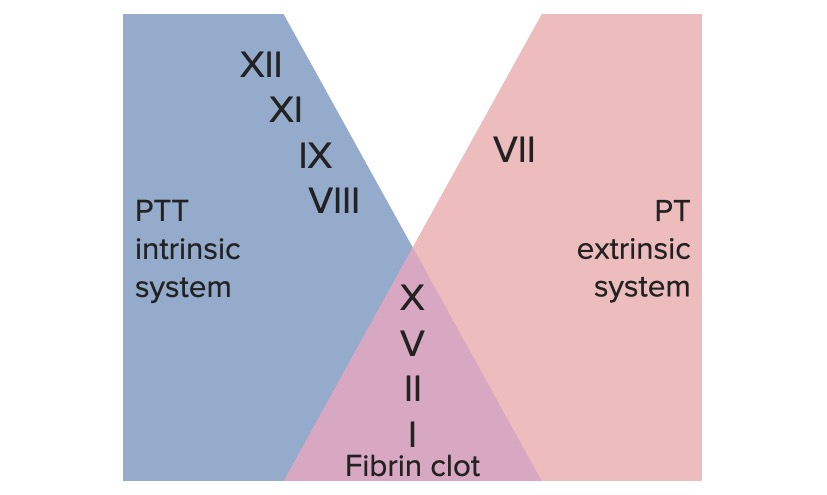
00:01 Welcome back. 00:02 So, we've talked about normal hemostasis. 00:04 We've talked about, kind of thrombosis and how that's regulated and not regulated. 00:09 Now, we're going to talk specifically, about bleeding disorders and thrombotic disorders. 00:14 So, hemorrhaging and too much clotting and flip sides of the coin. 00:19 This is where we are, in our roadmap and we've been through all the things above, including measuring clotting parameters. 00:28 Now, bleeding disorders. 00:31 So, we're going to start with platelets. 00:32 Platelets, we need to have the right number not too many not too few and the normal range is between 150,000 and 400,000 per microliter and most of us live, quite adequately within that. 00:48 You can even have normal hemostasis down to a level of 100,000 platelets, so, within that range, we're okay. 00:56 Now, if you were to traumatize yourself and you have a relatively lower amount of platelets at the 100,000 level, you might have significantly more bleeding, than if you had adequate numbers of platelets 150,000 and above. 01:11 If we start getting down into the 40,000 and less range, you can have spontaneous bleeding, into your brain into your gut into other tissues, that's potentially problematic. 01:25 At 10,000, you start having severe spontaneous bleeding. 01:29 So, it's in this range, usually around 10,000, that we will give exogenous platelets, we will do platelet transfusion, to patients who have been receiving chemotherapy or otherwise platelet deficient. 01:42 Above that 10,000 level we don't normally administer platelets, except in extreme circumstances and certainly if there's trauma and we need to stop the bleeding, we will give platelet transfusions even at levels 40,000 and above. 01:58 There are also problems related to inadequate or abnormal platelet function. 02:03 In a previous session, we talked about things like non-steroidal anti-inflammatory agents, which, will block the cyclooxygenase, that's responsible for generating thromboxane A2 and in that setting, platelets will become largely dysfunctional. 02:19 But they're also hereditary, non-acquired platelet defects. 02:25 So, let's talk about that. 02:27 Remember, that when you have an endothelial injury, a vascular injury, we will expose underlying extracellular matrix, that has deposited within it von Willebrand factor. 02:40 And one of the very first steps, in the coagulation process, is, the recruitment and binding of platelets to the newly exposed von Willebrand factor. 02:51 That interaction, requires, binding of glycoprotein Ib to von Willebrand. 02:58 Glycoprotein Ib is on the surface of the platelet, von Willebrand and the extracellular matrix. 03:03 If you don't have that, if you don't have von Willebrand factor, you have von Willebrand disease and will have bleeding. 03:10 Glycoprotein Ib, binds to von Willebrand factor, that's the other part of the equation, if you don't have glycoprotein Ib, because of a genetic deficiency, you have a disease called “Bernard Soulier syndrome.” That's not enough. 03:26 Remember, that's just your primary hemostatic plug, getting the platelets to bind to the extracellular matrix. 03:31 Now, we would like to recruit additional platelets and make a large aggregate to get a definitive secondary plug, that requires platelet-to-platelet interaction. 03:41 That's going on between GPIIb-IIIa the glycoprotein IIb/IIIa, sitting on the surface of activated platelets and then linking platelet to platelet, through fibrinogen, as the bridge between them. 03:55 That aggregation step, is completely blocked, if you have defects in GPIIb-IIIa and that disease is, "Glanzmann thrombasthenia." So, you can have a number of hereditary defects, that also will give you problems related to the primary acquisition and aggregation of platelets. 04:15 They're hereditary factor deficiencies. 04:17 So, remember that, you have platelets, you have coagulation factors, secreted mostly by the liver and we have endothelial cells, all working together in a beautifully highly choreographed dance, that leads to clotting. 04:33 You can have hereditary factor deficiencies, the most common probably overall is factor VIII deficiency. 04:40 Factor VIII and factor IX as we'll see in a second are both x-linked, so, it's much more commonly affecting men and if you have factor VIII deficiency, which is, somewhere in your common pathway, you'll have hemophilia A. 04:55 Factor IX deficiency, which is, more in the intrinsic pathway, more upstream, that would be hemophilia B. 05:02 Factor XI deficiencies are quite common, amongst Ashkenazi Jewish populations and factor XII deficiencies, are especially common, in the Asian population. 05:12 Interestingly and as we've remarked previously in one of the earlier sessions, having to do with coagulation factors, you can be completely factor XII deficient and have no problems associated with bleeding. 05:25 That's because of that crosstalk, between the extrinsic pathway and the intrinsic pathway, that completely bypasses factor XII. 05:33 And then, there are a number of other much rarer, hereditary factor deficiencies VII, II, V, and X. 05:41 So, in all those cases, we can also have bleeding tendencies.
About the Lecture
The lecture Bleeding Disorders: Platelet Count, Defects, and Factor Deficiencies by Richard Mitchell, MD, PhD is from the course Hemostasis.
Included Quiz Questions
What component is affected in the Bernard-Soulier syndrome?
- Platelet glycoprotein (GP)Ib
- von Willebrand factor
- Collagen
- Platelet glycoprotein (GP)IIb-IIIa
- Factor VIII
What is deficient in Glanzmann thrombasthenia?
- Platelet glycoprotein (GP) IIb-IIIa
- von Willebrand factor
- Platelet glycoprotein (GP) Ib
- Factor VIII
- Factor VII
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
1 customer review without text
1 user review without text