Playlist
Show Playlist
Hide Playlist
Arginine Vasopressin (AVP) Differential Diagnoses
-
Slides ActionOfADH EndocrinePathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
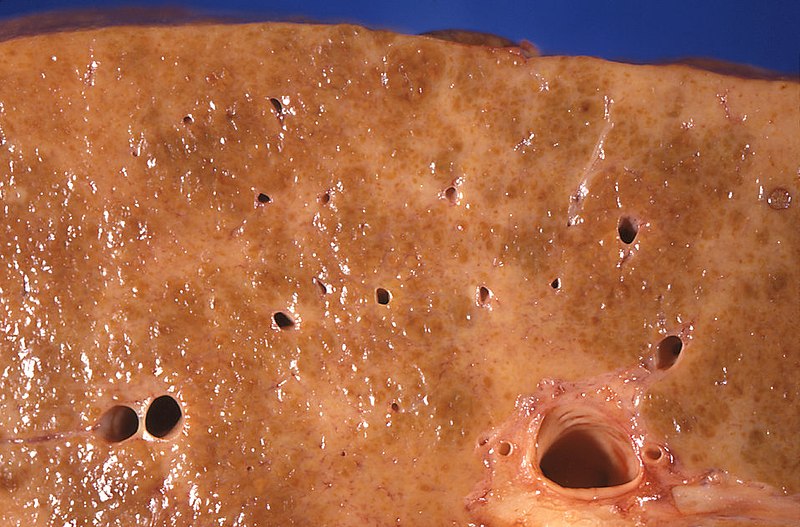
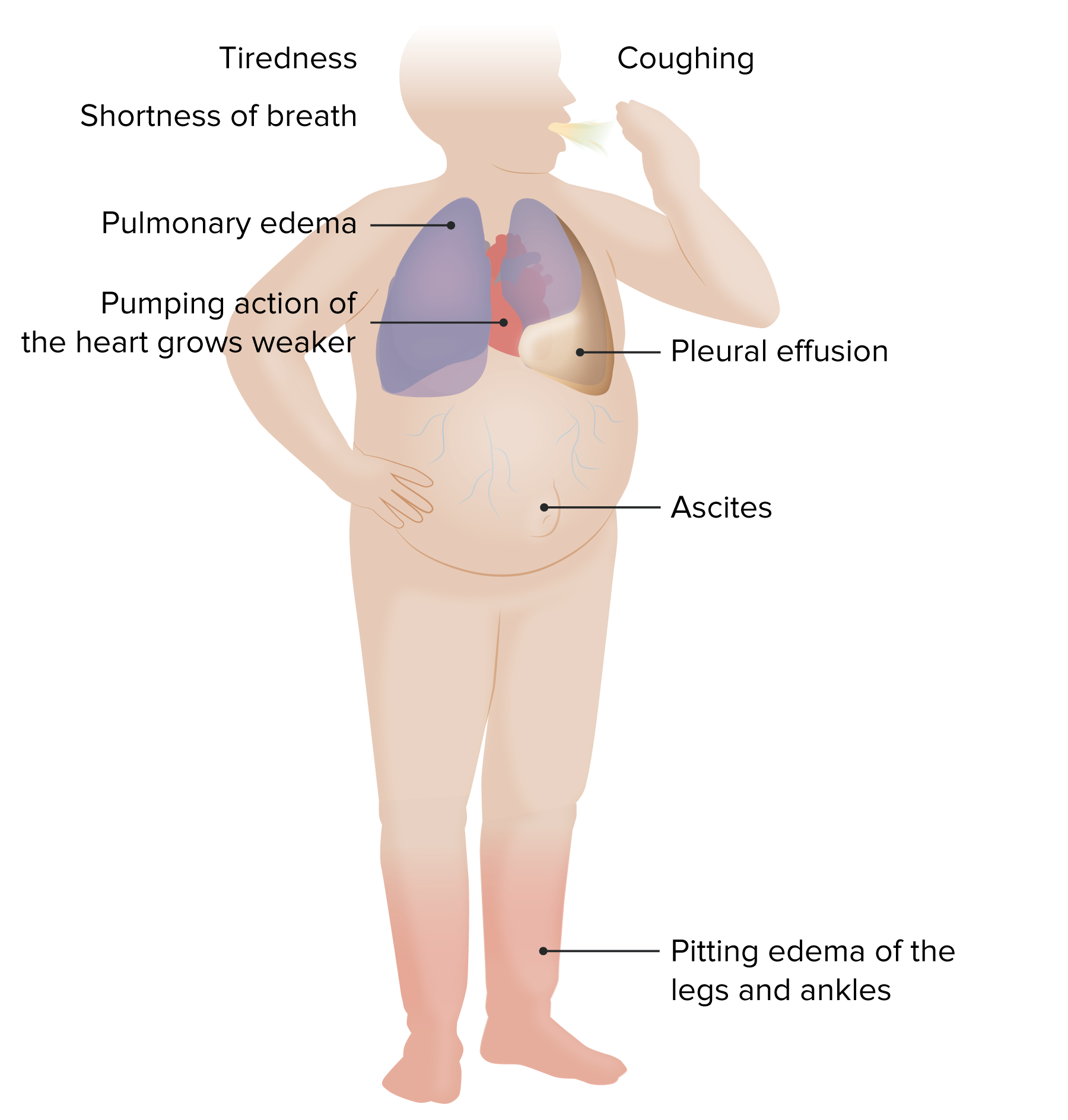
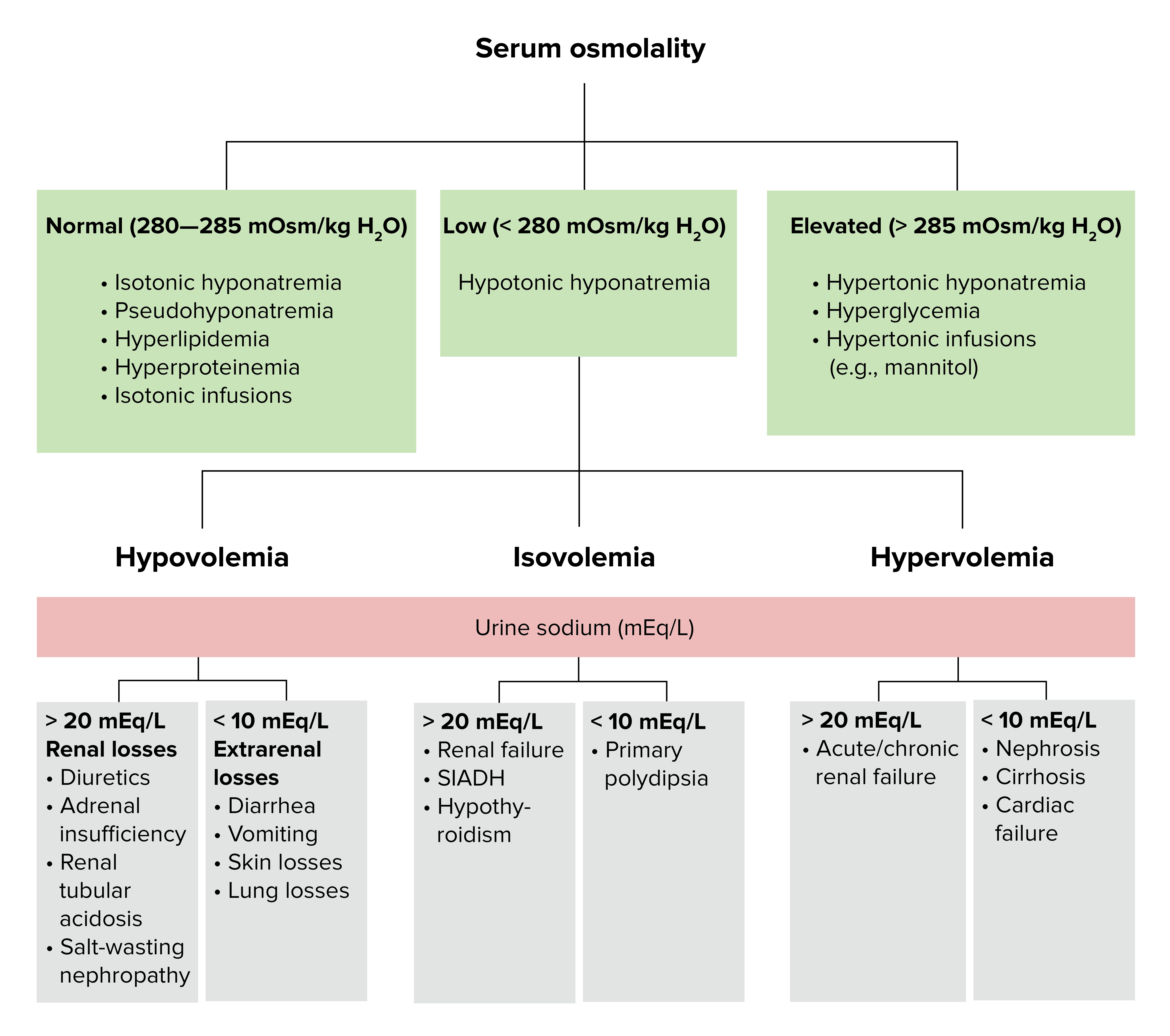
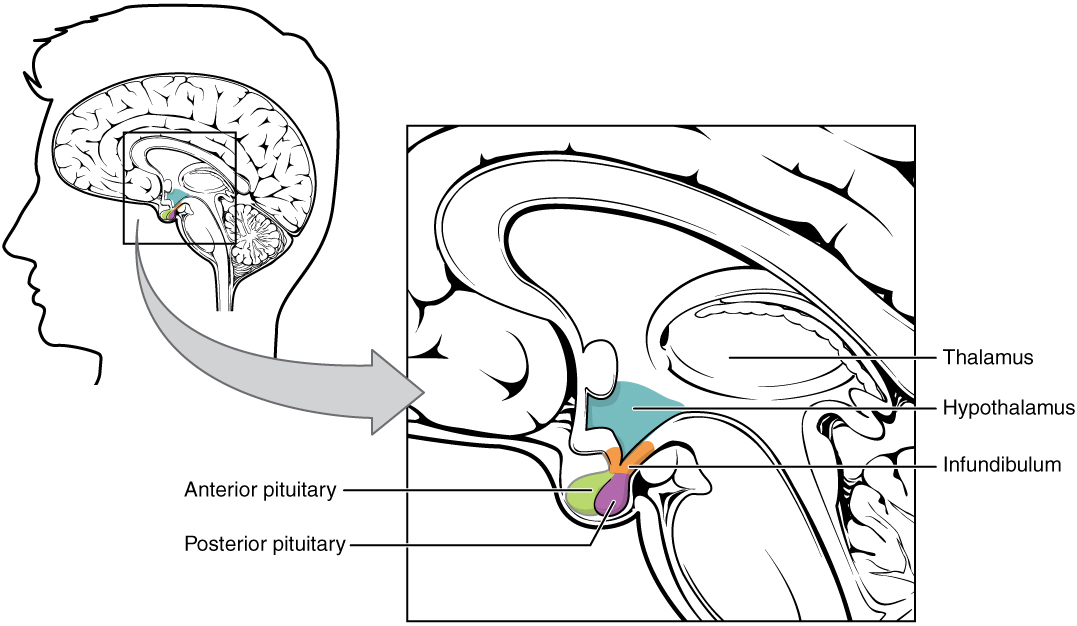
00:00 Let’s take a look at important arginine vasopressin differential diagnoses. 00:04 Once you’ve understood all of different topics that we covered up above, you go to this table and you take a look at the labs so that you’re able to clearly and quickly differentiate one pathology from the other. 00:17 And not all these are pathology. 00:18 Some of these are pathophysiologic point. 00:20 For example, water deprivation. 00:22 Close your eyes. 00:23 The water deprivation, what’s your plasma osmolarity? Increased. 00:26 What’s your urine osmolarity? Increased. 00:29 Water deprivation. 00:31 Osmoreceptors of hypothalamus. 00:32 You tell me. 00:33 Stimulated, ADH comes out. 00:36 Therefore, you can expect your serum ADH to be increased. 00:40 First column. 00:41 You tell me about plasma urine osmolality. 00:44 Done. 00:45 Flow rate – obviously, low because you’re reabsorbing water. 00:47 Next. 00:48 That’s a concept. 00:50 If there’s ADH, what you’re doing to free water? You’re reabsorbing it. 00:54 So, therefore, how much free water are you clearing? Negative. 01:00 SIADH. 01:02 Give me some reasons. 01:04 Neurosurgery, transsphenoidal. 01:06 You might be releasing too much ADH. 01:09 Maybe there’s lung disease. 01:10 What kind? Maybe pneumonia, maybe there’s thoracic surgery or maybe lung cancer such as small-cell. 01:18 Whatever the reason, increased serum ADH abundantly. 01:21 We know about plasma and urine and we know about flow rate and there’s your clearance of free water. 01:26 Then we have water drinking. 01:30 If you’re drinking water or let’s say that you have primary polydipsia and you’re drinking water too much, excessively. 01:36 Here, things are different, aren’t they? You’re going to inhibit the release of ADH – decreased. 01:42 Your plasma osmolarity will be low. 01:46 Urine osmolarity is going to be extremely... well, if you’re drinking plenty of water, it will be hypoosmotic. 01:54 The flow rate will be incredibly high and the amount of water that you’re now clearing, in terms of free water, will be excessive. 02:01 So, therefore, this will be positive. 02:07 Other differentials. 02:09 Central diabetes insipidus. 02:11 Give me some causes. 02:12 Trauma, triphasic. 02:15 Eventually during transsphenoidal surgery, you may result in complete ablation of ADH. 02:22 Or we talked about infiltrative such as Langerhans cell histiocytosis. 02:26 Here you have decreased ADH. 02:28 Tell me about your urine. 02:32 Hypoosmotic. 02:33 Tell me about plasma osmolarity. 02:35 It will be hypersmotic. 02:37 Flow rate will be high. 02:39 Clearance of free water, if ADH is not present, will be positive. 02:43 If it’s nephrogenic, just to make sure we’re clear here, receptors aren’t working properly. 02:50 Your urine will be diluted, hypoosmotic. 02:54 High flow rate. 02:55 Positive clearance of free water. 02:57 If the receptor, for whatever reason, is not working maybe due to demeclocycline or lithium or the V2 receptors are congenitally not functioning, this is nephrogenic diabetes insipidus. 03:10 Your ADH levels will be really high, but the receptors aren’t working properly. 03:15 Keep that in mind. 03:18 Let’s talk about hyponatremia and the different, different types of hyponatremia. 03:26 You can have hypovolemic, euvolemic, hypervolemic. 03:29 I want you to really pause here for a second. 03:34 Take a look at the entire picture of this algorithm. 03:37 My topic is hyponatremia. 03:40 If it’s hyponatremia, the patient has decreased plasma sodium. 03:47 But, you can have different amounts of volume and still result in hyponatremia. 03:54 What does that mean? You could be hypovolemic, hypervolemic or euvolemic hyponatremic. 04:02 Then this gives you important differentials. 04:04 Let’s take a look at our first branch of the algorithm for hyponatremia and we have hypovolemia. 04:10 Examples: vomiting and diarrhoea. 04:13 Here, the patient is hypovolemic and also hyponatremic. 04:19 Overall picture of this slide is hyponatremia. 04:22 Let’s talk about euvolemia. 04:26 You rule out adrenal, adrenal insufficiency and you rule out hypothyroidism then you have SIADH. 04:36 This patient is euvolemic. 04:37 So, even though there is going to be hyponatremia and increased amounts of fluid in your patient, we still call this patient euvolemic. 04:46 Is that important? Yes, clinically it is. 04:49 That’s why you’re paying attention to that point. 04:52 In hypervolemic, you have renal failure, you have congest-congestive heart failure or you have cirrhosis. 04:59 In all three instances, you’re going to accumulate volume – hypervolemia. 05:06 In all three instances with renal failure, we can talk about this as being nephrotic syndrome perhaps or renal failure itself, in which you are then retaining fluid with sodium. 05:17 Think about right-sided heart failure, think about cirrhosis with decreased albumin or nephrotic syndrome with decreased albumin. 05:28 These patients are hypervolemic, hyponatremia. 05:32 In this section, we’re looking at two hormones of the posterior pituitary. 05:37 One of the great detail about ADH, oxytocin, a much simpler hormone to deal with. 05:44 Oxytocin, wherever it functions, take look at the picture, we have the uterus and we have the myoepithelial cells of the breast. 05:51 Wherever it functions, either the uterus or the breast, we’re talking about positive feedback in which is responsible for contraction, contraction, contraction. 06:00 A simple question that you want to keep in mind would be, well, if it’s contraction, then what is the G protein that you’re referring to? Gq, right? Gq. 06:10 Contraction. 06:11 Oxytocin responsible for contraction of uterus so that you deliver the child and then also during suckling by an infant, with the mother you’re going to then eject milk. 06:23 It’s synthetized where? Paraventricular nuclei of the hypothalamus. 06:29 In fact, both posterior pituitary hormones are synthetized in hypothalamus. 06:36 It is then bound to neurophysin, brought into the posterior pituitary. 06:39 It’s important in parturition, meaning to say stimulation of the uterus and then with breast feeding with milk feeding. 06:50 Oxytocin – both circumstances, positive feedback. 06:53 Uterine contraction promotes uterine stretch. 06:56 Remember though that oxytocin and prostaglandin work in tandem so that you’re able to properly deliver your child. 07:04 The breast, specifically, histology here is the myoepithelial cells, as you see in the image. 07:10 Oxytocin used intravenously to induce or reinforce the labour. 07:16 And we have a drug called Atosiban, oxytocin receptor antagonist, used as a tocolytic in preterm labour. 07:25 Keep that in mind, please. 07:26 With slowing down contractions as being a major, major concept with oxytocin. 07:34 Ultimately, ADH and oxytocin management summary is what we’re looking at. 07:40 From the posterior pituitary, we have oxytocin. 07:44 With oxytocin, we have it at being a agonist to induce labour–welcome to Pitocin treatment indications. 07:55 Treatment indications or oxytocin in which you’re trying to slow down contraction. 08:03 The term here tocolytic. 08:06 You’re trying to lys the contraction, tocolytic. 08:11 The drug here, once again, Atosiban. 08:14 You want to try to slow down preterm labour, big time. 08:19 Now, on the other side, we have vasopressin and ADH. 08:23 Maybe perhaps you want to have agonist action. 08:27 Welcome to... remember, arginine, desmopressin, central diabetes inspidus. 08:33 Think about that patient in which, upon administration of desmopressin, you would then find urine osmolarity to then increase. 08:42 Antagonist, you remember that patient with SIADH? Would you tell me the steps of management? Number one, restrict free water use or consumption. 08:55 Number two, you want to crack that sodium maybe perhaps by giving? Good, IV fluids. 09:02 Next, you want to try to get rid of the excess fluid, so you give a loop diuretic, but once again, make sure that you keep an eye on that sodium because your patient is severely in a state of hyponatremia. 09:15 Maybe perhaps you want to block your V2 receptors. 09:16 Welcome to Conivaptan (IV administration), Tolvaptan (p.o. administration). 09:23 If your disease or your pathology still seems refractory, you want to start thinking about maybe injuring your V2 receptors on purpose. 09:33 Welcome to drugs such as demeclocycline or lithium.
About the Lecture
The lecture Arginine Vasopressin (AVP) Differential Diagnoses by Carlo Raj, MD is from the course Pituitary Gland Disorders.
Included Quiz Questions
What is the most likely diagnosis in a patient with high serum levels of antidiuretic hormone, hypoosmotic urine, and high plasma osmolarity?
- Nephrogenic diabetes insipidus
- Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
- Central diabetes insipidus
- Primary polydipsia
- Dehydration
Which cause of hyponatremia is most likely to present with hypervolemia?
- Congestive heart failure
- Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
- Addison's disease
- Hypothyroidism
- Paraneoplastic syndrome
Which change is most likely with ADH antagonism?
- Decrease in urine osmolarity
- Decrease in plasma osmolarity
- Increase in water reabsorption
- Decrease in serum sodium concentration
- Increase in interstitial fluid volume
What statement is false regarding oxytocin?
- It binds to its target receptor within the cytoplasm.
- It is synthesized in paraventricular nuclei of the hypothalamus.
- It is stored in the posterior pituitary.
- It stimulates Gq receptors.
- It activates a positive feedback response.
What is the mechanism of action of atosiban?
- Selective oxytocin-vasopressin receptor antagonist
- Synthetic form of oxytocin
- Promoter of breast myoepithelial contractions
- Stimulator of vasopressin receptor 2
- Stimulator of vasopressin receptor 1
Which condition maintains a high level of serum antidiuretic hormone despite a euvolemic state?
- SIADH
- Dehydration
- Nephrogenic diabetes insipidus
- Primary polydipsia
- Central diabetes insipidus
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |